INTRODUCTION
Cervical cancer occurs in approximately 528,000 people worldwide per year, and about 266,000 people per year die due to cervical cancer [
1]. The age-standardized incidence rate of cervical cancer in Korea has been decreasing, from 18.1 per 100,000 people in 1999 to 11.1 per 100,000 in 2013 [
234]. However, cervical cancer involves long-term carcinogenesis, unlike other cancers [
5]. Cervical cancer develops from a progression of epithelial cellular changes by multistages of oncogenic human papillomavirus (HPV) infection, persistent HPV infection, cervical intraepithelial neoplasia (CIN), and carcinoma in situ (CIS), which is a premalignant lesion of cervical cancer [
6]. Therefore, the fact that the incidence of new cases of cervical cancer is decreasing does not necessarily mean that the risk of cancer will be lower in the future.
While the age of first sexual intercourse is decreasing and the proportion of female smoker is rising, over 50% of women in Korea fail to get routine papanicolaou (Pap) smears [
7]. Although one might expect that the recent development of the HPV vaccine and the National Immunization Program (NIP) in Korea could prevent nearly 100% of HPV-related diseases, the NIP is not particularly addressing this issue as of now, besides its National Cancer Prevention, which offers Pap smear examinations to women ≥20 years of age.
Because of Korea's tight health care budget, the amount of investment in treating cervical cancer (for which an effective preventive measure is available) is an important issue. In order to ensure maximum effectiveness of any investment, it is necessary to assess the efficacy of the preventive measures by confirming not only the incidence of cervical cancer, but also the variation in the incidence of potentially pre-cancerous cervical lesions. However, so far, there is a lack of reliable data on CIN incidence in a unit ≥100,000 people, except data based on the results of Pap smears conducted in a small-scale cohort in Korea [
8].
Unlike other countries, the entire Korean population subscribes to one health insurance plan: the National Health Insurance Plan [
9]. Thus, by analyzing specific claim codes and procedure codes of the National Health Insurance Service, it is possible to estimate various factors of the causes of cervical cancer in Korean women.
According to many studies conducted in America [
1011], the medical cost per age and per disease was calculated for women with CIN or cervical cancer lesion. Similarly, we seek to collect and use such data in order to establish a prevention strategy.
The purpose of this study was to estimate the incidence rate and medical costs of pre-cancerous lesions around the cervix and cervical cancer based on age in the past 5 years (2010–2014) in Korean women in order to establish appropriate treatment protocols.
MATERIALS AND METHODS
1. Study population
We reviewed the data recorded by the national health claims database of the Health Insurance Review and Assessment (HIRA) service (2010–2014). The Institutional Review Board (IRB) of Uijeongbu St. Mary's Hospital approved the study protocol (#UC16EISI0020), and the study was conducted in accordance with the tenets of the Declaration of Helsinki.
All citizens of Korea are expected to register for Korean National Health Insurance, which covers about 98% of the Korean population [
12]. While the inpatients insured by the Korean National Health Insurance pay about 20% of their total medical expenses, the outpatients have paid about 50% recently. What is more, the patients with severe diseases such as cervical cancer (C53) or CIS of uterine cancer (D06) pay only 5% of their medical costs. Claims are accompanied by data regarding the diagnosis, procedure, prescription record, demographic information, and direct medical cost. Medical expenses not covered by the Korean National Health Insurance Plan are covered by the Medical Assistance Program or the Medical Care for Patriots and Veterans Affairs Plan. The claims from these other 2 plans are also recorded in the HIRA database. Therefore, the HIRA database is very extensive, including information on the entire Korean population, personal information on all patients, and medical records related to all medical claims made in Korea [
13].
A resident registration number is assigned to all Korean citizen at birth. This number is unique to each citizen and widely utilized by the government, including HIRA, for easy identification of citizens. HIRA database can therefore be used to obtain accurate health care records and demographic characteristics for CIN patients with no duplicates of this personal data. The HIRA database manages claims using the Korean Classification of Disease (6th edition), which is a modified version of the International Classification of Diseases, 10th edition (ICD-10), adapted for the Korean health care system. The compulsory healthcare system in Korea covers all CIN-related healthcare costs.
