|
1 |
Tuberculosis |
0.519 |
0.462 |
0.575 |
|
2 |
HIV disease resulting in mycobacterial infection |
0.746 |
0.694 |
0.792 |
|
3 |
HIV disease resulting in other specified or unspecified diseases |
0.787 |
0.740 |
0.828 |
|
4 |
Cholera |
0.355 |
0.298 |
0.415 |
|
5 |
Other salmonella infections |
0.279 |
0.229 |
0.334 |
|
6 |
Shigellosis |
0.248 |
0.198 |
0.303 |
|
7 |
Enteropathogenic E. coli infection |
0.290 |
0.236 |
0.347 |
|
8 |
Enterotoxigenic E. coli infection |
0.267 |
0.216 |
0.323 |
|
9 |
Campylobacter enteritis |
0.268 |
0.218 |
0.324 |
|
10 |
Amoebiasis |
0.380 |
0.321 |
0.440 |
|
11 |
Cryptosporidiosis |
0.518 |
0.459 |
0.577 |
|
12 |
Rotaviral enteritis |
0.188 |
0.146 |
0.236 |
|
13 |
Intestinal infection |
0.270 |
0.217 |
0.327 |
|
14 |
Typhoid and paratyphoid fevers |
0.382 |
0.322 |
0.445 |
|
15 |
Influenza |
0.149 |
0.112 |
0.194 |
|
16 |
Pneumococcal pneumonia |
0.427 |
0.369 |
0.486 |
|
17 |
H. influenzae type B pneumonia |
0.407 |
0.348 |
0.468 |
|
18 |
Respiratory syncytial virus pneumonia |
0.367 |
0.309 |
0.428 |
|
19 |
Upper respiratory infections |
0.131 |
0.096 |
0.173 |
|
20 |
Otitis media |
0.176 |
0.134 |
0.224 |
|
21 |
Pneumococcal meningitis |
0.590 |
0.532 |
0.645 |
|
22 |
H. influenzae type B meningitis |
0.557 |
0.498 |
0.614 |
|
23 |
Meningococcal infection |
0.530 |
0.470 |
0.588 |
|
24 |
Encephalitis |
0.687 |
0.632 |
0.737 |
|
25 |
Diphtheria |
0.340 |
0.284 |
0.398 |
|
26 |
Whooping cough |
0.253 |
0.203 |
0.307 |
|
27 |
Tetanus |
0.525 |
0.466 |
0.583 |
|
28 |
Measles |
0.254 |
0.203 |
0.312 |
|
29 |
Varicella |
0.241 |
0.193 |
0.293 |
|
30 |
Malaria |
0.438 |
0.381 |
0.497 |
|
31 |
Chagas disease |
0.547 |
0.489 |
0.604 |
|
32 |
Leishmaniasis |
0.408 |
0.350 |
0.467 |
|
33 |
African trypanosomiasis |
0.432 |
0.376 |
0.490 |
|
34 |
Schistosomiasis |
0.381 |
0.323 |
0.442 |
|
35 |
Cysticercosis |
0.372 |
0.316 |
0.431 |
|
36 |
Echinococcosis |
0.412 |
0.354 |
0.471 |
|
37 |
Lymphatic filariasis |
0.418 |
0.359 |
0.479 |
|
38 |
Onchocerciasis |
0.319 |
0.264 |
0.378 |
|
39 |
Trachoma |
0.437 |
0.376 |
0.498 |
|
40 |
Dengue |
0.395 |
0.337 |
0.455 |
|
41 |
Yellow fever |
0.504 |
0.444 |
0.563 |
|
42 |
Rabies |
0.655 |
0.598 |
0.709 |
|
43 |
Ascariasis |
0.231 |
0.183 |
0.284 |
|
44 |
Trichuriasis |
0.253 |
0.202 |
0.309 |
|
45 |
Hookworm disease |
0.241 |
0.193 |
0.295 |
|
46 |
Food-borne trematodiases |
0.275 |
0.224 |
0.330 |
|
47 |
Tsutsugamushi fever |
0.386 |
0.329 |
