INTRODUCTION
Temporary anchorage devices (TADs) have been used in clinical practice for anchorage and tooth movement, including intrusion and extrusion, distalization and mesialization, correction of the tooth axis and occlusal cant,
en-masse retraction procedures,
12 and to apply orthopedic force.
3 They can be placed at several sites during a single appointment without the need for a complicated surgical procedure.
4 However, TADs are also associated with various complications including vessel and sinus injury, TAD fracture during removal, TAD failure during insertion,
56 and TAD movement during orthodontic loading.
7 One possible reason for these complications has been suggested to be inadequate inter-radicular space between the root and TAD. The preferred and most secure site for TAD application was suggested to be the inter-radicular bone between the roots of adjacent teeth. However, this area was also associated with a risk of root damage.
8910 In addition to incorrect placement, TADs may also accidentally contact the root during the application of orthodontic force.
It was reported that root contact with TADs resulted in root resorption but that root repair occurred after contact was discontinued; damage was restricted to the cementum or dentin with no pulpal perforation.
2 Studies evaluating the healing period after root damage caused by TADs have reported conflicting results. For example, Kadioglu et al.
8 reported that complete healing occurred in 8 weeks, whereas Ahmed et al.
10 suggested that more than 12 weeks were required for complete healing in their clinical studies of patients. There is a lack of knowledge about the management of complications caused by TADs.
2
Micro-computed tomography (CT) is a fast, high-resolution method with a low error rate that enables advanced visual and three-dimensional (3D) evaluations.
1112 Previously, it was used to monitor and measure resorption craters on the root surfaces of extracted teeth after orthodontic tooth movement.
13 Previous studies examined the accuracy of 3D evaluations of root resorption craters versus two-dimensional histological and radiographic evaluations.
1415 To the best of our knowledge, there has been no 3D imaging study on the effect of the removal order of TADs or on the force used for root repair 12 weeks after accidental root-TAD contact. Thus, the aim of the current study was to evaluate force loading on root damage after root-TAD contact and on the root repair process over time (at 4, 8, and 12 weeks) after root-TAD contact. An additional aim was to add to the knowledge base on the management of this complication. We hypothesized that orthodontic force would cause more damage to the root surface than a TAD and that healing after damage would be incomplete at 12 weeks.
MATERIALS AND METHODS
This study adopted an experimental clinical design previously described in the literature.
8 Forty-two volunteers (24 female subjects and 18 male subjects aged between 13 and 18 years; mean, 15.15 ± 1.55 years) who required bilateral upper first premolar extractions who presented for orthodontic treatment between May 2014 and December 2015 in the Department of Orthodontics, Faculty of Dentistry, Inonu University were included. The current study was approved by the clinical research ethics committee of Inonu University (#2014-22). Written and detailed informed consent was obtained from the parents or guardians of all participants.
The exclusion criteria for all participants were a history of orthodontic treatment, poor oral hygiene with gingivitis detected by a periodontal clinical examination, metal allergies, non-cooperation, craniofacial or dentoalveolar anomalies, incomplete tooth apexification confirmed by radiographs, and close proximity between roots and impacted canines.
16
Study groups and design
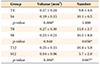
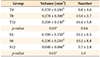
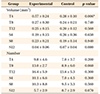
The randomization was performed at baseline for patient selection. All right sides were selected as the positive control group and all left sides were selected as the experimental group. Participants were divided into the TAD group (Group T: only TAD removal, n = 21) and the spring group (Group S: only spring removal, n = 21) according to the type of the removed appliances. For both groups' first premolars, cantilever springs were placed, and TADs were then immediately inserted between the first and second premolars. A split-mouth design was used in both groups as follows. In each volunteer, the left premolars were extracted 4, 8, or 12 weeks after TAD-root contact (Group T and Group S). The right premolars were extracted immediately after TAD-root contact and used as positive controls (Groups T-C and S-C) (
Figure 1). Resorption crater volumes and numbers of craters were determined by micro-CT.
