Abstract
Purpose
To evaluate the clinical outcomes of one day small incision lenticule extraction (SMILE), which was performed on the same day as preoperative examinations in myopic patients.
Methods
This study included 163 patients (163 eyes) who underwent SMILE with Visumax from January to June in 2017. We divided the patients into two groups. The one day SMILE group underwent surgery on the same day as the preoperative examinations including dilated fundus examinations. The scheduled group underwent the surgery on a different day. Only the right eye was included in the analysis. Visual acuity and refractive results were compared between groups.
Results
The one day SMILE group included 83 patients and the scheduled SMILE group included 80 patients. At postoperative 1 month, the myopic errors were −0.07 ± 0.43 diopters (D) for the one day SMILE group and −0.09 ± 0.37 D for the scheduled SMILE group (p = 0.81); the astigmatic refractions were −0.48 ± 0.29 D and −0.46 ± 0.28 D, respectively (p = 0.57), the postoperative uncorrected visual acuities were −0.02 ± 0.11 logarithm of the minimum angle of resolution (logMAR) and −0.02 ± 0.11 logMAR, respectively (p = 0.79). At postoperative 6 months, the myopic errors were −0.06 ± 0.42 D for the one day SMILE group and −0.08 ± 0.34 D for the scheduled SMILE group (p = 0.81), and the astigmatic refractions were −0.48 ± 0.25 D and −0.48 ± 0.30 D, respectively (p = 0.99); the postoperative uncorrected visual acuities were −0.04 ± 0.09 logMAR and −0.05 ± 0.07 logMAR, respectively (p = 0.45).
Figures and Tables
Figure 1
Refractive outcomes of the one day SMILE group and scheduled SMILE group. The spherical equivalent of one day SMILE and scheduled SMILE at postoperative 1 month (A). The spherical equivalent of one day SMILE and scheduled SMILE at postoperative 6 months (B). SMILE = small incision lenticule extraction; D = diopters.

Figure 2
Predictability of spherical equivalent correction of the one day SMILE group and scheduled SMILE group. The results of one day SMILE (A) and scheduled SMILE (B) at postoperative 1 month. The results of one day SMILE (C) and scheduled SMILE (D) at postoperative 6 months. SMILE = small incision lenticule extraction; D = diopters.
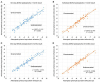
Figure 3
Preoperative and postoperative astigmatic refraction distribution of the one day SMILE group and scheduled SMILE group. Preoperative astigmatic diopters of two groups (A). Astigmatic diopters after the one day SMILE and scheduled SMILE at postoperative 1 month (B). Astigmatic diopters after the one day SMILE and scheduled SMILE at postoperative 6 months (C). SMILE = small incision lenticule extraction; D = diopters.
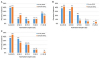
Table 1
Preoperative demographic characteristics of patients who underwent SMILE

Values are presented as mean ± standard deviation (range) unless otherwise indicated.
SMILE = small incision lenticule extraction; D = diopters; BCVA = best corrected visual acuity; logMAR = logarithm of minimum angle of resolution; IOP = intraocular pressure; CCT = central cornea thickness.
*Independent t-test; †Chi-square test.
References
1. Sekundo W, Gertnere J, Bertelmann T, Solomatin I. One-year refractive results, contrast sensitivity, high-order aberrations and complications after myopic small-incision lenticule extraction (ReLEx SMILE). Graefes Arch Clin Exp Ophthalmol. 2014; 252:837–843.


2. Pedersen IB, Ivarsen A, Hjortdal J. Three-year results of small incision lenticule extraction for high myopia: refractive outcomes and aberrations. J Refract Surg. 2015; 31:719–724.


3. Kobashi H, Kamiya K, Igarashi A, et al. Two-years results of small-incision lenticule extraction and wavefront-guided laser in situ keratomileusis for myopia. Acta Ophthalmol. 2018; 96:e119–e126.
4. Reinstein DZ, Archer TJ, Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vis (Lond). 2014; 1:3.