0.445 |
|
48 |
Typhus fever |
0.390 |
0.332 |
0.449 |
|
49 |
Hantaan virus disease |
0.472 |
0.411 |
0.532 |
|
50 |
Intestinal helminth |
0.267 |
0.217 |
0.321 |
|
51 |
Maternal hemorrhage |
0.514 |
0.453 |
0.575 |
|
52 |
Maternal sepsis |
0.749 |
0.699 |
0.795 |
|
53 |
Hypertensive disorders of pregnancy |
0.455 |
0.395 |
0.516 |
|
54 |
Obstructed labor |
0.462 |
0.404 |
0.521 |
|
55 |
Abortion |
0.300 |
0.245 |
0.359 |
|
56 |
Preterm birth complications |
0.517 |
0.456 |
0.576 |
|
57 |
Neonatal encephalopathy (birth asphyxia and birth trauma) |
0.858 |
0.815 |
0.893 |
|
58 |
Sepsis and other infectious disorders of the newborn baby |
0.711 |
0.658 |
0.759 |
|
59 |
Protein-energy malnutrition |
0.414 |
0.356 |
0.474 |
|
60 |
Iodine deficiency |
0.200 |
0.155 |
0.250 |
|
61 |
Vitamin A deficiency |
0.153 |
0.115 |
0.197 |
|
62 |
Iron-deficiency anemia |
0.170 |
0.131 |
0.216 |
|
63 |
Syphilis |
0.452 |
0.393 |
0.511 |
|
64 |
Sexually transmitted chlamydial diseases |
0.253 |
0.205 |
0.307 |
|
65 |
Gonococcal infection |
0.307 |
0.255 |
0.364 |
|
66 |
Trichomoniasis |
0.316 |
0.259 |
0.377 |
|
67 |
Herpes genitalia |
0.286 |
0.231 |
0.345 |
|
68 |
Acute hepatitis A |
0.364 |
0.307 |
0.424 |
|
69 |
Acute hepatitis B |
0.431 |
0.372 |
0.491 |
|
70 |
Acute hepatitis C |
0.501 |
0.441 |
0.561 |
|
71 |
Acute hepatitis E |
0.467 |
0.407 |
0.526 |
|
72 |
Leprosy |
0.613 |
0.558 |
0.665 |
|
73 |
Legionnaires' disease |
0.345 |
0.288 |
0.405 |
|
74 |
Leptospirosis |
0.415 |
0.355 |
0.475 |
|
75 |
Rubella |
0.359 |
0.301 |
0.418 |
|
76 |
Mumps |
0.202 |
0.157 |
0.253 |
|
77 |
Esophageal cancer |
0.841 |
0.802 |
0.875 |
|
78 |
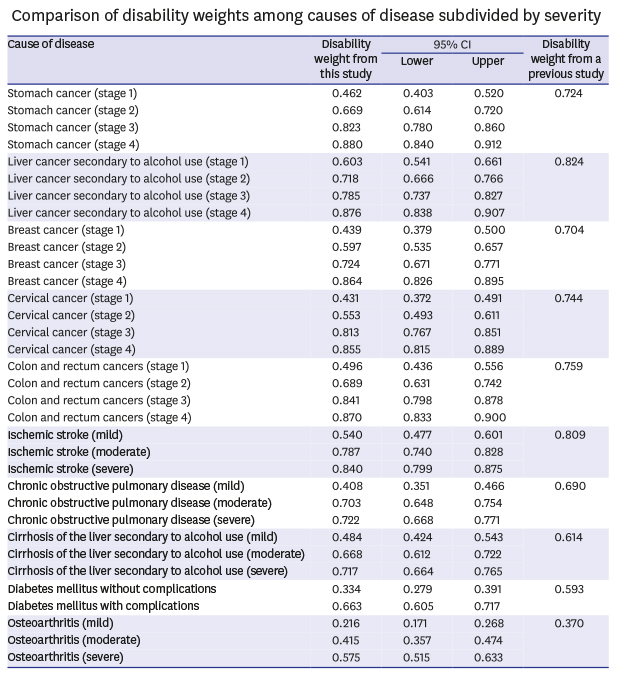
Stomach cancer (stage 1) |
0.462 |
0.403 |
0.520 |
|
79 |
Stomach cancer (stage 2) |
0.669 |
0.614 |
0.720 |
|
80 |
Stomach cancer (stage 3) |
0.823 |
0.780 |
0.860 |
|
81 |
Stomach cancer (stage 4) |
0.880 |
0.840 |
0.912 |
|
82 |
Liver cancer secondary to hepatitis B |
0.796 |
0.749 |
0.837 |
|
83 |
Liver cancer secondary to hepatitis C |
0.802 |
0.755 |
0.842 |
|
84 |
Liver cancer secondary to alcohol use (stage 1) |
0.603 |
0.541 |
0.661 |
|
85 |
Liver cancer secondary to alcohol use (stage 2) |
0.718 |
0.666 |
0.766 |
|
86 |
Liver cancer secondary to alcohol use (stage 3) |
0.785 |
0.737 |
0.827 |
|
87 |
Liver cancer secondary to alcohol use (stage 4) |
0.876 |
0.838 |
0.907 |
|
88 |
Larynx cancer |
0.824 |
0.784 |
0.859 |
|
89 |
Trachea, bronchus and lung cancers (stage 1) |
