Introduction
Some countries, including the United States, Canada, and Australia, require that prospective visitors seeking immigration, marriage, study, employment, working-holiday, or other visas must undergo a medical examination in a designated hospital. Identification of active tuberculosis (TB) cases is vital because the incidence thereof is much higher in South Korea (86.0 per 10
5 of the population) than in the United States (3.1 per 10
5 of the population), Canada (5.2 per 10
5 of the population), and Australia (6.4 per 10
5 of the population) in 2014
1.
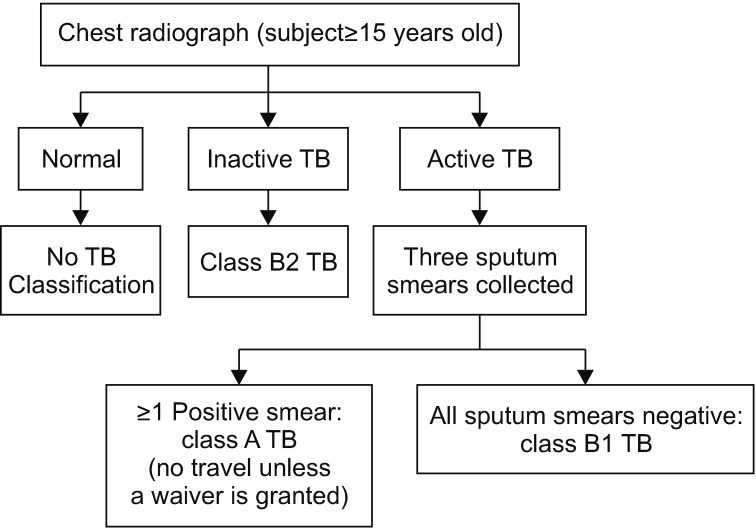
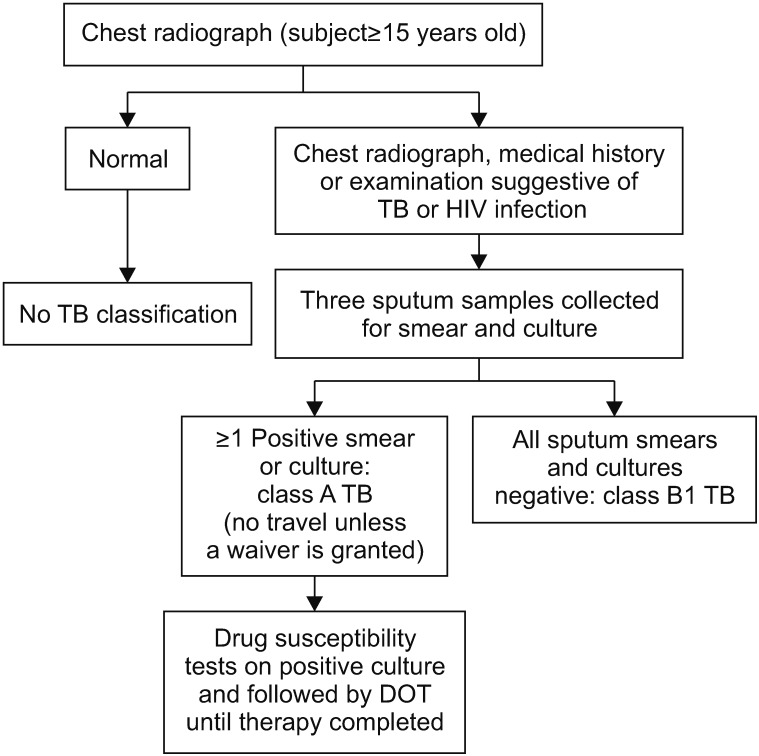
In 1991, the U.S. Centers for Disease Control and Prevention (CDC) drafted a technical instruction (TI) for TB screening and treatment of visa applicants; this TI featured chest radiography (CXR) and three consecutive acid-fast bacilli (AFB) smear tests on sputum if the CXR results were suggestive of TB. Although since 1991, the U.S. CDC TI for overseas TB screening has stipulated three consecutive AFB smear tests after an abnormal CXR, transmission of TB from AFB smear-negative patients remains important because of the relatively low predictive value of these tests. In 2007, the U.S. CDC expanded the TI to include three consecutive Mycobacterium tuberculosis (MTB) cultures of sputum in addition to the smear tests and mandated drug susceptibility testing (DST) and directly observed therapy (DOT) for those undergoing TB treatment (Culture and Directly Observed Therapy [CDOT] TB TI). Although some differences in the age of the subjects exist, the visa programs of many countries, including Canada, Australia, New Zealand, and the United States, follow the revised TI of the U.S. CDC.
