INTRODUCTION
Intussusception refers to the invagination of part of the intestine into the distal bowel and is the most common cause of acute intestinal obstruction in infants and young children [
1]. Intussusception is an emergent condition, requiring prompt diagnosis and management, as obstruction of the blood supply to the intestine may result in bowel infarction, perforation, and even death [
1].
In most cases, intussusceptions are idiopathic in nature [
23], however, recurrence is known to be associated with specific pathologies, including Meckel's diverticulum, duplication, polyps, and tumors, particularly in adults [
2345]. To date, definitive or reliable risk factors for recurrence, other than anatomical features, have not been identified [
67].
Awareness of the recurrence of intussusceptions and, therefore, early diagnosis, is often challenging for pediatricians in a clinical setting. Accordingly, the aim of this study was to identify the clinical features and risk factors of recurrent intussusception, beyond the anatomical points previously identified, which would allow clinicians to identify patients who are at an increased risk for recurrence after a primary episode. Providing a clinical index for the risk of intussusception recurrence would allow pediatricians to plan a more appropriate course of management and follow-up for these patients.
MATERIALS AND METHODS
We retrospectively analyzed the medical records of 137 pediatric patients who were diagnosed with intussusception and treated at Dongsan Medical Center between March 2015 and June 2017. This study was approved by our Institutional Review Board (No. 2018-07-023).
In all cases, the final diagnosis of intussusception was confirmed by medical imaging, normally using abdominal ultrasonography (USG), with abdominal computed tomography (CT) and barium enema required in some cases. Once the diagnosis was made, informed consent was obtained from the child's parents or guardians, before proceeding with the reduction procedure.
The reduction was performed using a water enema under ultrasound guidance in most cases, with a barium enema used in cases in which a water enema was not sufficient. Both water and barium enemas were performed from a height of 100–120 cm above the procedure table. A height of 100 cm yields an enema pressure of 84.4 mmHg and a normal saline pressure of 63.7 mmHg. In cases in which a reduction by pressure enema failed or if the patient showed any signs of perforation or cardiovascular compromise, we proceeded with emergent surgery.
Recurrent intussusception was defined as recurrence of the invagination after the initial reduction, regardless of the procedure used (water or barium enema, or surgery). These cases were classified into the recurrence group. Cases of successful reduction without recurrence were classified into the non-recurrence group, providing a control reference in our analysis of risk factors for recurrence.
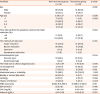
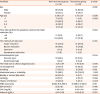
The demographic factors at baseline were compared between the non-recurrence and recurrence group. The distribution incidence by month, the time interval between symptom onset and the reduction, and the reduction method used were also compared between the 2 groups. The rate of recurrence by age was also calculated in the recurrence group. The presence or absence of the following clinical symptoms was also compared between the 2 groups: vomiting, abdominal pain, irritability, hematochezia (or currant jelly stool), and lethargy. The infection history was also investigated, including fever and respiratory symptoms, such as coughing and rhinorrhea, and diarrhea. The size of the invagination was measured by abdominal ultrasound or CT. Blood tests were performed at the initial examination to determine the white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and levels of C-reactive protein (CRP), and albumin. The presence or absence of pathologic factors was also evaluated, and the surgical method used, when needed, was investigated. Descriptive statistics for continuous variables were reported as the mean±standard deviation, with categorical and dichotomous variables reported using counts and percentages. Between-group differences were evaluated using a χ2 test, Fisher's exact test or Student t-test, as appropriate for the data type, and logistic regression was used to identify independent predictive variables. A p-value of <0.05 was considered significant for all tests.
All statistical analyses were conducted using SPSS statistics 21.0 (SPSS Inc., Chicago, IL, USA).
DISCUSSION
Recurrent intussusception was first reported by Clark and Bunts in 1900 and several cases have been reported since then, with rates of ranging between 2% and 20% [
68910], and between 7.1% and 11% in Koreans, specifically [
1112]. Although the recurrence of intussusceptions is considered to be spontaneous [
13], specific predisposing factors have been identified, including Peutz-Jeghers syndrome or Meckel's diverticulum, both of which are associated with a relatively high recurrence rate [
810]. Unlike in adults, intussusception in infants and children is rarely associated with specific anatomical factors [
414]. Still, little is known about the factors associated with intussusception recurrence in infants and children and reports have been widely inconsistent.
