2. Reindl R, Harvey EJ, Berry GK, Rahme E. Intramedullary versus extramedullary fixation for unstable intertrochanteric fractures: a prospective randomized controlled trial. J Bone Joint Surg Am. 2015; 97:1905–1912. PMID:
26631990.
5. Müller ME, Allgöwer M, Schneide R, Willenegger H. Manual of internal fixation: techniques recommended by the AO-ASIF group. 3rd ed. Berlin: Springer-Verlag;1991.
6. Sandifer PA, Hulick RM, Graves ML, et al. Extent and morbidity of lateralization of a trochanteric fixation nail blade. Orthopedics. 2017; 40:e886–e891. PMID:
28817157.

7. Stern R, Lübbeke A, Suva D, Miozzari H, Hoffmeyer P. Prospective randomised study comparing screw versus helical blade in the treatment of low-energy trochanteric fractures. Int Orthop. 2011; 35:1855–1861. PMID:
21387175.

8. Li C, Xie B, Chen S, Lin G, Yang G, Zhang L. The effect of local bone density on mechanical failure after internal fixation of pertrochanteric fractures. Arch Orthop Trauma Surg. 2016; 136:223–232. PMID:
26626056.

9. Fang C, Lau TW, Wong TM, Lee HL, Leung F. Sliding hip screw versus sliding helical blade for intertrochanteric fractures: a propensity score-matched case control study. Bone Joint J. 2015; 97-B:398–404. PMID:
25737525.
10. Goffin JM, Pankaj P, Simpson AH, Seil R, Gerich TG. Does bone compaction around the helical blade of a proximal femoral nail anti-rotation (PFNA) decrease the risk of cut-out?: A subject-specific computational study. Bone Joint Res. 2013; 2:79–83. PMID:
23673407.
11. Huang X, Leung F, Liu M, Chen L, Xu Z, Xiang Z. Is helical blade superior to screw design in terms of cut-out rate for elderly trochanteric fractures? A meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol. 2014; 24:1461–1468. PMID:
24557412.

12. Li S, Chang SM, Niu WX, Ma H. Comparison of tip apex distance and cut-out complications between helical blades and lag screws in intertrochanteric fractures among the elderly: a meta-analysis. J Orthop Sci. 2015; 20:1062–1069. PMID:
26481124.
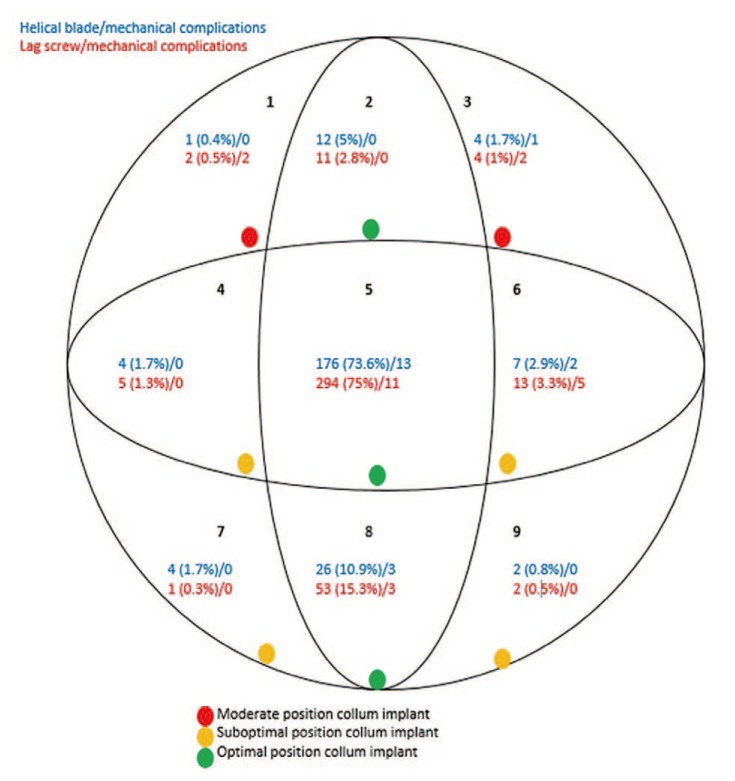
13. Caruso G, Bonomo M, Valpiani G, et al. A six-year retrospective analysis of cut-out risk predictors in cephalomedullary nailing for pertrochanteric fractures: Can the tip-apex distance (TAD) still be considered the best parameter? Bone Joint Res. 2017; 6:481–488. PMID:
28790037.
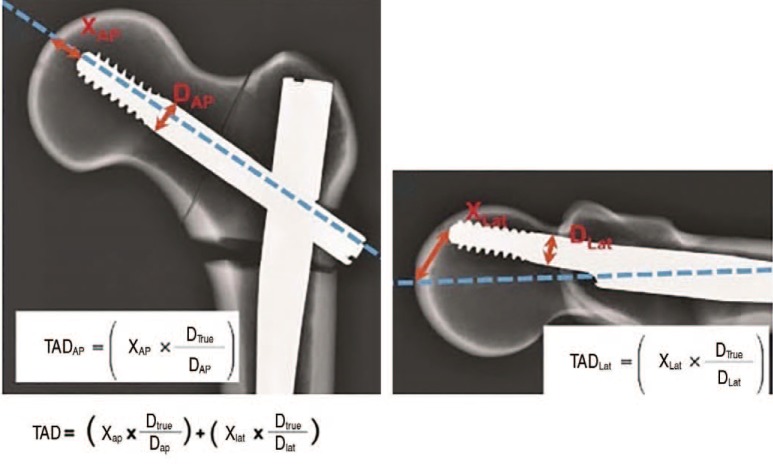
14. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995; 77:1058–1064. PMID:
7608228.