The prevalence of smear- and/or culture-positive TB has diminished noticeably according to the nationwide Korean TB surveys that were conducted every 5 years from 1965 (940 per 10
5 of the population) to 1995 (219 per 10
5 of the population)
2. The Korean Tuberculosis Surveillance System (KTBS), an internet-based system of case notification, was adopted in 2000, but this system has been criticized. Notification of TB cases, especially by private institutions, may be neglected or incomplete, which could lead to an underestimation of the TB burden
3.
We compared the incidence of TB among visa applicants screened using the culture-based protocol with that determined using the smear-based protocol. Additionally, we indirectly estimated the status of TB in South Korea from the number of cases of active TB identified in medical screening examinations of visa applicants.
Go to :

Results
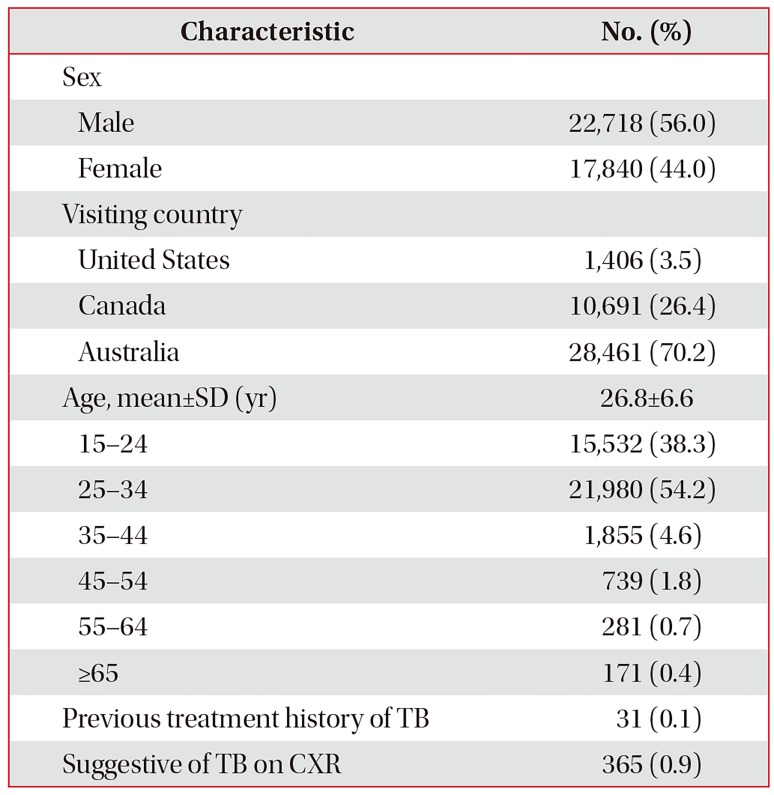
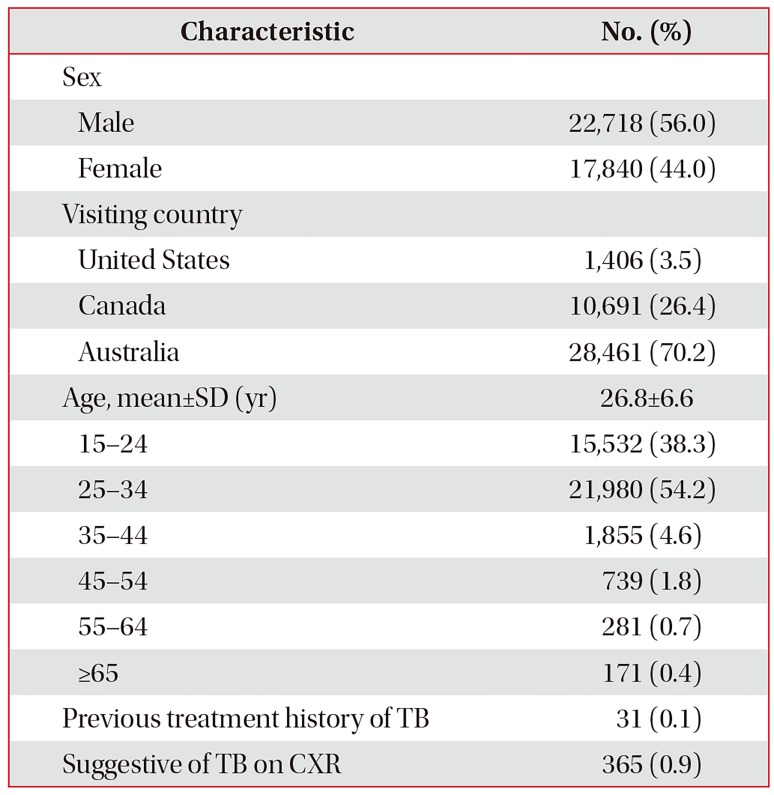
Among the 43,488 applicants, we excluded those under 15 years of age (n=444) who did not take CXR according to the U.S. CDC protocol, as well as foreigners (n=592). Applicants who visited several times because of repeat visits to one country or visits to several countries (n=1,887) were counted only once. Finally, we evaluated 40,558 subjects. The average age (±SD) of the population was 