0.600 |
0.542 |
0.656 |
|
90 |
Trachea, bronchus and lung cancers (stage 2) |
0.738 |
0.686 |
0.785 |
|
91 |
Trachea, bronchus and lung cancers (stage 3) |
0.758 |
0.710 |
0.801 |
|
92 |
Trachea, bronchus and lung cancers (stage 4) |
0.906 |
0.873 |
0.932 |
|
93 |
Breast cancer (stage 1) |
0.439 |
0.379 |
0.500 |
|
94 |
Breast cancer (stage 2) |
0.597 |
0.535 |
0.657 |
|
95 |
Breast cancer (stage 3) |
0.724 |
0.671 |
0.771 |
|
96 |
Breast cancer (stage 4) |
0.864 |
0.826 |
0.895 |
|
97 |
Cervical cancer (stage 1) |
0.431 |
0.372 |
0.491 |
|
98 |
Cervical cancer (stage 2) |
0.553 |
0.493 |
0.611 |
|
99 |
Cervical cancer (stage 3) |
0.813 |
0.767 |
0.851 |
|
100 |
Cervical cancer (stage 4) |
0.855 |
0.815 |
0.889 |
|
101 |
Uterine cancer |
0.711 |
0.661 |
0.757 |
|
102 |
Prostate cancer (stage 1) |
0.458 |
0.399 |
0.518 |
|
103 |
Prostate cancer (stage 2) |
0.613 |
0.552 |
0.672 |
|
104 |
Prostate cancer (stage 3) |
0.742 |
0.692 |
0.787 |
|
105 |
Prostate cancer (stage 4) |
0.838 |
0.795 |
0.874 |
|
106 |
Colon and rectum cancers (stage 1) |
0.496 |
0.436 |
0.556 |
|
107 |
Colon and rectum cancers (stage 2) |
0.689 |
0.631 |
0.742 |
|
108 |
Colon and rectum cancers (stage 3) |
0.841 |
0.798 |
0.878 |
|
109 |
Colon and rectum cancers (stage 4) |
0.870 |
0.833 |
0.900 |
|
110 |
Mouth cancer |
0.870 |
0.828 |
0.905 |
|
111 |
Nasopharynx cancer |
0.766 |
0.716 |
0.811 |
|
112 |
Cancer of other part of pharynx and oropharynx |
0.811 |
0.764 |
0.851 |
|
113 |
Gallbladder and biliary tract cancer |
0.800 |
0.752 |
0.843 |
|
114 |
Pancreatic cancer |
0.879 |
0.843 |
0.909 |
|
115 |
Malignant melanoma of skin |
0.786 |
0.737 |
0.829 |
|
116 |
Non-melanoma skin cancer |
0.649 |
0.593 |
0.702 |
|
117 |
Ovarian cancer |
0.776 |
0.727 |
0.821 |
|
118 |
Testicular cancer |
0.692 |
0.637 |
0.744 |
|
119 |
Kidney cancer (stage 1) |
0.570 |
0.509 |
0.627 |
|
120 |
Kidney cancer (stage 2) |
0.731 |
0.678 |
0.778 |
|
121 |
Kidney cancer (stage 3) |
0.809 |
0.762 |
0.849 |
|
122 |
Kidney cancer (stage 4) |
0.902 |
0.870 |
0.927 |
|
123 |
Other urinary organ cancers |
0.711 |
0.656 |
0.761 |
|
124 |
Bladder cancer (stage 1) |
0.500 |
0.441 |
0.558 |
|
125 |
Bladder cancer (stage 2) |
0.623 |
0.567 |
0.676 |
|
126 |
Bladder cancer (stage 3) |
0.769 |
0.720 |
0.812 |
|
127 |
Bladder cancer (stage 4) |
0.869 |
0.830 |
0.901 |
|
128 |
Brain and nervous system cancers |
0.888 |
0.852 |
0.918 |
|
129 |
Thyroid cancer (stage 1) |