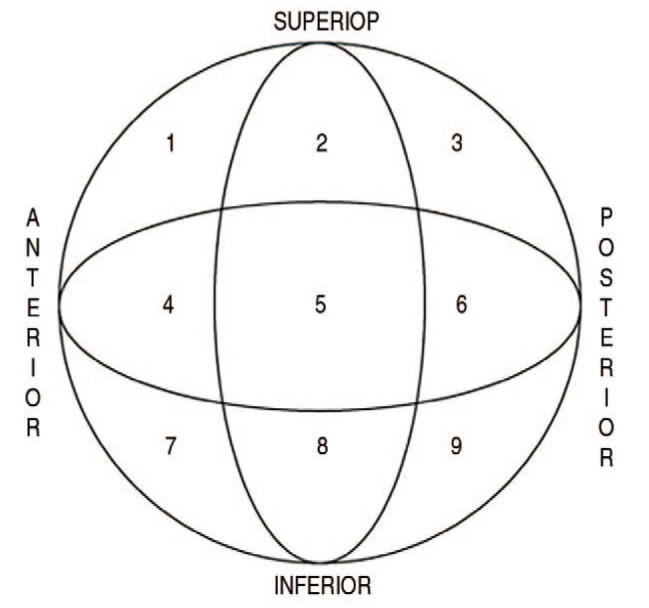
15. Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959; 41-A:1399–1408. PMID:
13849408.

17. Liu W, Zhou D, Liu F, Weaver MJ, Vrahas MS. Mechanical complications of intertrochanteric hip fractures treated with trochanteric femoral nails. J Trauma Acute Care Surg. 2013; 75:304–310. PMID:
23887564.

19. Zehir S, Zehir R, Zehir S, Azboy İ, Haykir N. Proximal femoral nail antirotation against dynamic hip screw for unstable trochanteric fractures; a prospective randomized comparison. Eur J Trauma Emerg Surg. 2015; 41:393–400. PMID:
26037995.

20. Kerremans MS, van Langelaan EJ, Apachitei I. Vermoeidheidsfractuur van de helical blade van een Proximal Femoral Nail Antirotation. Ned Tijdschr Orthop. 2010; 17:117–121.
21. Flores SA, Woolridge A, Caroom C, Jenkins M. The utility of the tip-apex distance in predicting axial migration and cutout with the trochanteric fixation nail system helical blade. J Orthop Trauma. 2016; 30:e207–e211. PMID:
26655519.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download