Herein, because all treatments for CIN and cervical cancer are either completed within a year or last longer than a year, and there is no data on those who were uninsured for less than a year, we counted the number of patients who did not claim any reimbursement in the previous year and filed one or more reimbursement claims in a year according to the relevant standardized disease codes, C53 (cervical cancer), D06 (CIN/CIS), N72 (cervicitis), N86 (cervical erosion), and N87 (CIN 1/2), as the number of women with pre-cancerous lesions or cervical cancer. In that way, we determined the yearly incidence rate from 2010–2014 and recorded the frequency of visits and the amount of reimbursement claims in each of those years.
Since codes C53 and D06 indicate that patients are severely ill, it is nearly impossible for them to file duplicate or false claims; C53 represents cervical cancer and D06 represents CIS. However, N72, N86, and N87 do not necessarily reflect CIN 1/2. Nevertheless, if a CIN is suspected, the necessary fee-for-service codes (such as those for punch biopsy and loop electrosurgical excision procedure [LEEP] conization), will be applied in addition to these procedure codes. The International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) vol. 3 codes include the following: colposcopy (70.21), chemical cauterization or vagina or uterine cauterization (68.29), cauterization of vagina (70.33), cervical histopathologic examination (67.12), conization of cervix (67.32), and conization of cervix (loop electrosurgical excision, 67.32). Any person who filed a reimbursement claim with any of those codes at least once was assigned an incidence of CIN 1/2.
The index date was recorded as the incident time, and the patient was considered an incidence in that year. The population at risk was extrapolated from the entire population of Korea, based on the resident registration available from the Korean Statistical Information Service [
9]. The population at risk consisted of Korean women over 20 years old, who were included by the Korean Statistical Information Service's resident registration, but not necessarily the beneficiaries of national health insurance. The number of Korean women over 20 years old were as estimated to be 20,280,871 in 2010, 20,556,348 in 2011, 20,855,339 in 2012, 21,160,289 in 2013, and 21,476,390 in 2014.
2. Statistical analysis
The person-time incidence rates for 2010–2014 were calculated as the number of people in whom CIN and cervical cancer developed, divided by the total person-time at risk during the study period. Therefore, in this analysis, person-years were counted after the incident time. The annual CIN incidence rates were calculated as persons in whom CIN developed, divided by the total population, based on the resident registration each year. Age-specific CIN and cervical cancer incidence rates were estimated. A 95% confidence interval (CI) for the incidence rate was estimated based on the poisson distribution. The χ2 analysis was used to compare the observed incidence rates between women over 30 years of age and younger women. The association between incidence of CIN and cervical cancer, and age groups was analyzed by logistic regression analysis as well as multiple regression analysis. A weighted generalized linear model was used in order to calculate the number of visits to health care institutions and the medical fee reimbursement claim per capita and per visit each year. We used SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA) for all analyses. The p-values <0.05 were considered to be significant.
RESULTS
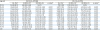
From 2010 through 2014, CIN 1/2 developed in 437,298 people, and CIN 3 in 50,270 people (
Table 1). There were differences regarding people's age in the incidence rate of both CIN 1/2 and CIN 3 (p<0.001, respectively). There were also differences in the incidence rate ratio of both CIN 1/2 and CIN 3 regarding to people's age (p<0.001, respectively). The incidence rates of CIN 1/2 in 2010, 2011, 2012, 2013, and 2014 were 317.9, 324.4, 317.7, 373.3, and 425.4 per 100,000 people, respectively, which illustrate an increasing trend (p for trend: <0.001,
Fig. 1). The incidence rates of CIN 3 measured in the same years were 40.5, 41.4, 38.9, 39.4, and 39.8 per 100,000 people, respectively, which illustrate a decreasing trend (p for trend: 0.007). The incidence rates of cervical cancer measured in the same years were 30.3, 29.7, 29.8, 30.2, and 28.4 per 100,000 people, respectively, which illustrate a decreasing trend (p for trend: 0.002).
