1. Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global cancer in women: burden and trends. Cancer Epidemiol Biomarkers Prev. 2017; 26:444–457.


2. International Agency for Research on Cancer. Cancer today [Internet]. Lyon: International Agency for Research on Cancer;cited 2018 Aug 2. Available from:
http://gco.iarc.fr/today.
3. Syauqy A, Hsu CY, Rau HH, Chao JC. Association of dietary patterns with components of metabolic syndrome and inflammation among middle-aged and older adults with metabolic syndrome in Taiwan. Nutrients. 2018; 10:143.


4. Ahluwalia N, Andreeva VA, Kesse-Guyot E, Hercberg S. Dietary patterns, inflammation and the metabolic syndrome. Diabetes Metab. 2013; 39:99–110.


6. Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. 2014; 2014:149185.

7. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014; 17:1689–1696.


9. Vahid F, Shivappa N, Hekmatdoost A, Hebert JR, Davoodi SH, Sadeghi M. Association between maternal dietary inflammatory Index (DII) and abortion in Iranian women and validation of DII with serum concentration of inflammatory factors: case-control study. Appl Physiol Nutr Metab. 2017; 42:511–516.


10. Shivappa N, Schneider A, Hébert JR, Koenig W, Peters A, Thorand B. Association between dietary inflammatory index, and cause-specific mortality in the MONICA/KORA Augsburg Cohort Study. Eur J Public Health. 2018; 28:167–172.


12. Ren Z, Zhao A, Wang Y, Meng L, Szeto IM, Li T, et al. Association between dietary inflammatory index, C-reactive protein and metabolic syndrome: a cross-sectional study. Nutrients. 2018; 10:831.


13. Shivappa N, Bonaccio M, Hebert JR, Di Castelnuovo A, Costanzo S, Ruggiero E, et al. Association of proinflammatory diet with low-grade inflammation: results from the Moli-sani study. Nutrition. 2018; 54:182–188.


15. Julia C, Assmann KE, Shivappa N, Hebert JR, Wirth MD, Hercberg S, et al. Long-term associations between inflammatory dietary scores in relation to long-term C-reactive protein status measured 12 years later: findings from the Supplémentation en Vitamines et Minéraux Antioxydants (SU.VI.MAX) cohort. Br J Nutr. 2017; 117:306–314.


16. Shivappa N, Hébert JR, Paddock LE, Rodriguez-Rodriguez L, Olson SH, Bandera EV. Dietary inflammatory index and ovarian cancer risk in a New Jersey case-control study. Nutrition. 2018; 46:78–82.


17. Shivappa N, Hébert JR, Zucchetto A, Montella M, Serraino D, La Vecchia C, et al. Dietary inflammatory index and endometrial cancer risk in an Italian case-control study. Br J Nutr. 2016; 115:138–146.


19. Peres LC, Bandera EV, Qin B, Guertin KA, Shivappa N, Hebert JR, et al. Dietary inflammatory index and risk of epithelial ovarian cancer in African American women. Int J Cancer. 2017; 140:535–543.


20. Wells GA, Shea B, O'connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON: Ottawa Hospital Research Institute;2009.
21. The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions, version 5.0.0 (updated February 2008) [Internet]. London: The Cochrane Collaboration;cited 2018 Aug 2. Available from:
http://handbook.cochrane.org/.
22. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7:177–188.


23. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011; 342:d549.

24. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21:1539–1558.


25. Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015; 8:2–10.


26. Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992; 135:1301–1309.


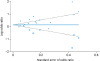
27. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994; 50:1088–1101.


29. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000; 56:455–463.


32. Li D, Hao X, Li J, Wu Z, Chen S, Lin J, et al. Dose-response relation between dietary inflammatory index and human cancer risk: evidence from 44 epidemiologic studies involving 1,082,092 participants. Am J Clin Nutr. 2018; 107:371–388.


33. Wang L, Liu C, Zhou C, Zhuang J, Tang S, Yu J, et al. Meta-analysis of the association between the dietary inflammatory index (DII) and breast cancer risk. Eur J Clin Nutr. Forthcoming. 2018.

34. Vahid F, Shivappa N, Hatami M, Sadeghi M, Ameri F, Jamshidi Naeini Y, et al. Association between dietary inflammatory index (DII) and risk of breast cancer: a case-control study. Asian Pac J Cancer Prev. 2018; 19:1215–1221.


35. Park YM, Shivappa N, Petimar J, Steck S, Hébert J, Sandler D. Association between dietary inflammatory potential and risk of breast cancer: findings from the sister study. FASEB J. 2017; 31:168.1.
36. Niclis C, Tumas N, Shivappa N, Hebert JR, Aballay L, Becaria Coquet J, et al. The inflammatory potential of diet is associated with breast cancer risk in different contexts of urbanization: a multilevel analysis. Ann Nutr Metab. 2017; 71:954.
38. Jalali S, Shivappa N, Hébert JR, Heidari Z, Hekmatdoost A, Rashidkhani B. Dietary inflammatory index and odds of breast cancer in a case-control study from Iran. Nutr Cancer. Forthcoming. 2018.

39. Shivappa N, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, et al. A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr. 2014; 17:1825–1833.


41. Modugno F, Ness RB, Chen C, Weiss NS. Inflammation and endometrial cancer: a hypothesis. Cancer Epidemiol Biomarkers Prev. 2005; 14:2840–2847.


42. Goswami B, Rajappa M, Sharma M, Sharma A. Inflammation: its role and interplay in the development of cancer, with special focus on gynecological malignancies. Int J Gynecol Cancer. 2008; 18:591–599.


43. Hartung DM, Touchette D. Overview of clinical research design. Am J Health Syst Pharm. 2009; 66:398–408.


44. Utsal L, Tillmann V, Zilmer M, Mäestu J, Purge P, Jürimäe J, et al. Elevated serum IL-6, IL-8, MCP-1, CRP, and IFN-γ levels in 10- to 11-year-old boys with increased BMI. Horm Res Paediatr. 2012; 78:31–39.


45. Berbic M, Ng CH, Fraser IS. Inflammation and endometrial bleeding. Climacteric. 2014; 17:Suppl 2. 47–53.


47. Huang WQ, Mo XF, Ye YB, Shivappa N, Lin FY, Huang J, et al. A higher Dietary Inflammatory Index score is associated with a higher risk of breast cancer among Chinese women: a case-control study. Br J Nutr. 2017; 117:1358–1367.


49. Ge I, Rudolph A, Shivappa N, Flesch-Janys D, Hébert JR, Chang-Claude J. Dietary inflammation potential and postmenopausal breast cancer risk in a German case-control study. Breast. 2015; 24:491–496.


50. Shivappa N, Hébert JR, Rosato V, Montella M, Serraino D, La Vecchia C. Association between the dietary inflammatory index and breast cancer in a large Italian case-control study. Mol Nutr Food Res. 2017; 61:1600500.

51. Nagle CM, Ibiebele T, Shivappa N, Hebert JR, DeFazio A, Webb PM. The association between the inflammatory potential of diet and risk of developing, and survival following, a diagnosis of ovarian cancer. Eur J Nutr. Forthcoming. 2018.

55. Shivappa N, Blair CK, Prizment AE, Jacobs DR, Hébert JR. Prospective study of the dietary inflammatory index and risk of breast cancer in postmenopausal women. Mol Nutr Food Res. 2017; 61:1600592.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download