Clinical procedure
Molar bands (Seamless Bands; 3M Unitek, Monrovia, CA, USA) were cemented to the upper first molars with glass ionomer cement (Ketac; 3M ESPE, Seefeld, Germany) and 0.022-inch self-ligating brackets (Empower; American Orthodontics, Sheboygan, WI, USA) were then applied to both upper first premolars (Transbond XT; 3M Unitek). Titanium molybdenum alloy cantilever springs (BT3, 14 × 0.017 × 0.025 inch; G&H, Franklin, IN, USA) were applied with a 150-g force (
Figure 2) and TADs (Aarhus screw; Medicon, Tuttlingen, Germany) with a 1.5-mm diameter and 8-mm length were placed between the first and second premolars. Resin-modified glass ionomer cement (Multi-Cure Glass Ionomer Orthodontic Band Cement; 3M Unitek) was placed on the surface of the mandibular first molars to avoid occlusal interference (
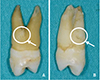
Figure 3). The positions of the TADs were confirmed on periapical radiographs (
Figure 4A and 4B). The force was applied until TAD-root contact was obtained, which occurred after 4 weeks in all participants.
In all individuals in Groups T-C and S-C, the right premolars were extracted immediately after TAD-root contact was confirmed by periapical radiographs. Following TAD-root contact, the left premolars were extracted 4, 8, or 12 weeks after TAD removal (Group T) or spring removal (Group S).
The same surgeon performed all extractions under local anesthesia. During the extraction process, care was taken when using extraction forceps to avoid damage to the surfaces of the roots. After the extractions, blood and tissue residues on the teeth were removed by pressureless washing with an isotonic solution without damaging the root surface. For each tooth, root resorption was observed by visual inspection with the aid of a magnifying glass (
Figure 5). The extracted teeth were then transferred to sterile tubes. Finally, the teeth were transferred to the laboratory for radiographic analysis.
Radiographic analysis
The numbers and volumes of resorption craters were detected using a micro-CT system (SkyScan 1172; Bruker, Kontich, Belgium). In total, 1,300 to 1,350 sections were obtained with a rotation interval of 0.40° and thickness of about 9.0 µm while rotating the device 360° to scan the teeth. The area of evaluation was limited to the cervicoapical direction of cross-section slides (CTAn 1.15.4.0, SkyScan; Kontich). The total root surface was divided into three parts: cervical, middle, and apical. Each part was further divided into four sub-regions: mesiobuccal, distobuccal, mesiolingual, and distolingual (
Figure 6). The resorption area in all three planes was separated from other tissues by using the same program (CTAn 1.15.4.0, SkyScan). In the second step, a binary view page was used to perform thresholding in order to determine the resorption craters. A custom processing page was utilized and the same task list was used as the standard to calculate the volumes and numbers of resorption craters in each sample. Finally, the volumes and numbers of craters in the roots were calculated.
Statistical analysis
To determine the sample size for each group, a power analysis was carried out based on an alpha significance level of 0.05 and beta value of 0.1 to achieve 90% power to detect an average difference of 0.5 mm
3 (± 0.20 mm
3) in resorption craters on root surfaces from the different groups (version 3.0.10, G*Power; Franz Faul Universidad, Kiel, Germany).
17 The power analysis showed that seven patients were required in each group. Thus, to achieve 90% power (significance levels: alpha = 0.05, beta = 0.1), the patients in Group T and Group S were randomly divided into three subgroups according to the observation period (4, 8, or 12 weeks) with seven patients in each group.
Descriptive statistical data (the mean and standard deviation) are presented. Non-parametric statistical tests were conducted to determine the volumes and numbers of resorption craters. The Kruskal-Wallis test, a one-way analysis of variance, and the Mann-Whitney U test with the Bonferroni correction were performed for statistical assessments. The data were analyzed using SPSS software ver. 22.0 (IBM Corp., Armonk, NY, USA).
DISCUSSION
Root damage caused by TADs is a common complication seen in clinical practice.