Table 1
Actual numbers and incidence rates of CIN in Korean population from 2010 to 2014
|
Age (yr) |
CIN 1/2 (n=437,298) |
CIN 3 (n=50,270) |
|
No. (%)*
|
IR (95% CI)†
|
IRR (95% CI) |
p-value‡
|
No. (%)*
|
IR (95% CI)†
|
IRR (95% CI) |
p-value‡
|
|
20–24 |
35,488 (8.11) |
460 (455–465) |
1 (ref.) |
|
752 (1.50) |
9.74 (9.06–10.5) |
1 (ref.) |
|
|
25–29 |
61,583 (14.1) |
741 (735–747) |
1.61 (1.50–1.63) |
<0.001 |
3,977 (7.91) |
47.8 (46.4–49.3) |
4.91 (4.54–5.31) |
<0.001 |
|
30–34 |
71,648 (16.4) |
736 (731–742) |
1.60 (1.58–1.62) |
<0.001 |
7,967 (15.8) |
81.9 (80.1–83.7) |
8.41 (7.80–9.06) |
<0.001 |
|
35–39 |
64,335 (14.7) |
634 (629–638) |
1.38 (1.36–1.40) |
<0.001 |
7,669 (15.3) |
75.5 (73.9–77.2) |
7.75 (7.19–8.36) |
<0.001 |
|
40–44 |
66,603 (15.2) |
601 (596–606) |
1.31 (1.29–1.32) |
<0.001 |
8,674 (17.3) |
78.3 (76.6–79.9) |
8.03 (7.46–8.65) |
<0.001 |
|
45–49 |
55,296 (12.6) |
532 (528–537) |
1.16 (1.14–1.17) |
<0.001 |
6,874 (13.7) |
66.2 (64.6–67.8) |
6.79 (6.30–7.32) |
<0.001 |
|
50–54 |
38,955 (8.91) |
374 (370–377) |
0.81 (0.80–0.82) |
<0.001 |
5,218 (10.4) |
50.0 (48.7–51.4) |
5.14 (4.76–5.54) |
<0.001 |
|
55–59 |
20,025 (4.58) |
246 (243–250) |
0.54 (0.53–0.55) |
<0.001 |
3,211 (6.39) |
39.5 (38.2–40.9) |
4.05 (3.75–4.39) |
<0.001 |
|
60–64 |
10,680 (2.44) |
178 (175–182) |
0.39 (0.38–0.40) |
<0.001 |
2,240 (4.46) |
37.4 (35.9–39.0) |
3.84 (3.53–4.16) |
<0.001 |
|
65–69 |
6,405 (1.46) |
126 (123–129) |
0.27 (0.27–0.28) |
<0.001 |
1,644 (3.27) |
32.3 (30.7–33.8) |
3.31 (3.04–3.61) |
<0.001 |
|
70–74 |
3,969 (0.91) |
84 (81.4–86.6) |
0.18 (0.18–0.19) |
<0.001 |
1,209 (2.41) |
25.6 (24.2–27.1) |
2.63 (2.40–2.88) |
<0.001 |
|
75–79 |
1,667 (0.38) |
47.2 (45.0–50.0) |
0.10 (0.10–0.11) |
<0.001 |
601 (1.20) |
17.0 (15.7–18.4) |
1.75 (1.57–1.95) |
<0.001 |
|
≥80 |
644 (0.15) |
17.4 (16.1–18.7) |
0.04 (0.04–0.04) |
<0.001 |
234 (0.47) |
6.31 (5.54–7.15) |
0.65 (0.56–0.75) |
<0.001 |

 | Fig. 1
Incidence rate trend of CIN 1/2, CIN 3, and cervical cancer in Korea from 2010 through 2014.
CIN, cervical intraepithelial neoplasia.

|
As for the distribution by age, the peak age range was 25–29 years old for CIN 1/2, 30–34 years old for CIN 3, and 70–74 years old for cervical cancer (
Fig. 2). In addition, the incidence distribution was different for all grades in the 30s based on the above results (
Fig. 2, p for trend: <0.001). The incidence of CIN 1/2 showed an increasing trend in people of all ages (p for trend: <0.001,
Fig. 3A), while incidence of CIN3 showed an increasing trend amongst those 30–39 and ≥80 years old, but a decreasing trend in 40–44 and 50–54 years old (p for trend: <0.001,
Fig. 3B). The incidence of cervical cancer showed a decreasing trend in most age ranges, but an increasing trend amongst those 35–39 years old (p for trend: <0.001,
Fig. 3C).
 | Fig. 2
Comparison of the average annual incidence rate by grade according to age in Korea from 2010 through 2014.