0.301 |
0.248 |
0.359 |
|
130 |
Thyroid cancer (stage 2) |
0.484 |
0.425 |
0.543 |
|
131 |
Thyroid cancer (stage 3) |
0.639 |
0.583 |
0.691 |
|
132 |
Thyroid cancer (stage 4) |
0.779 |
0.730 |
0.822 |
|
133 |
Hodgkin's disease |
0.670 |
0.612 |
0.725 |
|
134 |
Non-Hodgkin lymphoma |
0.689 |
0.636 |
0.737 |
|
135 |
Multiple myeloma |
0.764 |
0.714 |
0.808 |
|
136 |
Leukemia |
0.812 |
0.765 |
0.854 |
|
137 |
Bone and connective tissue cancer |
0.765 |
0.717 |
0.809 |
|
138 |
Benign neoplasm of brain and other parts of central nervous system |
0.505 |
0.442 |
0.567 |
|
139 |
Rheumatic heart disease |
0.600 |
0.542 |
0.657 |
|
140 |
Ischemic heart disease |
0.534 |
0.475 |
0.592 |
|
141 |
Ischemic stroke (mild) |
0.540 |
0.477 |
0.601 |
|
142 |
Ischemic stroke (moderate) |
0.787 |
0.740 |
0.828 |
|
143 |
Ischemic stroke (severe) |
0.840 |
0.799 |
0.875 |
|
144 |
Hemorrhagic and other non-ischemic stroke |
0.785 |
0.738 |
0.825 |
|
145 |
Hypertensive heart disease |
0.502 |
0.444 |
0.560 |
|
146 |
Cardiomyopathy and myocarditis |
0.717 |
0.661 |
0.768 |
|
147 |
Atrial fibrillation and flutter |
0.584 |
0.526 |
0.641 |
|
148 |
Aortic aneurysm |
0.647 |
0.591 |
0.700 |
|
149 |
Peripheral vascular disease |
0.430 |
0.368 |
0.492 |
|
150 |
Endocarditis |
0.646 |
0.589 |
0.700 |
|
151 |
Hermorrhoid |
0.139 |
0.103 |
0.182 |
|
152 |
Varicose veins of lower extremities |
0.173 |
0.132 |
0.219 |
|
153 |
Chronic obstructive pulmonary disease (mild) |
0.408 |
0.351 |
0.466 |
|
154 |
Chronic obstructive pulmonary disease (moderate) |
0.703 |
0.648 |
0.754 |
|
155 |
Chronic obstructive pulmonary disease (severe) |
0.722 |
0.668 |
0.771 |
|
156 |
Pneumoconiosis |
0.669 |
0.614 |
0.721 |
|
157 |
Asthma |
0.396 |
0.337 |
0.458 |
|
158 |
Interstitial lung disease and pulmonary sarcoidosis |
0.678 |
0.623 |
0.729 |
|
159 |
Cirrhosis of the liver secondary to hepatitis B |
0.707 |
0.655 |
0.755 |
|
160 |
Cirrhosis of the liver secondary to hepatitis C |
0.706 |
0.653 |
0.754 |
|
161 |
Cirrhosis of the liver secondary to alcohol use (mild) |
0.484 |
0.424 |
0.543 |
|
162 |
Cirrhosis of the liver secondary to alcohol use (moderate) |
0.668 |
0.612 |
0.722 |
|
163 |
Cirrhosis of the liver secondary to alcohol use (severe) |
0.717 |
0.664 |
0.765 |
|
164 |
Peptic ulcer disease |
0.260 |
0.207 |
0.319 |
|
165 |
Gastritis and duodenitis |
0.144 |
0.107 |
0.187 |
|
166 |
Appendicitis |
0.245 |
0.196 |
0.300 |
|
167 |