With regard to the effect of the method of reduction on recurrence, a rate of 1% to 3% has been reported after open manual reduction [
15], compared to 10% to 15% after non-operative reduction [
16]. It is likely that internal adhesions resulting from scarring after the surgical procedure lowered the risk of invagination recurrence [
1617]. Among non-operative methods, the rate of recurrence has been reported to be lower for reductions using air or saline than for barium enemas [
8]. However, in our study, we did not identify an effect of the method of reduction on the rate of recurrence.
The intussusception type was also not associated with the recurrence of intussusception. We found that most of the intussusceptions were ileocolic, with only 1 small bowel case. Small bowel intussusception is known to be rare, representing about 1.68% to 17% of all intussusceptions [
18]. This agrees with our result, which showed only 1 small bowel intussusception (0.7%) among all the cases. This could have resulted from the nature of the small bowel intussusceptions, which tend to spontaneously resolve if they are small, and also from the regional characteristic that intussusception patients would have been dispersed to one of the many tertiary medical centers near our center.
In their review of 127 cases of recurrent intussusception in pediatric patients, Wang et al. [
19] reported the rate of recurrence to be higher for patients presenting with intussusceptions at >1 year of age than those diagnosed at ≤1 year. Guo et al. [
10] reported a rate of recurrence of 67.5% among patients older than 1 year of age at the time of the first presentation with an intussusception. These results are consistent with our findings of a higher rate of recurrence among patients over the age of 1 year at the time of the first diagnosis (95.7%) compared to those diagnosed before the age of 1 year (4.3%,
p=0.018). We also identified the recurrence rate to be higher among children older than 3 years of age at the first incidence of intussusception (45.5%) compared to a diagnosis obtained before the age of 3 years (17.5%,
p=0.006). Therefore, across all studies, the rate of recurrence was higher among children who first developed intussusception at an older age, with age >1 year identified as an independent risk factor for recurrence in our study.
The clinical symptoms related to intussusceptions recurrence have previously been studied. In their review of 85 cases, Bines et al. [
20] reported the risk of recurrence to be higher for cases of invagination on the right side of the abdomen, compared to the left. We did not find an effect of the side of the lesion on the rate of recurrence nor of the size of the mass measured by USG or CT. In their evaluation of 23 cases, Champoux et al. [
21] reported that, compared to patients in the non-recurrence group, symptoms among patients in the recurrence group were milder and of shorter duration. Similarly, Guo et al. [
10] reported milder vomiting and shorter duration among patients in the recurrence group compared to the non-recurrence group. Eklöf and Reiter [
22] also reported more striking clinical symptoms in patients in the non-recurrence than the recurrence group, although they did not report this between-group difference to be significant. These findings are consistent with ours, with fewer incidences of vomiting as an initial symptom in the recurrence than in the non-recurrence group. A history of infection, which included symptoms and signs of fever, coughing, rhinorrhea, and diarrhea, were also significantly higher in the non-recurrence group than in the recurrence group in this study. Moreover, we found that the incidence of hematochezia or currant jelly stool was significantly lower in the recurrence group than in the non-recurrence group. Therefore, the severity of clinical symptoms or signs of infection at the time of presentation may not be positively related to future recurrent intussusceptions. As such, it is important for clinicians to educate parents (or caregivers) on the possibility of recurrence after a successful reduction, even if presenting symptoms or signs are mild. It is equally important for clinicians to be aware of the possibility for recurrence, despite mild symptoms or signs.
Those findings, milder symptoms and a lower rate of previous infections in the non-recurrence group, are thought to be related to the different age distributions between the groups. There were more younger children, younger than 1 year specifically, in the non-recurrence group in our study. Considering that gastrointestinal or respiratory infections are more common in younger ages, especially in neonates and infants [
23], it is reasonable that the 2 factors, age >1 year and no infection history, identified as significant predictive factors in our study, should be closely related to each other.