CIN, cervical intraepithelial neoplasia.

|
 | Fig. 3
Incidence rate of CIN or cervical cancer according to the age in Korea from 2010 through 2014.
(A) Incidence rate of CIN 1/2. (B) Incidence rate of CIN 3. (C) Incidence rate of cervical cancer.
CIN, cervical intraepithelial neoplasia.

|
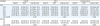
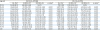
The number of visits per person, which was confirmed using the claims data of the HIRA service, reveals an increasing trend in all grades (CIN 1/2, CIN 3, and cervical cancer) from 2010–2014 (
Table 2). The medical costs per person decreased over time for CIN 1/2 (p for trend: 0.01,
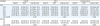
Table 3). In addition, for those over thirty years of age, the health care cost associated with all 3 grades increased (p for trend: <0.001, 0.001, and 0.032 for CIN 1/2, CIN 3, and cervical cancer, respectively,
Table 3). Furthermore, when comparing the age-specific costs in CIN, particularly for age <30 and ≥30, the mean cost per visit has increased significantly for age ≥30 (p for trend: <0.001 and 0.002 for CIN 1/2 and CIN 3, respectively,
Table 4).
Table 2
Health care resource utilization per episode of care for CIN 1/2, CIN 3, cervical cancer

|
Variables |
CIN 1/2 (n=442,658) |
CIN 3 (n=50,309) |
Cervical cancer (n=37,311) |
|
Patients*
|
Visit per person |
Patients*
|
Visit per person |
Patients*
|
Visit per person |
|
Year |
|
|
|
|
|
|
|
2010 |
79,172 (17.9) |
1.26 (1.24–1.28) |
10,081 (20.0) |
2.76 (2.69–2.83) |
7,550 (20.2) |
5.00 (4.79–5.20) |
|
2011 |
81,195 (18.3) |
1.26 (1.23–1.28) |
10,370 (20.6) |
2.98 (2.91–3.05) |
7,433 (19.9) |
6.21 (5.92–6.49) |
|
2012 |
79,939 (18.1) |
1.30 (1.27–1.33) |
9,798 (19.5) |
3.80 (3.66–3.93) |
7,485 (20.1) |
9.35 (9.00–9.69) |
|
2013 |
94,355 (21.3) |
1.34 (1.31–1.36) |
9,958 (19.8) |
3.79 (3.68–3.90) |
7,637 (20.5) |
9.11 (8.63–9.59) |
|
2014 |
107,997 (24.4) |
1.34 (1.32–1.37) |
10,102 (20.1) |
3.72 (3.63–3.80) |
7,206 (19.3) |
8.80 (8.30–9.29) |
|
p for trend†
|
|
<0.0001 |
|
<0.0001 |
|
<0.0001 |
|
Age (yr) |
|
|
|
|
|
|
|
<30 |
102,431 (23.1) |
1.37 (1.36–1.39) |
4,768 (9.48) |
3.61 (3.34–3.87) |
936 (2.51) |
6.45 (5.46–7.43) |
|
≥30 |
340,227 (76.9) |
1.28 (1.27–1.30) |
45,541 (90.5) |
3.38 (3.26–3.51) |
36,375 (97.5) |
7.72 (7.22–8.22) |
|
p for trend†
|
|
<0.001 |
|
0.254 |
|
0.383 |

Table 3
The medical costs per person related with CIN or cervical cancer in a Korean population

|
Variables |
CIN 1/2 |
CIN 3 |
Cervical cancer |
|
Patient*
|
Visit†
|
Cost per person |
Patient*
|
Visit†
|
Cost per person |
Patient*
|
Visit†
|
Cost per person |
|
Year |
|
|
|
|
|
|
|
|
|
|
2010 |
79,172 (17.9) |
99,706 (17.3) |
90.8‡ (84.3–97.3) |
10,081 (20.0) |
27,849 (16.3) |
459‡ (378–540) |
7,550 (20.2) |
37,731 (13.2) |
3,133‡ (2,988–3,278) |
|
2011 |
81,195 (18.3) |
102,055 (17.7) |
95.5‡ (88.3–103) |
10,370 (20.6) |
30,890 (18.0) |
484‡ (396–571) |
7,433 (19.9) |
46,128 (16.1) |
3,287‡ (3,108–3,467) |
|
2012 |
79,939 (18.1) |
104,117 (18.0) |
87.6‡ (81.7–93.5) |
9,798 (19.5) |
37,190 (21.7) |
461‡ (386–536) |
7,485 (20.1) |
69,964 (24.4) |
3,235‡ (3,107–3,362) |
|
2013 |
94,355 (21.3) |
126,054 (21.8) |
83.8‡ (78.9–88.7) |
