INTRODUCTION
Morbihan disease (MD) is a rare form of rosacea that presents with chronic erythema and solid oedema on the upper half of the face. A diagnosis of MD can be made only after eliminating diseases that are similar in terms of clinical and histopathological presentation. The cause of MD remains unclear and no standardized treatment is yet available. MD often tends to be recalcitrant to therapies commonly used to treat rosacea, including systemic corticosteroids, antibiotics, isotretinoin, and topical regimens. Thus, surgical interventions have been attempted but most cases have exhibited unsatisfactory responses. We treated six patients with extreme eyelid lymphoedema without any other cutaneous manifestation. Surgical eyelid reduction was performed in all patients, because ptosis and narrowing of the visual field were the major complaints. Histopathological tests revealed various extents of perivascular and perifollicular inflammation, and dermal oedema. After surgery, patients with severe inflammatory cell infiltration (including mast cells) exhibited a tendency toward recurrence. Other patients with severe dermal oedema exhibited better responses to surgical reduction, and thus no recurrence. We propose that MD should be included in the differential diagnosis of persistent, chronic eyelid oedema even if eyelid oedema is the only manifestation; the histological features may aid in the selection of appropriate therapeutic strategies. We suggest that eyelid reduction surgery can be a useful treatment option for MD patients when there is no massive mast cell infiltration.
MD, also known as rosacea lymphoedema, is a rare entity characterized by persistent lymphoedema of the upper half of the face
1. Although an association with rosacea has been suggested, the underlying pathogenic mechanism remains unclear. We treated six patients with extensive non-pitting eyelid lymphoedema and without any other symptom of rosacea. Herein, we describe their notable clinical features, histopathological findings, and treatment outcomes.
CASE REPORT
We retrospectively studied six patients who presented in 2015 and 2016 with eyelid MD; all exhibited persistent, extensive eyelid oedema requiring surgical eyelid reduction. We received the patient's consent form about publishing all photographic materials. Their clinical details, including age and sex, symptoms, disease duration, any previous history of rosacea or any other dermatosis, histopathological findings, and treatment outcomes are summarized in
Table 1.
Our case series consisted of six Koreans aged 42 to 73 years. Disease duration ranged from 8 months to 3 years. The eyelids (both) were the only areas involved in all patients, none of whom had any previous history of rosacea or any other dermatosis. Laboratory data (including antinuclear antibody levels) were normal in all six patients. Head computed tomographic data were also normal except for diffuse infiltration into both eyelids. All patients complained of persistent eyelid oedema, accompanied by narrowing of the visual field; they underwent surgical eyelid reduction followed by lymphatic drainage (
Fig. 1A~C).
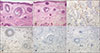
Diagnoses were based on characteristic clinical features and histopathological data obtained from the surgically excised specimens. All specimens were stained with hematoxylin and eosin, and tagged antibodies against CD68 and CD117. Histopathologically, all patients exhibited dermal oedema with perivascular and perifollicular inflammatory cell infiltration (
Fig. 2). However, the histological features were of two different types. Three patients exhibited severe perivascular and perifollicular inflammatory cell infiltration, including of lymphohistiocytes and many mast cells. In contrast, severe dermal oedema, interface dermatitis, and sun damage were the major findings in two patients. The final patient exhibited mixed histological features with moderate dermal oedema and moderateto-severe inflammatory lymphohistiocytic infiltration with abundant mast cells.
All six patients underwent surgical reduction of the eyelids and levator muscles followed by lymphatic drainage. All showed marked improvement (
Fig. 1D~F). Two patients (no. 1 and 2) did not experience any recurrence at that time, and were satisfied with their results. However in three cases (no. 4~6), recurrence developed by the 6-month follow-up. One patient (no. 3) felt that surgery had afforded significant improvement, but developed slow intermittent swelling of both eyelids, although the symptoms were much less bothersome than previously. We commenced oral doxycycline at 200 mg/day; the symptoms were gradually relieved and observation is continuing. Interestingly, the three patients who experienced recurrences were of the histological type associated with severe perivascular and perifollicular inflammatory cell infiltration, including of lymphohistiocytes and many mast cells. The two patients who did not experience recurrence were of the other histological type, characterized by severe dermal oedema and sun damage. The patient who developed intermittent eyelid swelling after surgery had mixed histological features.