Paralytic ileus and intestinal obstruction without hernia |
0.388 |
0.332 |
0.446 |
|
168 |
Inguinal or femoral hernia |
0.269 |
0.220 |
0.322 |
|
169 |
Crohn's disease |
0.597 |
0.538 |
0.653 |
|
170 |
Ulcerative colitis |
0.545 |
0.485 |
0.604 |
|
171 |
Vascular disorders of intestine |
0.515 |
0.455 |
0.573 |
|
172 |
Gallbladder and bile duct disease |
0.448 |
0.386 |
0.511 |
|
173 |
Pancreatitis |
0.498 |
0.436 |
0.559 |
|
174 |
Gastroesophageal reflux disease |
0.163 |
0.123 |
0.209 |
|
175 |
Alzheimer's disease and other dementias |
0.736 |
0.685 |
0.782 |
|
176 |
Parkinson's disease |
0.660 |
0.606 |
0.711 |
|
177 |
Epilepsy |
0.581 |
0.523 |
0.637 |
|
178 |
Multiple sclerosis |
0.693 |
0.640 |
0.742 |
|
179 |
Migraine |
0.190 |
0.148 |
0.237 |
|
180 |
Tension-type headache |
0.163 |
0.121 |
0.212 |
|
181 |
Schizophrenia |
0.666 |
0.612 |
0.717 |
|
182 |
Alcohol use disorders |
0.350 |
0.295 |
0.407 |
|
183 |
Opioid use disorders |
0.457 |
0.398 |
0.517 |
|
184 |
Cocaine use disorders |
0.459 |
0.401 |
0.518 |
|
185 |
Amphetamine use disorders |
0.473 |
0.413 |
0.534 |
|
186 |
Cannabis use disorders |
0.355 |
0.299 |
0.413 |
|
187 |
Major depressive disorder (mild) |
0.279 |
0.229 |
0.333 |
|
188 |
Major depressive disorder (moderate) |
0.528 |
0.469 |
0.586 |
|
189 |
Major depressive disorder (severe) |
0.569 |
0.509 |
0.627 |
|
190 |
Dysthymia |
0.188 |
0.145 |
0.238 |
|
191 |
Bipolar affective disorder |
0.483 |
0.424 |
0.542 |
|
192 |
Panic disorder |
0.391 |
0.335 |
0.448 |
|
193 |
Obsessive-compulsive disorder |
0.321 |
0.266 |
0.378 |
|
194 |
Post-traumatic stress disorder |
0.415 |
0.357 |
0.474 |
|
195 |
Anorexia nervosa |
0.420 |
0.363 |
0.478 |
|
196 |
Bulimia nervosa |
0.392 |
0.334 |
0.451 |
|
197 |
Autism |
0.510 |
0.449 |
0.570 |
|
198 |
Asperger's syndrome |
0.408 |
0.349 |
0.469 |
|
199 |
Attention-deficit hyperactivity disorder |
0.249 |
0.200 |
0.302 |
|
200 |
Conduct disorder |
0.275 |
0.224 |
0.331 |
|
201 |
Idiopathic intellectual disability |
0.483 |
0.422 |
0.543 |
|
202 |
Borderline personality disorder |
0.397 |
0.340 |
0.455 |
|
203 |
Diabetes mellitus without complications |
0.334 |
0.279 |
0.391 |
|
204 |
Diabetes mellitus with complications |
0.663 |
0.605 |
0.717 |
|
205 |
Acute glomerulonephritis |
0.420 |
0.362 |
0.480 |
|
206 |
Chronic kidney disease due to diabetes mellitus |
0.674 |
0.617 |
0.727 |
|
207 |
Chronic kidney disease due to hypertension |
0.594 |
0.534 |
0.652 |
|
208 |