9,958 (19.8) |
37,752 (22.0) |
474‡ (390–557) |
7,637 (20.5) |
69,586 (24.3) |
3,252‡ (3,075–3,429) |
|
2014 |
107,997 (24.4) |
145,024 (25.1) |
84.8‡ (80.2–89.4) |
10,102 (20.1) |
37,540 (21.9) |
466‡ (396–537) |
7,206 (19.3) |
63,385 (22.1) |
3,347‡ (3,191–3,503) |
|
p for trend§
|
|
|
0.01 |
|
|
0.998 |
|
|
0.162 |
|
Age (yr) |
|
|
|
|
|
|
|
|
|
|
<30 |
102,431 (23.1) |
140,735 (24.4) |
72.2‡ (69.3–75.0) |
4,768 (9.48) |
17,189 (10.0) |
298‡ (288–307) |
936 (2.51) |
6,033 (2.10) |
2,848‡ (2,412–3,284) |
|
≥30 |
340,227 (76.9) |
436,221 (75.6) |
93.2‡ (90.8–95.6) |
45,541 (90.5) |
154,032 (90.0) |
488‡ (449–526) |
36,375 (97.5) |
280,761 (97.9) |
3,268‡ (3,196–3,339) |
|
p for trend§
|
|
|
<0.001 |
|
|
<0.001 |
|
|
0.032 |
|
Total number |
442,658 |
576,956 |
|
50,309 |
171,221 |
|
37,311 |
286,794 |
|

Table 4
The medical costs per visit related with CIN or cervical cancer in a Korean population
|
Variables |
CIN 1/2 |
CIN 3 |
Cervical cancer |
|
Patient*
|
Visit†
|
Cost per visit |
Patient*
|
Visit†
|
Cost per visit |
Patient*
|
Visit†
|
Cost per visit |
|
Year |
|
|
|
|
|
|
|
|
|
|
2010 |
79,172 (17.9) |
99,706 (17.3) |
72.5‡ (66.2–78.8) |
10,081 (20.0) |
27,849 (16.3) |
168‡ (136–199) |
7,550 (20.2) |
37,731 (13.2) |
623‡ (609–637) |
|
2011 |
81,195 (18.3) |
102,055 (17.7) |
76.4‡ (69.4–83.4) |
10,370 (20.6) |
30,890 (18.0) |
164‡ (132–196) |
7,433 (19.9) |
46,128 (16.1) |
526‡ (511–540) |
|
2012 |
79,939 (18.1) |
104,117 (18.0) |
67.7‡ (61.8–73.4) |
9,798 (19.5) |
37,190 (21.7) |
123‡ (101–145) |
7,485 (20.1) |
69,964 (24.4) |
345‡ (333–357) |
|
2013 |
94,355 (21.3) |
126,054 (21.8) |
62.9‡ (58.3–67.6) |
9,958 (19.8) |
37,752 (22.0) |
126‡ (102–151) |
7,637 (20.5) |
69,586 (24.3) |
354‡ (346–361) |
|
2014 |
107,997 (24.4) |
145,024 (25.1) |
63.3‡ (59.0–67.8) |
10,102 (20.1) |
37,540 (21.9) |
126‡ (106–146) |
7,206 (19.3) |
63,385 (22.1) |
377‡ (367–387) |
|
p for trend§
|
|
|
<0.001 |
|
|
0.005 |
|
|
<0.001 |
|
Age (yr) |
|
|
|
|
|
|
|
|
|
|
<30 |
102,431 (23.1) |
140,735 (24.4) |
52.6‡ (50.3–54.9) |
4,768 (9.48) |
17,189 (10.0) |
81.9‡ (77.5–86.3) |
936 (2.51) |
6,033 (2.10) |
425‡ (365–484) |
|
≥30 |
340,227 (76.9) |
436,221 (75.6) |
72.9‡ (70.3–75.5) |
45,541 (90.5) |
154,032 (90.0) |
145‡ (132–159) |
36,375 (97.5) |
280,761 (97.9) |
420‡ (393–447) |
|
p for trend§
|
|
|
<0.001 |
|
|
0.002 |
|
|
0.987 |

DISCUSSION
There is not much published data on the overall incidence or costs yet. Therefore, this study sought to estimate the annual change of the incidence of CIN and its associated medical costs in Korean women by age in order to help establish an early preventive strategy based on the results. We collected data on annual incidence and medical costs of CIN and cervical cancer from 2010 until the end of 2014 from the HIRA database. Incidence rates of CIN 3 and cervical cancer are reducing over time, whereas CIN 1/2 is increasing significantly. The crude incidence of CIN 1/2 increased by approximately 30% in 2014 compared to 5 years ago and demonstrated an increasing trend in all age groups. The CIN 3 showed a significantly increasing trend in the age group of 30–39 years old, the cervical cancer was significantly reduced in all ages, except the 35–39 years old. When comparing the age-specific costs in CIN, the mean cost per visit has increase significantly for age ≥30