26.8 (±6.6) years; 21,980 (54.2%) were aged 25–34 years, 15,532 (38.3%) were 15–24 years, with those of younger age (15–34 years) constituting 90% of the population. Thirty-one applicants stated that they had previously undergone treatment for TB. Abnormal CXR results suggestive of either inactive or active TB were obtained from 365 subjects (0.9%, 899.9 per 10
5 of the population) (
Table 1).
Table 1
General characteristics of the study population (n=40,558)
|
Characteristic |
No. (%) |
|
Sex |
|
|
Male |
22,718 (56.0) |
|
Female |
17,840 (44.0) |
|
Visiting country |
|
|
United States |
1,406 (3.5) |
|
Canada |
10,691 (26.4) |
|
Australia |
28,461 (70.2) |
|
Age, mean±SD (yr) |
26.8±6.6 |
|
15–24 |
15,532 (38.3) |
|
25–34 |
21,980 (54.2) |
|
35–44 |
1,855 (4.6) |
|
45–54 |
739 (1.8) |
|
55–64 |
281 (0.7) |
|
≥65 |
171 (0.4) |
|
Previous treatment history of TB |
31 (0.1) |
|
Suggestive of TB on CXR |
365 (0.9) |

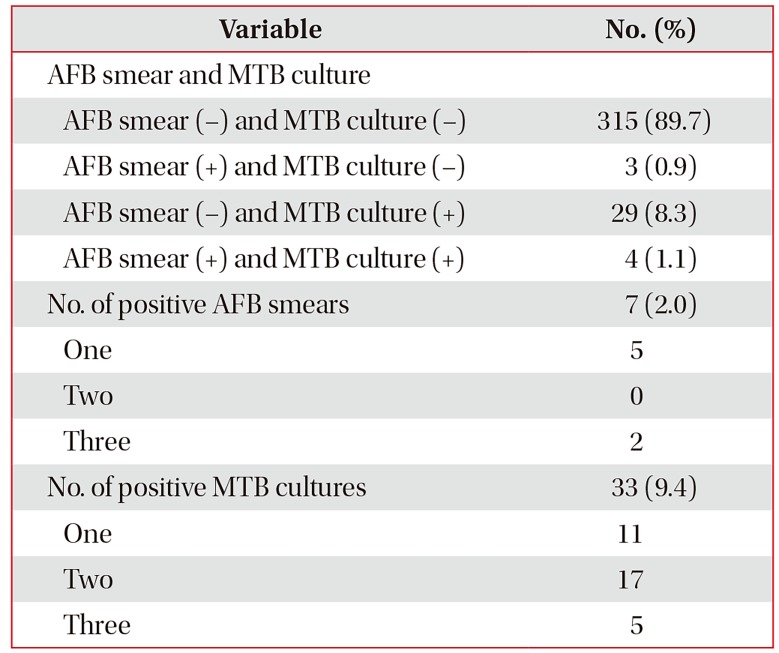
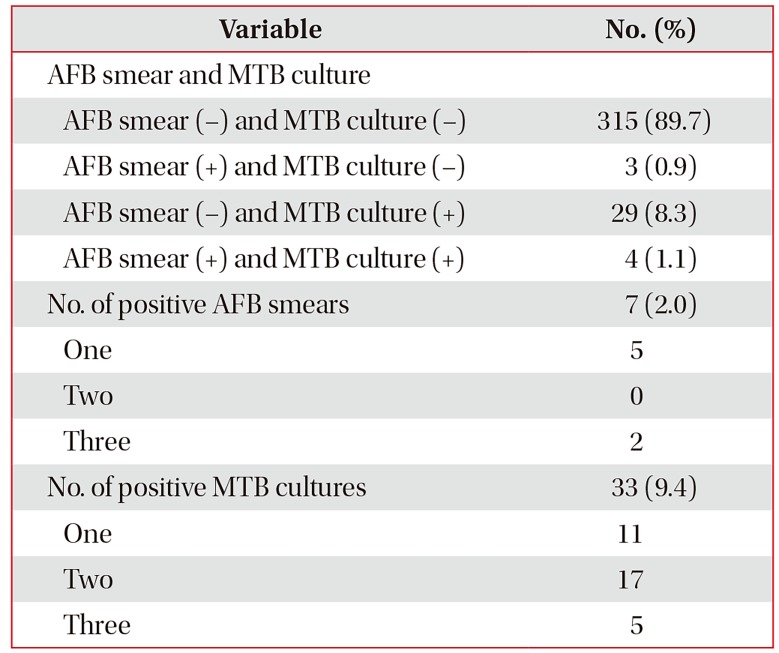
Fourteen subjects refused further sputum examinations, and 351 underwent three sputum AFB smear tests and MTB cultures. Seven subjects had at least one positive smear test and 33 at least one positive MTB culture. Twenty-nine subjects were negative on the AFB smear tests but positive on the culture tests. One positive sputum test was associated with a positive MTB culture in 11 cases, two sputum tests were associated with positive cultures in 17 cases, and all three sputum tests were positive in five cases, together with positive culture data (
