This article has been
cited by other articles in ScienceCentral.
Abstract
Schwannomas are neurogenic tumors, which are among the most varied tumors with respect to morphology, clinical associations, and presentations; they occur in a wide variety of sites. The uterine cervix is a rare site of occurrence and only 15 cases of schwannomas of the uterine cervix, including 5 benign and 10 malignant cases, have been reported to date. Thus, schwannomas of the uterine cervix may pose diagnostic difficulty. Here, we report a case of benign schwannoma of the uterine cervix in a 37-year-old female, who presented with vaginal spotting.
Keywords: Polyp, Nerve sheath neoplasm, Schwann cells
Introduction
Schwannomas are nerve sheath neoplasms arising from Schwann cells [
1]. One-third cases of schwannomas have been reported in the head and neck region [
2]. However, they are also reported to occur at upper and lower extremities, posterior mediastinum, and retroperitoneum [
12]. With respect to the female genital tract, an uncommon location for schwannomas [
1], the uterine cervix is an extremely rare site of occurrence; only 15 related cases (including benign and malignant) have been reported until date [
1]. Therefore, because of their rarity, the diagnosis of these tumors remains a challenge. We present a case of schwannoma of uterine cervix in a 37-year-old female.
Case report
The study patient, who was gravida 2 and para 2, presented with vaginal spotting for 1 week. The abdomen was soft on palpation and did not reveal any lump. Per speculum examination revealed a polyp measuring 1×0.5 cm on the cervical lip. The uterine cavity was normal on transvaginal sonography. Laboratory examinations including whole blood count, liver function tests, coagulation parameters, and thyroid profile tests were within the reference ranges. A clinical diagnosis of cervical leiomyomatous polyp was made. Polypectomy in addition to dilatation and curettage of the endometrial cavity was performed. Tissue samples from the patient were subjected to histopathological examination.
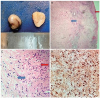
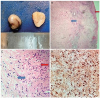
The results revealed that the polyp was grayish white and measured 1×1×0.5 cm (
Fig. 1A). On histological examination, the cervical polyp revealed a well-circumscribed tumor with overlying ectocervical lining (
Fig. 1B). Hypocellular and hypercellular areas were also observed. The Antoni A areas composed of spindle cells arranged in a palisading manner. In Antoni B areas, tumor cells were separated by abundant edematous fluid, giving a myxoid appearance (
Fig. 1C). In addition, mitosis was infrequent. Immunohistochemical (IHC) analysis revealed that the tumor cells were strongly positive for S100 and negative for desmin, smooth muscle actin (SMA), human melanoma black (HMB)-45, and neurofilament protein (
Fig. 1D). Based on histomorphology and immunohistochemistry, the cervical polyp was diagnosed as benign schwannoma, with a negative margin. The endometrial curettage showed endometrial glands in the secretory phase. Because the surgical margin was negative, the patient was discharged and advised regular follow-up. At the 6-month post-operative follow-up, the patient has shown recovery without any recurrence.
Fig. 1
(A) The polyp was grayish white and measured 1×1×0.5 cm. (B) A photomicrograph showing a well-circumscribed tumor (blue arrow) with overlying ectocervical lining (red arrow) (4×, hematoxylin and eosin). (C) A photomicrograph showing cellular Antoni A areas composed of spindle cells (red arrow) and hypocellular Antoni B areas with abundant edematous fluid, which gave a myxoid appearance (blue arrow) (10×, hematoxylin and eosin). (D) The tumor cells were positive for S100 (40×).
Discussion
Schwannomas typically occur in individuals aged 20–50 years, but they may occur at any age and show equal sex predilection [
2]. These tumors are usually present as solitary, painless, and slow-growing mass of variable size [
2]. However, multiple lesions may be seen in association with von-Recklinghausen's neurofibromatosis [
2]. Schwannomas are mostly benign and less than 1% transform to malignancy, known as malignant peripheral nerve sheath tumors (MPNSTs), also reported as “malignant schwannoma,” “neurogenic sarcoma,” and “neurofibrosarcoma” [
1].