Tubulointerstitial nephritis, pyelonephritis, and urinary tract infections |
0.359 |
0.302 |
0.418 |
|
209 |
Urolithiasis |
0.294 |
0.242 |
0.350 |
|
210 |
Benign prostatic hyperplasia |
0.207 |
0.161 |
0.259 |
|
211 |
Men infertility |
0.332 |
0.279 |
0.389 |
|
212 |
Urinary incontinence |
0.287 |
0.233 |
0.345 |
|
213 |
Uterine fibroids |
0.223 |
0.177 |
0.274 |
|
214 |
Polycystic ovarian syndrome |
0.399 |
0.342 |
0.458 |
|
215 |
Women infertility |
0.362 |
0.306 |
0.421 |
|
216 |
Endometriosis |
0.349 |
0.292 |
0.408 |
|
217 |
Genital prolapse |
0.404 |
0.338 |
0.471 |
|
218 |
Premenstrual syndrome |
0.136 |
0.101 |
0.179 |
|
219 |
Thalassemias |
0.485 |
0.425 |
0.545 |
|
220 |
Sickle cell disorders |
0.552 |
0.494 |
0.609 |
|
221 |
G6PD deficiency |
0.519 |
0.458 |
0.580 |
|
222 |
Rheumatoid arthritis |
0.451 |
0.392 |
0.510 |
|
223 |
Osteoarthritis (mild) |
0.216 |
0.171 |
0.268 |
|
224 |
Osteoarthritis (moderate) |
0.415 |
0.357 |
0.474 |
|
225 |
Osteoarthritis (severe) |
0.575 |
0.515 |
0.633 |
|
226 |
Low back pain (mild) |
0.138 |
0.101 |
0.181 |
|
227 |
Low back pain (moderate) |
0.310 |
0.257 |
0.368 |
|
228 |
Low back pain (severe) |
0.456 |
0.396 |
0.517 |
|
229 |
Neck pain |
0.133 |
0.097 |
0.177 |
|
230 |
Gout |
0.390 |
0.332 |
0.451 |
|
231 |
Systemic lupus erythematosus |
0.594 |
0.533 |
0.651 |
|
232 |
Neural tube defects |
0.782 |
0.734 |
0.825 |
|
233 |
Congenital heart anomalies |
0.679 |
0.622 |
0.731 |
|
234 |
Cleft lip and cleft palate |
0.313 |
0.258 |
0.372 |
|
235 |
Down's syndrome |
0.590 |
0.533 |
0.645 |
|
236 |
Eczema |
0.135 |
0.098 |
0.179 |
|
237 |
Psoriasis |
0.235 |
0.187 |
0.288 |
|
238 |
Cellulitis |
0.273 |
0.222 |
0.329 |
|
239 |
Abscess, impetigo, and other bacterial skin diseases |
0.267 |
0.215 |
0.324 |
|
240 |
Scabies |
0.194 |
0.150 |
0.245 |
|
241 |
Fungal skin diseases |
0.260 |
0.210 |
0.316 |
|
242 |
Viral skin diseases |
0.166 |
0.126 |
0.212 |
|
243 |
Acne vulgaris |
0.049 |
0.029 |
0.078 |
|
244 |
Alopecia areata |
0.154 |
0.114 |
0.200 |
|
245 |
Pruritus |
0.100 |
0.069 |
0.140 |
|
246 |
Urticaria |
0.106 |
0.074 |
0.147 |
|
247 |
Decubitus ulcer |
0.479 |
0.421 |
0.536 |
|
248 |
Glaucoma |
0.449 |
0.388 |
0.510 |
|
249 |
Cataracts |
0.324 |
0.267 |
0.383 |
|
250 |
Macular degeneration |
0.457 |
0.396 |
0.518 |
|
251 |
Refraction and accommodation disorders |
0.206 |
0.162 |
0.257 |
|
252 |
Dental caries |
0.065 |
0.042 |
0.097 |
|
253 |
Periodontal disease |
