INTRODUCTION
Hand eczema (HE) is a common skin disorder, with an annual prevalence of 7%~12%
12. Some cases of HE are attributed to exposures to irritants or allergens, or previous or concurrent skin disease involving the skin barrier function like atopic dermatitis and are called exogenous HE
3. However, some cases of HE do not have any causative factors, i.e., endogenous HE. HEs are frequently refractory to conventional treatment and take a chronic relapsing course
34.
Palmoplantar pustulosis (PPP) is another bothersome skin disorder that is still under debate whether it is a spectrum of psoriasis or a separate entity
5. In practice, PPP is difficult to distinguish from HE, especially vesicular HE, namely pompholyx, because they have similar clinical features as well as similar histological features
6. PPP is also difficult to treat and is frequently resistant to topical and systemic treatments
7.
Recently, several studies have demonstrated the efficacy and safety of oral alitretinoin in refractory HE
891011. On the other hand, the efficacy of alitretinoin in PPP is still controversial
1213. This study aimed to investigate the efficacy and safety of oral alitretinoin in HE and PPP and factors which affect the response of the two disorders to alitretinoin.
MATERIALS AND METHODS
A retrospective review of the electronic medical records from SMG-SNU Boramae Medical Center was undertaken for patients over 18 years of age with moderate to severe HE or PPP treated with oral alitretinoin between February 2014 and December 2017. This study was approved by the Institutional Review Board of SMG-SNU Boramae Medical Center (IRB no. 20-2017-31).
HE patients who were refractory to conventional treatments including topical treatments (corticosteroids and/or calcineurin inhibitors), skin care, and avoidance of irritants and allergens if identified were prescribed alitretinoin. Patients with widespread eczema on the body were not included. PPP was diagnosed by clinical features or by histology; when the diagnosis was ambiguous whether it was PPP or vesicular HE, decision was made based on the results of previous studies (
Supplementary Table 1)
6141516.
PPP patients who were refractory to topical treatments (corticosteroids, calcineurin inhibitors, and/or vitamin D agents) or oral acitretin, or who failed tapering of systemic immunosuppressants due to relapse were prescribed alitretinoin. Total 65 patients were screened and 10 of them were lost after first prescription. Adverse events (AEs) were assessed in the remaining 55 patients, and efficacy was assessed in 46 patients treated with alitretinoin for at least 1 month (
Fig. 1).
HE was classified by morphology according to HE classification recently proposed by Diepgen et al.
3 HE which had no vesicles or pustules and had hyperkeratosis only was classified as hyperkeratotic HE (HHE), and recurrent HE with vesicular or pustular eruptions which might accompany hyperkeratosis was classified as vesicular HE (VHE) (
Fig. 1)
17. Morphologically PPP was classified as vesicular morphology according to the criteria mentioned above for HE; in addition some patients demonstrated hyperkeratotic features like hyperkeratosis, scaling, and fissuring. We divided PPP into PPP with hyperkeratotic features (PPP H+) and PPP without hyperkeratotic features (PPP H−) (
Fig. 1).
The severity of disease was evaluated at the first visit and every follow-up visit using the physician's global assessment (PGA): clear, almost clear, mild, moderate and severe (
Supplementary Table 2)
9. Response was defined as a PGA rating of ‘clear’ or ‘almost clear.’ Time to response was defined as the time from alitretinoin initiation to the first response. The basal dose of alitretinoin was 30 mg daily and the dose was decreased to 10 mg every other day, 10 mg daily or 30 mg every other day according to the treatment response and AEs. Concomitant treatments including topical corticosteroids or calcineurin inhibitors, or oral antihistamines were allowed. When the response was achieved, alitretinoin treatment was stopped, or was continued if patients wished. Medical records of all responders were reviewed until December 2017 to follow up the status after response achievement. Relapse was defined as a PGA rating of ‘mild,’ ‘moderate’ or ‘severe’ after alitretinoin discontinuation. Time to relapse was defined as the time from alitretinoin discontinuation to the first relapse. AEs were evaluated at every follow-up visit.
The chi-squared test or Fisher's exact test (when at least one cell had <5 count) was used for categorical variables and the Student's t-test or the Mann-Whitney U test for continuous variables. p-values less than 0.05 were considered statistically significant. Statistical tests were performed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA).
RESULTS
The characteristics of the 55 patients are summarized in
Table 1. More than half of patients showed severe disease and 80% of patients were refractory to previous treatments.