2 There is limited knowledge on the management of this complication, including the repair process of the root surface and the timing of force loading. Thus, the current study investigated the repair process for root damage caused by TADs using micro-CT. The results revealed that a 12-week period may not be adequate for root healing. The results also suggested that when TADs cause root damage, clinicians should remove the loading immediately and should not perform reloading for longer than 12 weeks.
Several studies
8910 have evaluated changes to the root surface after TAD-root contact. Kadioglu et al.
8 examined root damage in 10 patients over an 8-week period histologically and reported that collagen fibrils completely covered the damaged surface during the entire period. In the current study, which adopted a similar group design to that used by Kadioglu et al.,
8 an 8-week period was not adequate for the root repair process, as evaluated by micro-CT. Instead, longer than 12 weeks was required for the repair process. The discordance between the study findings may be attributed to the methodologies used, as a histological analysis is superior to micro-CT in terms of the detection of repaired cementum.
17 Kadioglu et al.
8 also evaluated the removal order of the spring or TAD but they did not report a comparison of the removal order. In addition, in the same study, they did not conduct a statistical analysis of the impact of the removal order of springs or TAD on the healing period. In the current study, immediately after TAD-root contact, the first step was removal of the spring, followed by no reloading for longer than 12 weeks. In this study, crater volumes and numbers significantly decreased after removing the spring and leaving the TAD in contact with the root
in situ (Group S) compared with removal of the TAD with continuous force (Group T) for 12 weeks. Both groups showed a tendency toward decreased crater volumes after 12 weeks but with no difference in crater numbers. Thus, complete root healing did not appear to have occurred by 12 weeks, as shown by micro-CT.
Ahmed et al.
10 examined cementum repair after TAD-root contact in human upper first premolars and reported that 70% of teeth showed ≥ 90% healing at 12 weeks, with most healing completed by 8 weeks. They concluded that longer than 12 weeks was required for complete healing. However, they did not examine the effects of force loading and did not leave the TAD
in situ after TAD-root contact. In the current study, similar to the findings of Ahmed et al.,
10 a 12-week period was not sufficient for healing. In addition, leaving the TAD in contact with the root affected the repair process less adversely compared with removal of the TAD with continuous force. TAD-root contact may not be detected immediately in a clinical setting. The results of the present study suggest that it is better to remove the spring at the time of the detection of TAD-root contact rather than to remove the TAD and that longer than a 12-week period should elapse before the application of a reloading force.
Maino et al.
9 evaluated the effects of a root notch caused by drills or TAD contact in two male patients and reported that the root notch partially healed with the formation of cellular cementum almost 8 weeks after root drilling. After the root notch occurred and the root was in contact with a TAD for 1 week, followed by a delay of 4 weeks, the defect was only partially healed. They concluded that a force of 200
g from an open-coil spring may disturb root healing following root damage. Similar to their results, in the current study, only partial healing of root damage related to TADs was observed after 4 weeks, and healing was reduced compared to that at 8 and 12 weeks. Total healing was not observed until 12 weeks. Furthermore, in the current study, a loading force of 150
g from cantilever springs prolonged the healing period.
Kim and Kim
18 examined root damage caused by TAD-root contact in four mini-pigs for up to 16 weeks and evaluated the impact of leaving the TAD in contact with the teeth
in situ on the healing of damaged roots. They concluded that when TAD-root contact occurs, the TAD should be removed immediately. They also reported that when the TAD was left in contact with the root
in situ , no definitive cementum repair was observed for up to 16 weeks. In the current study, in the group in which the TAD was left
in situ without force (Group S), crater volumes were decreased at 12 weeks compared to those at 4 weeks, whereas crater numbers remained similar at all observation time points. The decrease in crater volume was attributed to spring removal, which may cause relapse and thus the TAD-root contact may be not be tight. In the study by Kim and Kim,
18 the authors removed the TAD after TAD-root contact and evaluated root healing over a 16-week period without force loading. They observed partial healing after 4 weeks and increased healing over time, with complete healing observed by 8 to 16 weeks. In the current study, crater volumes in the group that underwent TAD removal with continuous force (Group T) decreased over time, but crater numbers were similar in Group T at all observation time points. The differences in crater volumes were attributed to continued force loading from springs in the TAD removal group (Group T) possibly decreasing healing. Kim and Kim
18 also reported that root damage caused by TADs was irreversible when the TADs penetrated the pulp. In the current study, no pulpal damage was detected. The effects of TAD removal on healing were not compared with the findings of Kim and Kim
18 because of the difference in study designs.