The HIRA database provides information on the various diseases endured by more than 10 million subscribers, among whom the majority are Korean women. Therefore, our study included a greater amount of data on the residents of Korea by region than did other studies.
In 2014, the incidence rates of CIN 1/2 and CIN 3 were 425.4 and 39.8 per 100,000 people, respectively. According to a study conducted in the United States (US), the incidence of CIN 1 is 120 per 100,000, and that of CIN 2/3 is 150 per 100,000 [
10]. Another US study found that the incidence of CIN 1 is 160 per 100,000 people, and that of CIN 2/3 is 120 per 100,000 [
11]. The overall incidence of CIN in the US was 270 per 100,000, which is less than that of Korea [
10]. According to the Health Plan study conducted from 1999 to 2004 in the US, the peak age group in which women develop both CIN 1 and CIN 2/3 is 21–30, with a decrease in incidence after the age of 30. This indicates that the peak age for CIN 3 is younger in the US than in Korea (30–34 years old).
When compared to the US study, the peak age of CIN 3 in our study is a little older, which may partly be due to the Pap smear rate given for cervical cancer screenings. According to the Korea National Health and Nutrition Examination Survey (2009–2012), only approximately 50% of all women received Pap smears; those under the age of 40 had a Pap smear rate lower than 29% [
7]. And the other reason is the difference in the age of first sexual intercourse. Because the age of first sexual intercourse was lower, there was an earlier peak age of CIN 3 in the US. Therefore, more aggressive and earlier Pap smear screening is needed in Korea.
The cost per visit in Korea is 30% less ($467) than the cost per visit in the US. In cases of CIN 1/2, the cost per visit is just $83, which is only 10% of the cost in the US. Expensive procedures for treating CIN 3, such as cold knife conization, large loop excision of the transformation zone (LLETZ), and occasionally hysterectomy, are more commonly used than CIN 1/2 [
11].
According to a CIN incidence study performed in Israel, Israel has a crude incidence rate of cervical cancer of 5 per 100,000 people, which is lower than that in Korea. The crude incidence rate for CIN 1/2 was 111 per 100,000 people, while that for CIN3 was 36 per 100,000. These values indicate that the incidence rate of CIN 1/2 is lower in Israel than in Korea, whereas the rate of CIN 3 is similar to that of Korea. The percentage of women receiving routine Pap smears in Israel was about 50%, which is similar to that of Korea, and the peak incidence ages of CIN were the late thirties, similar to those of Korea. However, unlike in Korea, the incidence of CIN 1 is decreasing in Israel, and the incidence rates of CIN 2/3 are increasing year by year [
14]. The Israel population is given Pap smears beginning at the age of 20, and the reason that the peak age is in the late 30s is most likely due to the ethnic differences and differences in vaccination uptake rates. Additional studies are required to clarify this issue.