Among 46 patients who were treated with alitretinoin for at least 1 month, 29 patients (61.1% in HE and 40.0% in PPP) showed response to alitretinoin in the median 14 weeks after treatment (
Table 2). Within HE group, HHE group showed higher response rate than VHE group (
p=0.026) (
Fig. 2A). Similarly, within PPP group, PPP H+ group showed higher response than PPP H− group (
p=0.033) (
Fig. 2B). PPP group showed lower response than HHE group (
p=0.026), and similar response with VHE group (
p=0.675) (
Fig. 2A). PPP H+ group showed similar response rate with HHE group (
p=0.554), and PPP H− group showed similar response rate with VHE group (
p=0.278). When total patients were divided into patients with response and those without response, responders had more hyperkeratotic morphology than non-responders (
p=0.005) (
Table 2). However, the following patient characteristics were not significantly different between the two groups: age, sex, body weight, disease duration, initial PGA rating, and diagnosis (
Table 2). Initially 30 mg of oral alitretinoin was administered daily, and dose was reduced in subsequent visits in seven patients due to AE, cost or low compliance (
Table 1). Among the seven, three showed no response to alitretinoin both before and after dose reduction to 10 mg daily or 30 mg every other day. Other four showed good efficacy of alitretinoin after dose reduction to 10 mg daily or 30 mg every other day and reached a PGA rating ‘clear.’ In one, relapsed occurred 2 months after further dose reduction to 10 mg every other day; 10 mg daily dose was as good as 30 mg daily dose, whereas 10 mg every other day dose was not effective.
After achieving response, among 29 responders 75.9% (22/29) discontinued alitretinoin and were observed, and half of those (11/22) were followed up again later (
Table 3). Relapse rate was 63.6% (7/11) and median time to relapse was 150 days (range, 76~730 days).
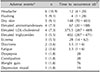
Total 55 patients were evaluated for any AEs during alitretinoin treatment (
Table 4). The median of follow-up period was 77 days (range, 1~609 days) and the median of total alitretinoin dose was 2,280 mg (range, 30~18,270 mg) (
Table 1). In total, 47.3% of patients (26/55) experienced one or more AEs. Headache (10.9%) was the most common, followed by flushing (9.1%), dry skin (9.1%) and laboratory abnormalities including elevated serum aminotransferases (7.3%), elevated serum low density lipoprotein (LDL)-cholesterol (7.3%), and elevated serum triglycerides (5.5%). Compared with other AEs, dry skin and elevated LDL-cholesterol and triglycerides (dyslipidemia) occurred after long-term alitretinoin intake, approximately 5 months or longer. Of 26 patients with AEs, 9 discontinued the treatment, 11 resolved spontaneously or were controlled with symptomatic treatment, 4 underwent dose reduction, and 2 were lost. Headache and flushing were the most frequent AEs leading to discontinuation. Of 5 with dry skin, although all cases were mild and controllable with emollients, 2 discontinued the treatment because they had already achieved therapeutic response. Serum alanine/aspartate aminotransferase was mildly elevated to between 40 and 70 IU/L (normal range, 0~39 IU/L). Also, all cases with dyslipidemia were mild: elevated LDL-cholesterol with early 140s mg/dl (normal range, 0~129 mg/dl), and elevated triglycerides between 200 to 350 mg/dl (normal range, 0~199 mg/dl). AEs disappeared after withdrawal, dose reduction or symptomatic treatment, or they resolved spontaneously. No serious or permanent AE was noted.
DISCUSSION
Alitretinoin (9-cis-retinoic acid) is an endogenous retinoid which is structurally similar to vitamin A. Unlike other retinoids, which bind selectively to either retinoic acid receptors (RAR) or retinoid X receptors (RXR), alitretinoin is a pan-agonist retinoid, capable of binding to all six retinoid receptors (RAR-α, -β, -γ, and RXR-α, -β, -γ)
1819.
Alitretinoin is proven to be efficacious in refractory HE by previous clinical studies
891011. Although the precise mechanism of action of alitretinoin in HE is yet unknown, it is likely due to its anti-inflammatory effects and immunomodulatory properties in various cell types including keratinocytes, fibroblasts, mast cells, dendritic cells and T cells
13. In contrast, retinoids that interact with RAR or RXR alone, such as isotretinoin, acitretin and baxarotene, have relatively limited efficacy in HE
2021. It seems that alitretinoin may affect HE via synergistic activation of multiple retinoid receptors
22.