Table 2).
Table 2
Sputum test results of those with abnormal chest radiographs (n=351)
|
Variable |
No. (%) |
|
AFB smear and MTB culture |
|
|
AFB smear (−) and MTB culture (−) |
315 (89.7) |
|
AFB smear (+) and MTB culture (−) |
3 (0.9) |
|
AFB smear (−) and MTB culture (+) |
29 (8.3) |
|
AFB smear (+) and MTB culture (+) |
4 (1.1) |
|
No. of positive AFB smears |
7 (2.0) |
|
One |
5 |
|
Two |
0 |
|
Three |
2 |
|
No. of positive MTB cultures |
33 (9.4) |
|
One |
11 |
|
Two |
17 |
|
Three |
5 |

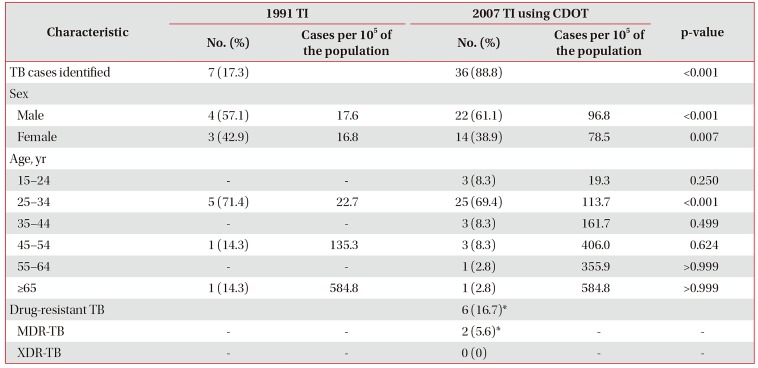
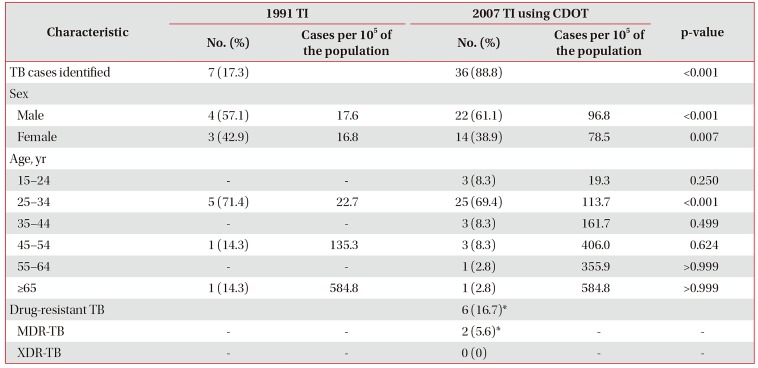
TB was identified in 36 subjects (88.8 per 105 of the population) using the CDOT TB TI but in only seven using the 1991 U.S. CDC TI (p<0.001). When evaluated by sex, 22 males (96.8 per 10
5 of the population) and 14 females (78.5 per 10
5 of the population) were classified with TB using the 2007 TI, but only four males and three females were classified with TB using the 1991 TI; these differences were statistically significant (p<0.001 and p=0.007, respectively). Six cases were resistant to at least one TB drug (16.7%), and two were MDR-TB (5.6%) according to the CDOT TB TI (
Table 3).