5. Vestergaard A, Ivarsen A, Asp S, Hjortdal JØ. Femtosecond (FS) laser vision correction procedure for moderate to high myopia: a prospective study of ReLEx (R) flex and comparison with a retrospective study of FS-laser in situ keratomileusis. Acta Ophthalmol. 2013; 91:355–362.

6. Ganesh S, Brar S, Arra RR. Refractive lenticule extraction small incision lenticule extraction: a new refractive surgery paradigm. Indian J Ophthalmol. 2018; 66:10–19.



7. Ağca A, Demirok A, Yildirim Y, et al. Refractive lenticule extraction (ReLEx) through a small incision (SMILE) for correction of myopia and myopic astigmatism: current perspectives. Clin Ophthalmol. 2016; 10:1905–1912.



8. Piñero DP, Teus MA. Clinical outcomes of small-incision lenticule extraction and femtosecond laser-assisted wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg. 2016; 42:1078–1093.


9. Seven I, Vahdati A, Pedersen IB, et al. Contralateral eye comparison of SMILE and flap-based corneal refractive surgery: computational analysis of biomechanical impact. J Refract Surg. 2017; 33:444–453.



10. Shetty R, Francis M, Shroff R, et al. Corneal biomechanical changes and tissue remodeling after SMILE and LASIK. Invest Ophthalmol Vis Sci. 2017; 58:5703–5712.


11. Denoyer A, Landman E, Trinh L, et al. Dry eye disease after refractive surgery comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015; 122:669–676.

12. kobashi H, Kamiya K, Shimizu K. Dry eye after small incision lenticule extraction and femtosecond laser-assisted LASIK: meta-analysis. Cornea. 2017; 36:85–91.

13. Xia LK, Ma J, Liu HN, et al. Three-year results of small incision lenticule extraction and wavefront-guided femtosecond laser-assisted laser in situ keratomileusis for correction of high myopia and myopic astigmatism. Int J Ophthalmol. 2018; 11:470–477.



14. Shen Z, Shi K, Yu Y, et al. Small incision lenticule extraction (SMILE) versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia: a systematic review and meta-analysis. PLoS ONE. 2016; 11:e0158176.

15. Lam DS, Fan DS, Chan WM, et al. Prevalence and characteristics of peripheral retinal degeneration in chinese adults with high myopia: a cross-sectional prevalence survey. Optom Vis Sci. 2005; 82:235–238.


16. Arevalo JF. Retinal complications after laser-assisted in situ keratomileusis (LASIK). Curr Opin Ophthalmol. 2004; 15:184–191.


17. Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol. 2003; 136:155–160.

18. Lin J, Xie X, Du X, et al. Incidence of vitreoretinal pathologic conditions in myopic eyes after laser in situ keratomileusis. Zhonghua Yan Ke Za Zhi. 2002; 38:546–549.

19. Ghosh S, Couper TA, Lamoureux E, et al. Evaluation of iris recognition system for wavefront-guided laser in situ keratomileusis for myopic astigmatism. J Cataract Refract Surg. 2008; 34:215–221.


20. Pierro L, Camesasca FI, Mischi M, Brancato R. Peripheral retinal changes and axial myopia. Retina. 1992; 12:12–17.


21. Kirker GE, McDonald DJ. Peripheral retinal degeneration in high myopia. Can J Ophthalmol. 1971; 6:58–61.

22. Lin SC, Tseng SH. Prophylactic laser photocoagulation for retinal breaks before laser in situ keratomileusis. J Refract Surg. 2003; 19:661–665.


23. Wilkes SR, Beard CN, Kurland LT, et al. The incidence of retinal detachment in Rochester, Minnesota, 1970–1978. Am J Ophthalmol. 1982; 94:670–673.


24. Arevalo JF, Ramirez E, Suarez E, et al. Rhegmatogenous retinal detachment in myopic eyes after laser in situ keratomileusis. Frequency, characteristics, and mechanism. J Cataract Refract Surg. 2001; 27:674–680.