The common locations of benign schwannomas are the head and neck regions as well as the distal extremities [
2]. The uterine cervix is an extremely rare location for benign schwannomas, with only 5 cases reported to date (
Table 1). The first case in English was reported by Gwavava and Traub in 1980, but it was reported as early as in 1960 in German [
134]. Patients present with varied presentations, ranging from pain abdomen and nodular swelling in the cervix to being asymptomatic with incidental finding on routine annual pelvic examination [
34567]. Ten cases of malignant schwannomas have been reported in the literature (
Table 1). Malignancy in schwannomas or MPNST typically presents with abnormal vaginal bleeding [
89101112131415]. The patient in the present study presented with a nodular lesion in the cervix (
Table 1). Therefore, a pre-operative diagnosis of this tumor may be challenging because to its rarity as well as the various differential diagnoses, which must be considered by both gynecologists and pathologists. Clinical and histomorphological differential diagnoses of benign schwannomas of the uterine cervix include palisaded leiomyoma, angiomyofibroblastoma, desmoplastic melanoma, and neurofibroma [
7]; IHC analysis plays an important role in the diagnosis. S100 is strongly positive in benign schwannoma, and negative expression for desmin and SMA rules out palisaded leiomyoma and angiomyofibroblastoma [
7]. The negative expression of HMB-45 and neurofilament protein rules out melanoma and neurofibroma, respectively [
7]. In the present case, strong immunoreactivity with S100 and negative immunoreactivity for desmin, SMA, HMB-45, and neurofilament protein helped in confirming the diagnosis.
Table 1
Cases of schwannoma of the uterine cervix reported in literature

|
Authors |
Age (yr) |
Clinical presentation |
Pathological findings |
|
Cid [3] |
- |
- |
Benign schwannosis |
|
Gwavava and Traub [4] |
38 |
Nodular swelling on the anterior lip of cervix |
Benign schwannoma |
|
Terzakis et al. [5] |
47 |
Protruding lesion of the cervix |
Pigmented melanocytic schwannoma |
|
LeMaire et al. [6] |
47 |
Asymptomatic, incidentally found to have mass in the posterior lip of cervix on routine examination |
Benign schwannoma |
|
Tahmasbi et al. [7] |
48 |
Pain abdomen with multiple masses in uterus and cervix |
Benign schwannoma |
|
Sloan [8] |
47 |
Abnormal vaginal bleeding |
Malignant schwannoma |
|
Junge et al. [9] |
41 |
Abnormal vaginal bleeding |
Malignant schwannoma |
|
Keel et al. [10] |
25 |
Two of three cases presented |
Malignant schwannoma (malignant peripheral nerve sheath tumor) |
|
65 |
with abnormal vaginal bleeding |
|
73 |
Polypoid lesions in two cases, one was ulcerated |
|
Lallas et al. [11] |
51 |
Abnormal vaginal bleeding |
Malignant schwannoma |
|
Bernstein et al. [12] |
65 |
Abnormal vaginal bleeding |
Malignant schwannoma |
|
Di Giovannantonio et al. [13] |
27 |
Abnormal vaginal bleeding |
Malignant schwannoma |
|
Kim et al. [14] |
50 |
Polypoid lesion |
Malignant schwannoma (malignant peripheral nerve sheath tumor) |
|
Dong et al. [15] |
45 |
Abnormal vaginal bleeding |
Malignant schwannoma (malignant peripheral nerve sheath tumor) |
|
Present case |
37 |
Nodular swelling on the cervix |
Benign schwannoma |
Surgical excision is recommended in cases of benign schwannoma, which rarely recurs if completely excised [
2]. In the present case, the polyp was excised and the margin was free.
Although the uterine cervix is a rare site for benign schwannomas, it should be considered in the differential diagnosis of cervical masses. Clinically and morphologically, it may mimic other neoplasms, which are more common at this site. Therefore, surgical excision with free margins is the mainstay of treatment.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download