Table 3
Characteristics of the TB cases identified using different technical instructions
|
Characteristic |
1991 TI |
2007 TI using CDOT |
p-value |
|
No. (%) |
Cases per 105 of the population |
No. (%) |
Cases per 105 of the population |
|
TB cases identified |
7 (17.3) |
|
36 (88.8) |
|
<0.001 |
|
Sex |
|
|
|
|
|
|
Male |
4 (57.1) |
17.6 |
22 (61.1) |
96.8 |
<0.001 |
|
Female |
3 (42.9) |
16.8 |
14 (38.9) |
78.5 |
0.007 |
|
Age, yr |
|
|
|
|
|
|
15–24 |
- |
- |
3 (8.3) |
19.3 |
0.250 |
|
25–34 |
5 (71.4) |
22.7 |
25 (69.4) |
113.7 |
<0.001 |
|
35–44 |
- |
- |
3 (8.3) |
161.7 |
0.499 |
|
45–54 |
1 (14.3) |
135.3 |
3 (8.3) |
406.0 |
0.624 |
|
55–64 |
- |
- |
1 (2.8) |
355.9 |
>0.999 |
|
≥65 |
1 (14.3) |
584.8 |
1 (2.8) |
584.8 |
>0.999 |
|
Drug-resistant TB |
|
|
6 (16.7)*
|
|
|
|
MDR-TB |
- |
- |
2 (5.6)*
|
- |
- |
|
XDR-TB |
- |
- |
0 (0) |
- |
- |

Go to :

Discussion
In total, 36 cases of TB were detected in visa applicants using the CDOT TB TI (88.8 per 105 of the population). The incidence was found to be already high in younger subjects (118.3 per 105 of the population aged 25–34 years) and to increase with age. When the older smear-based U.S. CDC TI was used, only seven applicants were classified as having TB; thus, 29 positive TB cases (80.6%) were missed when the older TI was used.
The prevalence of TB in South Korea has decreased with an improving economy, but TB control remains unsatisfactory
8. A public health problem is evident. The incidence of TB (86 per 10
5 of the population) is the highest among the 34 countries of the Organization for Economic Cooperation and Development (OECD) in 2014; the average TB incidence in the other 33 OECD countries was only 9.76 per 10
5 of the population in 2014
1. In the United States from 2001 to 2008, South Koreans accounted for 8.1% of all estimated TB cases among newly arrived students/exchange visitors and for 6.2% of TB cases among newly arrived tourists and business travelers, ranking as the fourth and seventh most significant sources of infection, respectively
9.
Immigration has been an important cause of TB in high-income countries. In the United States, for example, 64% of new TB cases in 2013 were attributable to infections spread from foreign-born subjects
10. The U.S. CDC conducted a preliminary study on the effectiveness of pre-immigration TB screening programs in Vietnam among 1,179 U.S.-bound immigrants with abnormal CXRs; positive AFB smear results were detected in 82 (7.0%) immigrants, positive MTB culture results in 183 (15.5%), and negative smear but positive culture results in 120 (10.2%)
11. Follow-up evaluation from 1999 to 2005 revealed that 7.0% of smear-negative TB immigrants were diagnosed with active TB after arrival in the United States
12. A DNA fingerprinting study performed in the United States showed that at least 17% of TB patients had been infected by smear-negative patients; the relative TB transmission rate from smear-negative to smear-positive patients was found to be 0.22 (95% confidence interval, 0.16–0.32)
13.