0.206 |
0.161 |
0.257 |
|
254 |
Edentulism |
0.471 |
0.410 |
0.531 |
|
255 |
Pedestrian injury by road vehicle |
0.470 |
0.410 |
0.530 |
|
256 |
Road injury (pedal cycle vehicle) |
0.315 |
0.262 |
0.371 |
|
257 |
Road injury (motorized vehicle with two wheels) |
0.495 |
0.435 |
0.555 |
|
258 |
Road injury (motorized vehicle with three or more wheels) |
0.597 |
0.538 |
0.653 |
|
259 |
Falls |
0.165 |
0.126 |
0.212 |
|
260 |
Drowning |
0.514 |
0.454 |
0.573 |
|
261 |
Fire, heat and hot substances |
0.362 |
0.304 |
0.423 |
|
262 |
Poisonings |
0.475 |
0.415 |
0.536 |
|
263 |
Mechanical forces (firearm) |
0.547 |
0.485 |
0.608 |
|
264 |
Adverse effects of medical treatment |
0.362 |
0.306 |
0.420 |
|
265 |
Animal contact (venomous) |
0.363 |
0.304 |
0.424 |
|
266 |
Animal contact (non-venomous) |
0.132 |
0.095 |
0.176 |
|
267 |
Self-harm |
0.516 |
0.455 |
0.577 |
|
268 |
Assault by firearm |
0.488 |
0.429 |
0.548 |
|
269 |
Assault by sharp object |
0.260 |
0.212 |
0.312 |
|
270 |
Exposure to forces of nature |
0.235 |
0.188 |
0.287 |
|
271 |
Collective violence and legal intervention |
0.432 |
0.373 |
0.492 |
|
272 |
Allergic rhinitis |
0.087 |
0.059 |
0.123 |
|
273 |
Atopic dermatitis |
0.231 |
0.182 |
0.285 |
|
274 |
Metabolic syndrome |
0.304 |
0.250 |
0.361 |
|
275 |
Allergic rhinitis and atopic dermatitis |
0.166 |
0.124 |
0.215 |
|
276 |
Diabetes mellitus and osteoarthritis |
0.495 |
0.436 |
0.553 |
|
277 |
Allergic rhinitis and asthma |
0.187 |
0.145 |
0.236 |
|
278 |
Allergic rhinitis and osteoarthritis |
0.192 |
0.147 |
0.244 |
|
279 |
Allergic rhinitis and major depressive disorder |
0.394 |
0.336 |
0.453 |
|
280 |
Major depressive disorder and osteoarthritis |
0.478 |
0.418 |
0.539 |
|
281 |
Diabetes mellitus and ischemic stroke |
0.629 |
0.570 |
0.685 |
|
282 |
Diabetes mellitus and tuberculosis |
0.478 |
0.418 |
0.539 |
|
283 |
Diabetes mellitus, osteoarthritis, and major depressive disorder |
0.543 |
0.484 |
0.601 |
|
284 |
Diabetes mellitus, osteoarthritis, and ischemic stroke |
0.667 |
0.611 |
0.719 |
|
285 |
Allergic rhinitis, asthma, and atopic dermatitis |
0.172 |
0.131 |
0.219 |
|
286 |
Diabetes, osteoarthritis, and tuberculosis |
0.574 |
0.514 |
0.632 |
|
287 |
Diabetes mellitus, osteoarthritis, rheumatoid arthritis |
0.494 |
0.431 |
0.556 |
|
288 |
Full heath |
0.000 |
0.000 |
0.000 |
|
289 |
Being dead |
1.000 |
1.000 |
1.000 |







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download