Although the incidence of cervical cancer in Korea is significantly decreasing, it is still above the global average (14 per 100,000 people) [
2]. As previously mentioned, the findings that the incidence rates of CIN 3 and cervical cancer are increasing amongst women of childbearing age (30–40s) indicate that screenings (Pap smears) are not conducted properly for women in their 20s. In addition, the finding that CIN 1/2 is steadily increasing in all age groups (increased by 30% in 2014, as compared to 2010) reflects the increase of HPV-related diseases, which signals the necessity for appropriate and aggressive early prevention measures.
The reason for the increasing CIN 1/2 might be the increase of the disease itself because the risk of HPV infection could be increasing over time, or the increase in the chance to get screening test because of the promotion of vaccination since 2008. However, despite the increase in the incidence of CIN 1/2, the incidence of CIN 3 is decreasing, possibly pointing to active treatment on CIN 1/2 as the causes for this particular trend.
When comparing the age-specific costs in all groups of CIN and cervical cancer, particularly for age <30 and ≥30, it was confirmed that the mean cost per capita for the patient and the mean cost per visit have increased significantly for age >30. The pre-30 and post-30 cost differences seemed to be caused by the high disease incidence frequency and the severity of the disease for age >30. Considering the pathogenesis of cervical cancer, early detection of cervical cancer before women turn 30 years old can make cost reduction in the disease treatment possible.
First, this is due to the prevalence of HPV persistent infection in women over the age of 30 and the longevity of the follow-up period. Second, there is a big difference in how women 20–30 years and women above 30 years are affected. While there is a peak in HPV infection between women of 20–30 years, it gets treated relatively quickly. On the other hand, there are many cases among women over 30 years of age, in which, punch biopsy, a long post-observation period, and eventually LEEP conization are all implemented because of the persistent infection that follows CIN lesion.
According to a 2013 report by the Centers for Disease Control and Prevention, Korea has a completion rate of approximately 28.7% in the age range of 19–26 years, since the domestic marketing of the vaccine against cervical cancer was authorized in 2008 [
15]. The National Vaccination Project to prevent cervical cancer was launched nationwide in 2016. However, it takes 10 years to examine the effect of the cervical cancer vaccine [
16].
In our study, we found that the incidence rate and medical costs related to CIN differ by age. To effectively implement secondary prevention strategies against cervical cancer within a limited budget, age-specific strategies should be more closely studied in the future.
This study has a few limitations. First, because we carried out this research relying on somewhat unclear disease codes and the number of claims provided by the HIRA service, it is highly likely that there are duplicated or false claims, and that the actual residence address may be different from the registered address. For example, since the incidence rate was calculated by excluding the previous year's claimants only, patients with cervical cancer who were assigned accurate disease codes may have been included twice in our data if they were diagnosed 2 years previously and, in addition, obtained healthcare for their condition within those 2 years. There is also a high potential that cervical cancer will recur, but this would not have a large influence on the comparison of incidence rates over the course of 5 years. Secondly, since CIN 1/2 was identified with a combination of a disease code and fee code, it is likely that we included cases of other conditions, such as chronic cervicitis or genital warts. Indeed, treatment for CIN was not followed up at an interval of ≥1 year; therefore, within these conditions, it is challenging to distinguish between CIN 1/2 and chronic cervicitis or genital warts. Lastly, although the classification of CIN 1 and CIN 2 is important for the difference in management of surgical treatment versus observation, it is difficult to classify it accurately as a realistic constraint (coding inaccuracy).
This study is significant as it is the first study on the incidence of CIN and cervical cancer in Korea conducted in the largest possible population. This study was conducted in a single community consisting of the largest population over the course of 5 years. It will be the basis for confirming the predicted size of the pre-cancerous lesion of cervix and the effect of vaccination in the future. Our results illustrated that the crude incidence rate of cervical cancer is currently decreasing among Korean women, but the incidence rates and medical costs of CIN and cervical cancer are increasing in women in their 30s in Korea. This study shows that cervical cancer preventive strategies are not effectively implemented in Korea. We have focused on increasing cervical cancer vaccine coverage and improving Pap smear screening rate for women in their 20s.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download