Hembree et al.
19 evaluated the healing process following root damage caused by TAD-root contact over both short (6 weeks) and long (12 weeks) periods in seven beagle dogs. They reported that damage caused by leaving the TAD
in situ and in contact with the roots was the same at 6 and 12 weeks compared to that at baseline, contrary to expectations. They also reported that leaving a TAD in contact with the root may not stimulate root resorption without continuous force. Similar to their findings, we found significantly lower crater volumes and numbers at 12 weeks in Group S compared with those in Group T. Thus, force loading from springs appeared to cause more resorption and less healing than leaving a TAD in contact with the root
in situ without force for 12 weeks.
Similar to Hembree et al.,
19 Renjen et al.
20 evaluated the effect of TAD-root contact on the root surface in three beagle dogs for 12 weeks and concluded that TAD penetration of the root surface did not influence cementum repair or healing. In the current study, similar to the findings of Renjen et al.,
20 leaving the TADs
in situ appeared to have less of an effect on healing than a continuous force.
The minimum distance between the root and TAD was suggested to be 1.5 mm.
21 In addition, root resorption was reported when the mini-implant was closer than 0.6 mm to the root.
22 In the current study, to prevent the possible stimulation of root absorption by TADs, the TADs were placed using a minimally invasive technique and a low torque between the middle of the roots; initial cone-beam computed tomography (CBCT) was not acquired and this was accepted as a limitation. Although we did not measure the distance between the root and TAD at baseline using CBCT, no invasion of the periodontal ligament of the roots occurred, as confirmed by radiographs and a visual inspection.
Previous research reported that root resorption due to iatrogenic trauma may differ from root resorption due to orthodontically induced inflammation.
18 Therefore, the response to healing may vary.
18 In the present study, the experimental model aimed to mimic accidental contact between a TAD and roots during anchorage. Thus, the current results may apply only to orthodontically induced inflammatory root resorption with damage caused by TADs. Further studies on trauma-related root injury and inflammatory root resorption caused by TAD insertion or drilling may be needed.
Clinically, during conventional orthodontic treatment, resorption and healing can occur between appointments.
23 A continuous orthodontic force initiates the resorption process.
24 However, when this force is discontinued or falls below a certain level, the resorption lacuna begins to repair.
24 In cases where root resorption is detected during orthodontic treatment, it is recommended that the application of active force be stopped. In some cases, iatrogenic injuries induced by TADs may contribute to root resorption.
25 As shown in the present experimental model, accidental contact between the root and TAD, even when it is inserted in an ideal position, may cause root resorption. Thus, when TAD-root contact occurs, clinicians should not continue force loading on the damaged root. They should allow time for the healing process, which may require longer than 12 weeks.
Some previous studies
1726 used passive retention wires. According to Xu et al.,
27 the most serious relapse in tooth movement occurred immediately after removal of the wires, and then the tooth returned completely to its original position. In the current study, a passive wire was not applied after the spring was removed to keep the teeth in position. This was a limitation of the present study. As subsequent relapses may have increased resorption, the use of a passive wire in future studies may prevent tooth movement during retention or recovery.
According to the results of the current study, a 12-week period may not be adequate for total healing of damaged roots, and further studies with longer healing periods would be beneficial to provide more knowledge about the healing process. However, conducting studies of longer durations would likely prove difficult, as they would extend patients' treatment periods, and the patients would obtain no additional benefit from the treatment other than contributing to science.









 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download