25. Wright KW, Strube YN. Pediatric ophthalmology and strabismus. 3rd ed. New York: Oxford University Press;2012. p. 92.
26. Kim WK, Ryu IH, Lee IS, et al. Comparison of postoperative results of one day laser-assisted in-situ keratomileusis, laser-assisted sub-epithelial keratectomy surgery, and conventional surgery. J Korean Ophthalmol Soc. 2018; 59:410–418.
27. Chan TCY, Ng ALK, Cheng GPM, et al. Effect of the learning curve on visual and refractive outcomes of small-incision lenticule extraction. Cornea. 2017; 36:1044–1050.


28. Kang DSY, Lee H, Reinstein DZ, et al. Comparison of the distribution of lenticule decentration following SMILE by subjective patient fixation or triple marking centration. J Refract Surg. 2018; 34:446–452.

29. Lee H, Roberts CJ, Arba-Mosquera S, et al. Relationship between decentration and induced corneal higher-order aberrations following small-incision lenticule extraction procedure. Invest Ophthalmol Vis Sci. 2018; 59:2316–2324.


30. Titiyal JS, Kaur M, Rathi A, et al. Learning curve of small incision lenticule extraction: challenges and complications. Cornea. 2017; 36:1377–1382.


31. Steinwender G, Shajari M, Mayer WJ, et al. Impact of a displaced corneal apex in small incision lenticule extraction. J Refract Surg. 2018; 34:460–465.


32. Jun I, Kang DSY, Reinstein DZ, et al. Clinical outcomes of SMILE with a triple centration technique and corneal wavefront-guided transepithelial PRK in high astigmatism. J Refract Surg. 2018; 34:156–163.


33. Zhao F, Han T, Chen X, et al. Minimum pupil in pupillary response to light and myopia affect disk halo size: a cross-sectional study. BMJ Open. 2018; 8:e019914.

34. De Ortueta D, Arba-Mosquera S. Laser in situ keratomileusis for high hyperopia with corneal vertex centration and asymmetric offset. Eur J Ophthalmol. 2017; 27:141–152.


35. Narváez J, Brucks M, Zimmerman G, et al. Intraoperative cyclorotation and pupil centroid shift during LASIK and PRK. J Refract Surg. 2012; 28:353–357.


36. Damgaard IB, Ang M, Farook M, et al. Intraoperative patient experience and postoperative visual quality after smile and lasik in a randomized, paired-eye, controlled study. J Refract Surg. 2018; 34:92–99.


37. Ganesh S, Gupta R. Comparison of visual and refractive outcomes following femtosecond laser-assisted LASIK with SMILE in patients with myopia or myopic astigmatism. J Refract Surg. 2014; 30:590–596.

38. Riau AK, Angunawela RI, Chaurasia SS, et al. Effect of different femtosecond laser-firing patterns on collagen disruption during refractive lenticule extraction. J Cataract Refract Surg. 2012; 38:1467–1475.


39. Wei S, Wang Y, Wu D, et al. Ultrastructural changes and corneal wound healing after SMILE and PRK procedures. Curr Eye Res. 2016; 41:1316–1325.


40. Han T, Zhao J, Shen Y, et al. A three-year observation of corneal backscatter after small incision lenticule extraction (SMILE). J Refract Surg. 2017; 33:377–382.


41. Agca A, Ozgurhan EB, Yildirim Y, et al. Corneal backscatter analysis by in vivo confocal microscopy: fellow eye comparison of small incision lenticule extraction and femtosecond laser-assisted LASIK. J Ophthalmol. 2014; 2014:265012.

42. Yao P, Zhao J, Li M, et al. Microdistortions in bowman’s layer following femtosecond laser small incision lenticule extraction observed by fourier-domain OCT. J Refract Surg. 2013; 29:668–674.


43. Agca A, Ozgurhan EB, Demirok A, et al. Comparison of corneal hysteresis and corneal resistance factor after small incision lenticule extraction and femtosecond laser-assisted LASIK: a prospective fellow eye study. Cont Lens Anterior Eye. 2014; 37:77–80.