DISCUSSION
MD was first reported by Degos et al.
2 in 1957. Clinically, the manifestations usually include firm, non-pitting oedema and erythema, particularly of the glabella, eyelids, forehead, nose, and cheeks
1. Patients often have no subjective symptoms (itching or pain), or only mild symptoms, but eyelid lymphoedema is commonly accompanied by narrowing of the visual field and ptosis
3. In severe cases, the ptosis can be almost complete. Although MD is occasionally regarded as a rare complication of chronic rosacea associated with ocular involvement, MD can occur without any symptoms of rosacea
4. Thus, it is unclear whether MD should be considered as a standalone condition, or a complication caused by rosacea
135.
No histopathological study on MD has yet appeared. Generally, histopathological findings include dermal oedema, vascular hyperplasia and dilatation, perifollicular fibrosis, and perivascular and perifollicular inflammatory cell infiltration (lymphocytes, with occasional neutrophils, eosinophils, mast cells, and plasma cells)
14. However, MD has no known pathognomonic histological feature, and diagnosis thus remains difficult, usually being made after exclusion of various conditions that are similar in appearance, such as dermatomyositis, systemic lupus erythematosus, and chronic actinic dermatitis
3.
All of our patients presented with extreme eyelid oedema but no other lesion, and they all considered the ptosis and visual field narrowing to be major problems; we thus performed eyelid reduction surgery. The clinical manifestations were very similar among the patients, so we could not predict the histological differences between them. However, histopathological examination showed that the MD was of two different histological types, one of which was associated with severe perivascular and perifollicular inflammation with abundant mast cells; and the other with severe dermal oedema, interface dermatitis, and sun damage. One patient had a mixed histological pattern with both dermal oedema and inflammation. The treatment outcomes differed somewhat by histological type. The inflammationpredominant MD was associated with recurrence but the dermal oedema-predominant type was not.
The pathogenesis of MD remains unknown. Nagasaka et al.
1 suggested that closure of lymphatic vessels caused by granulomatous infiltration might explain the oedema. Jansen and Plewig
6 observed infiltration of mast cells around lymphatic vessels, and suggested that such cells might play an important role in disease development, although mast cell infiltration is not a consistent feature of MD
1. Mast cells have been shown to be upregulated in the rosacea lesion. Recently, Mascarenhas et al.
7 suggested that TRPV4 played an important role in LL-37-driven mast cell activation. Although the wider pathological implications are still not clearly understood, mast cells may partly explain the pathogenesis and clinical diversity of rosacea. In addition, Aroni et al.
8 suggested that mast cell numbers were associated with disease duration. Mast cells were thought to contribute significantly to lesional persistence, and functional endothelial compromise. Thus, we assumed that these features might trigger specific forms of rosacea such as MD.
Treatment of MD is often difficult; no standard regimen has yet emerged. Systemic corticosteroids, e.g. tetracycline, thalidomide, and isotretinoin are often used, but most cases exhibit a chronic refractory course and inadequate response
9. Surgery is also possible, but recurrence is common
10. MD associated with massive mast cell infiltration has been treated with long-term oral antibiotics
51112. Fujimoto et al.
11 suggested that the extent of response to tetracycline was associated with the degree of mast cell infiltration. Further study of the role played by mast cells in pathogenesis and prognosis is required; the fact that the disease responds to tetracycline does indeed suggest that mast cells play a particular role. We noted no recurrence in patients whose principal histological feature was dermal oedema. However, patients with abundant mast cell infiltration experienced recurrence. The degree of inflammation may be partially related to treatment outcomes, but we thought it important to explore the influence of mast cell infiltration.
Shim et al.
13 reported a case of MD in Korea, the patient was successfully treated with doxycycline and colchicine over 7 months. No recurrence was detected after 14 months of follow-up. To the best of our knowledge, this is the only reported case of MD to date in Korea.
In summary, we report six MD cases in whom extreme eyelid oedema was the only symptom. We observed two histologically different patterns that seemed to affect the treatment outcome after identical surgery. We propose that MD should be included in the differential diagnosis of persistent, chronic eyelid oedema; the histological features may aid in the choice of an appropriate therapeutic strategy. Eyelid reduction surgery may be a useful treatment option for MD without massive mast cell infiltration.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download