According to previous controlled clinical trials, 30 mg daily oral alitretinoin for 24 weeks in refractory HE patients achieved response rates of 47.7%~56.7%
89. In a study of Korean patients, similar response rate (44.4%) was achieved by the equal dose for shorter period, 12 weeks
11. In this study, 61.1% of HE patients showed response to alitretinoin. This better response rate than those of previous studies could be attributed to the lower body weights (average, 64.5 kg) of Koreans included in the present study than those of Caucasians in the previous studies (average, 79.2~81.8 kg). This hypothesis needs to be verified in further study because body weight data was available only in approximately half of subjects. In addition, the use of concomitant treatments and a lower percentage of severe patients and patients who were refractory to conventional treatments may have contributed to the higher response rate
89. Alitretinoin was more effective in HHE than in VHE and this result is consistent with prior studies
89.
In PPP, the efficacy of alitretinoin is still controversial
1213. In the most recent clinical trial, Reich et al.
12 showed that alitretinoin had no effect in severe PPP compared to placebo. In the current study, alitretinoin was effective in 40% of patients with PPP. Additionally, as in HE, alitretinoin was more effective when PPP showed additional hyperkeratotic features. This result is reasonable, considering the mechanism by which alitretinoin modulates differentiation and proliferation of keratinocytes.
When responder and non-responder groups were compared within total patients, neither diagnosis nor initial disease severity was related to the response rate. Morphology of lesions was the only factor which was different between the two groups. Response rate to alitretinoin was higher in HE than in PPP; however, when HHE and PPP H+, and VHE and PPP H− were each compared, response rate was not significantly different between the groups, respectively. Within HE, the proportion of HHE was 2 to 4 times higher than that of VHE in our study and other previous studies investigating efficacy of alitretinoin
8910. On the other hand, morphology of PPP basically fits into the vesicular category, but some chronic and recalcitrant cases may demonstrate additional hyperkeratotic features including hyperkeratosis, scaling and fissuring
5. Even so, their proportion in PPP is likely to be smaller than the proportion of HHE in HE. Taken together, our results suggest that the high efficacy of alitretinoin in HE and uncertain efficacy in PPP in previous clinical trials were not due to the difference of disease entity, but due to the difference of proportion of hyperkeratotic features between HE and PPP. The response to alitretinoin in PPP could have been different depending on the proportion of the PPP accompanied by hyperkeratotic features.
PPP is a still unclear disease entity. Some authors consider it a separate entity, whereas others consider it an entity in the spectrum of psoriasis
5. In practice, PPP is difficult to distinguish from HE, especially VHE, even for dermatologists. PPP and VHE share not only similar clinical features but also histological features (
Supplementary Table 1)
6141516. However, the present study suggests that even when the diagnosis is equivocal, the response to alitretinoin can be predicted by morphology regardless of diagnosis.
Ruzicka et al.
9 reported the relapse rate as approximately 40% with 5.5 months of median time to relapse. The median time to relapse in our study was similar to the previous report, but relapse rate was higher. This may be because we did not fix the follow-up period of relapse as the previous study, resulting in a much longer follow-up time. Furthermore, there is a possibility that patients with relapse tended to return to clinic more than those without relapse.
There were AEs, but they were all controllable and transient. AEs occurred in 47.3% of total patients, and this is higher than the 23% reported in the previous studies of Caucasians. Analogous to the higher response rate than in previous studies, higher AE rate may be explained by the generally lower body weights of Koreans than Caucasians.
We observed that the efficacy of alitretinoin was maintained after dose reduction in four of seven patients. With regards to the efficacy and safety, the ideal regimen to administer alitretinoin in the Asian patients has not been determined yet, and a larger scale study in the future may provide additional answers to whether starting with 30 mg and dosing down is better or starting with 10 mg and dosing up gradually is better. According to the median occurrence time, AEs were divided into two groups; dry skin and dyslipidemia (elevated LDL-cholesterol and triglycerides) developed after a long-term administration for more than 5 months, whereas the other AEs occurred within 2 months. Headache and flushing were most common AEs in the first 2 months and this result is similar with prior studies
910.
This study has some limitations: including its retrospective nature, a relatively small number of patients with PPP compared to HE, and having no control group. Particularly, owing to small number of PPP patients, the present results should be accepted with considering the possibility of selection bias and need to be reviewed in a further study with larger subjects. However, our study demonstrated and compared the efficacy of alitretinoin in the largest number of patients in Korean (east Asian) for the first time, and it investigated the safety of alitretinoin for the longest period thus far. Furthermore, its novel conclusion that morphology is the most important factor to predict the response to alitretinoin will be useful in real life practice setting where differentiation of PPP from HE is not always clear-cut.
In conclusion, the efficacy of alitretinoin in HE and PPP can be predicted based on the morphology regardless of diagnosis. Lesions with hyperkeratotic features are expected to respond better to alitretinoin than those with other features. Finally, AEs were all controllable and transient in patients who remained on alitretinoin regimen.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download