44. Kamiya K, Shimizu K, Igarashi A, Kobashi H. Visual and refractive outcomes of femtosecond lenticule extraction and small incision lenticule extraction for myopia. Am J Ophthalmol. 2014; 157:128–134.

45. Son GS, Lee SC, Lim TH. Clinical outcomes of small incision lenticule extraction including visual qaulity analysis. J Korean Ophthalmol Soc. 2016; 57:562–567.
46. Bueeler M, Mrochen M, Seiler T. Maximum permissible lateral decentration in aberration-sensing and wavefront-guided corneal ablation. J Cataract Refract Surg. 2003; 29:257–263.


47. Mrochen M, Kaemmerer M, Mierdel P, Seiler T. Increased higher-order optical aberrations after laser refractive surgery: a problem of subclinical decentration. J Cataract Refract Surg. 2001; 27:362–369.
48. Wang L, Koch DD. Residual higher-order aberrations caused by clinically measured cyclotorsional misalignment or decentration during wavefront-guided excimer laser corneal ablation. J Cataract Refract Surg. 2008; 34:2057–2062.


49. Okamoto S, Kimura K, Funakura M, et al. Comparison of myopic LASIK centered on the coaxially sighted corneal light reflex or line of sight. J Refract surg. 2009; 25:10 Suppl. S944–S950.

50. Reinstein DZ, Archer TJ, Gobbe M. Is topography-guided ablation profile centered on the corneal vertex better than wavefront-guided ablation profile centered on the entrance pupil? J Refract Surg. 2012; 28:139–143.


51. Arbelaez MC, Vidal C, Arba-Mosquera S. Clinical outcomes of corneal vertex versus central pupil references with aberration-free ablation strategies and LASIK. Invest Ophthalmol Vis Sci. 2008; 49:5287–5294.


52. Reinstein DZ, Gobbe M, Gobbe L, et al. Optical zone centration accuracy using corneal fixation-based SMILE compared to eye tracker-based femtosecond laser-assisted LASIK for myopia. J Refract Surg. 2015; 31:586–592.


53. Steinwender G, Shajari M, Mayer WJ, et al. Impact of a displaced corneal apex in small incision lenticule extraction. J Refract Surg. 2018; 34:460–465.


54. Uozato H, Guyton DL. Centering corneal surgical procedures. Am J Ophthalmol. 1987; 103(3 Pt 1):264–275.


55. Yang Y, Thompson K, Burns SA. Pupil location under mesopic, photopic, and pharmacologically dilated conditions. Invest Ophthalmol Vis Sci. 2002; 43:2508–2512.


56. Erdem U, Muftuoglu O, Gundogan FC, et al. Pupil center shift relative to the coaxially sighted corneal light reflex under natural and pharmacologically dilated conditions. J Refract Surg. 2008; 24:530–538.


57. Schruender SA, Fuchs H, Spasovski S, Dankert A. Intraoperative corneal topography for image registration. J Refract Surg. 2002; 18:S624–S629.

58. Alió del Barrio JL, Vargas V, Al-Shymali O, Alió JL. Small incision lenticule extraction (SMILE) in the correction of myopic astigmatism: outcomes and limitations - an update. Eye Vis (Lond). 2017; 4:26.



59. Hall RC, Rosman M, Chan C, et al. Patient and surgeon experience during laser in situ keratomileusis using 2 femtosecond laser systems. J Cataract Refract Surg. 2014; 40:423–429.


60. Pedersen IB, Ivarsen A, Hjortdal J. Changes in astigmatism, densitometry, and aberrations after SMILE for low to high myopic astigmatism: a 12-month prospective study. J Refract Surg. 2017; 33:11–17.


61. Swami AU, Steinert RF, Osborne WE, White AA. Rotational malposition during laser in situ keratomileusis. Am J Ophthalmol. 2002; 133:561–562.


63. Ganesh S, Brar S, Pawar A. Results of intraoperative manual cyclotorsion compensation for myopic astigmatism in patients undergoing small incision lenticule extraction (SMILE). J Refract Surg. 2017; 33:506–512.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download