The different rate of infections according to age probably resulted from the natural immunological development process in humans. The innate, adaptive immune system and the intestinal function and environment, including gut microbiota, are weaker and immature in neonates and infants, which make them susceptible to various infections [
23]. And infections with some pathogens have been reported as causes of intussusceptions, by creating a leading point of intestinal lymphoid hyperplasia [
2024252627]. The different incidence of intussusceptions between the age groups could be explained, although incompletely, by the theory of immune development status, infection rates, and lymphoid hyperplasia, however, it doesn't completely explain why the recurrence rate is higher in older age-onset intussusception cases without pathologic anatomical leading points. Recently, some investigations into the pathophysiology of intussusceptions provided experimental evidence that lipopolysaccharide-induced intussusception was mediated by innate immunity, such as by toll-like receptor 4 and phagocytes, and by intestinal hypomotility [
2829]. Those newer theories could provide clues to the different mechanisms of intussusceptions, including the recurrence difference between ages, and further investigations are warranted.
Few studies have examined the differences in blood test results between patients with and without recurrence of intussusception. Ravitch [
30] reported a WBC >10,000/mm
3 to be predictive of an unfavorable prognosis. Considering that intussusception can cause edema and inflammation due to stasis in the mesenteric blood flow, we evaluated 4 blood serum markers: WBC count, ESR, CRP levels, and albumin. Of these, only the CRP levels were different between the 2 groups, with higher levels found in the recurrence compared to the non-recurrence group (
p=0.024). CRP is an acute phase reactant which is found non-specifically in inflammatory states (including infection and autoimmune diseases) and with tissue damage (including trauma, surgery, myocardial infarction, and tumors). Within the context of intussusceptions, inflammation and tissue damage could result from the stasis in mesenteric blood flow. As such, it is logical that an increase in CRP would be detected with recurrent intussusceptions.
The time interval from symptom onset to the initial reduction was significantly longer (≥48 hours) in the recurrence than in the non-recurrence group in our study (
p=0.034), suggesting that a longer delay caused progression of the inflammation and mucosal edema at the site of intestinal invagination. The local progression in inflammation and edema could increase the time required to achieve a reduction, as well as increase the risk of an incomplete reduction and elevate the ESR level, which is an inflammatory marker, in the ≥48 hours group compared to the <48 hours group (13.83±12.35 mm/hr and 29.79±16.16 mm/hr, respectively;
p=0.031). Fallon et al. [
31] reported that abdominal symptoms lasting more than 2 days were significantly associated with the initial failure of an enema reduction and the need for surgical management. For patients who delay more than 48 hours before seeking care, clinicians should be more aware of possible difficulties during the reduction process, as well as the higher risk of recurrence.
With regard to the underlying cause of intussusceptions, sub-serous lymphoid hyperplasia has commonly been reported among cases reported to be idiopathic in nature, with this hyperplasia possibly being an anatomical susceptibility for invagination [
12]. In our study group, enlarged LNs were observed on USG or CT in about half of our patients (n=66, 46.8%). Although previous studies have reported an association between respiratory or enteric infections and the incidence of intussusceptions [
323334], we did not identify a significant association between isolated pathogens and enlarged LNs and no significant difference in the presence of enlarged LNs between the recurrence and non-recurrence group. Since we did not test for specific pathogens in all patients, some interpretations of our study are limited. Similarly, although anatomical factors, such as Meckel's diverticulum, polyps, or lymphoma have been associated with intussusceptions [
616], we did not identify pathologic factors (other than enlarged LNs) in our study group. Considering that the evaluations performed, including CT, endoscopy, scintigraphy, or exploratory surgery, were not conducted routinely in the recurrence cases in this study, conclusions about the association between pathologic anatomical leading points and the recurrence of intussusception are also limited.
In conclusion, we identified that intussusceptions occurring after the age of 1 year, a delay between symptom onset and initial reduction ≥48 hours, CRP levels >0.5mg/dL, the absence of hematochezia or currant jelly stool, and no history of infection were factors significantly associated with recurrent intussusceptions. Among these factors, age >1 year at the first diagnosis and no history of infection were retained as independent predictors of recurrence on multivariate analysis. Children with these risk factors require close observation and a good educational program should be provided to parents to increase their awareness of a possible recurrence.