The AFB smear test has a sensitivity of about 53%. A second specimen increases this to 64.4% and a third specimen increases this to 66.4%–69.4%
14. This is because 5,000–10,000 AFB per microliter sputum sample are required for a positive result
15, compared to 10–100 AFB per microliter for a sputum culture
16, which has a sensitivity of 80%–85% and specificity of about 98%
171819. The low sensitivity of the AFB smear test is also attributable to differences in staining technique, centrifugation speed, reader experience, and the TB prevalence in the population (30%–80%)
1720. In this study, the culture test identified 33 TB cases, compared to seven for the AFB smear test.
After implementation of culture-based TB screening in subjects from countries with a high TB burden in 2007, the annual number of TB cases diagnosed within 1 year of arrival among foreign-born subjects decreased steadily from 1,326 to 940 (2008–2012) compared with the 1,424–1,626 (mean 1,504) cases (2002–2007) diagnosed prior to implementation of the new TI. Concomitantly, the incidence of smear-negative culture-positive cases increased from 178 (42.4%) in 2008 to 629 (59.5%) in 2012
21. Approximately 60% of immigrants and refugees with TB had negative smear results but positive culture results, according to the U.S. CDC
22. The enhanced screening program reduced the occurrence of TB within 6 months of arrival in the United States from 86 of 2,049 subjects (4.2%) (preintervention; applying the 1991 TI) to 22 of 1,430 subjects (1.5%) post-intervention (applying the new 2007 TI)
23. In the present study, 29 of 36 cases (80.5%) were smear-negative but culture-positive using the 2007 TI, whereas only seven were diagnosed with TB using the 1991 TI.
Drug-resistant TB was not uncommon in this study. DST is included in the enhanced TI to identify drug-resistant TB cases and to treat MDR-TB. In a four-round Korean study on national drug resistance conducted from 1994 to 2004, the prevalence of anti-TB drug resistance increased steadily from 11.3% to 12.8% and that of MDR from 1.6% to 2.7% of new cases and 27.5% to 14.0% of previously treated cases, respectively
24. In a previous Korean study, 5.8% of new cases and 20.1% of previously treated cases had MDR-TB
25. Another study in South Korea reported that 6.8% of total TB cases were MDR-TB, and 12.4% of these were XDR-TB
26. In this study, six of the 36 patients (16.7%) diagnosed with TB were resistant to at least one anti-TB drug, and two (5.6%) had MDR-TB and it was consistent with previous study.
Host immunity against MTB declines with age
27. We found that the number of TB cases per 10
5 of the population increased with age. A high prevalence of latent TB and TB re-activation may explain this finding. However, the high incidence of TB even in younger subjects suggests that TB remains infectious and is spreading among the young in South Korea. The incidence of TB in this study was 88.8 per 10
5 of the population, which is lower than the 89.6 per 10
5 of the population in the 2013 KTBS annual report of TB in Korea
28. The incidence of TB among subjects 25–34 years of age was greater in this work that in the 2013 report (113.78 vs. 76.4 per 10
5 of the population 25–29 years of age and 60.4 per 10
5 of the population 30–34 years of age, respectively). The difference between our findings and the KTBS report becomes greater with increasing age, with the exception of those 15–24 years of age (19.3 vs. 37.2 per 10
5 of the population 15–19 years of age and 62.7 per 10
5 of the population 20–24 years of age, respectively).
Much effort has focused on controlling TB in South Korea. The latent TB infection (LTBI) guidelines are reinforced in the revision of the 2014 Korean guidelines for TB because LTBI treatment is important for reducing the incidence of TB
29. Moreover, identification of active TB cases is also important for reducing the prevalence of TB.
This study had several limitations. First, it was performed in a single private hospital and was of a retrospective design, so the results are not representative of all visa applicants in South Korea. A multi-center prospective study would provide a clearer picture. Second, the study population consisted mostly of young subjects; less than 10% were over 35 years of age, possibly indicating selection bias. Third, AFB smear-positive and MTB culture-negative cases were common due to NTM or contamination of sputum. Fourth, most applicants refused to report their history of TB treatment to avoid further sputum tests; indeed, 14 applicants with CXR results suggestive of TB refused sputum tests. If these subjects had agreed to such testing, the TB frequency might have been higher.
The culture-based protocol identified a fivefold greater number of TB cases than the older smear-based protocol. TB screening tests, including consecutive sputum MTB culture tests, are essential for the diagnosis of, and epidemiological studies on, TB. The national TB control program needs to be enhanced, including by use of culture tests, if the prevalence of TB in South Korea is to be reduced.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download