Abstract
Purpose
To analyze the risk factors and the rate of neurological complication occurring after micro-surgical enucleation of schwannoma, and the relationship between single fascicle resection and neurological deficiency.
Methods
From January 2010 through September 2018, a total of 65 patients underwent micro-surgical enucleation for schwannoma in the forearm and hand. The factors affecting new neurological deficiency after surgery were analyzed, and the differences in neurological incidence were compared between those that preserved the fascicle and those that were unavoidable to resect the fascicle at surgery.
Results
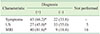
Immediately neurological complications were reported in 16 patients (24.6%) after the surgery, with 4 patients (6.2%) remaining in the final outcome. Neurological complication (50.0%) was higher in case of resection of fascicle at surgery (hazard ratio, HR=18.791, p<0.05). The preoperative misdiagnosis also increased the incidence of neurological complications (HR=10.693, p<0.05).
Conclusion
Accurate diagnosis before surgery and preservation of the nerve fascicle at surgery are important to reduce postoperative neurological complications in the treatment of schwannoma. For accurate diagnosis, detailed history taking, physical examination and magnetic resonance imaging should be actively done, and during surgery, efforts should be made to preserve the nerve fascicle as much as possible by using microscopic surgical techniques.
Figures and Tables
 | Fig. 1(A) Ultrasonographic imaging of a 78-year-old male patients shows hypoechogenic mass with small vascularity. (B) On magnetic resonance imaging, sagittal T1-weighted image revealed a homogenously enhancing tumor expanding the superficial branch of radial nerve. (C) Magnetic resonance neurography image demonstrated high signal of the tumor and longitudinal course of the nerve. (D) Intraoperative photograph showing the tumor prior to capsulotomy and enucleation. (E) Under microscope, completely intra-capsular enucleation was done. (F) After enucleation, all nerve fascicle was preserved. |
 | Fig. 2Gross photography of specimens. (A) Completely intracapsular enucleated tumor. (B) Incompletely intra-capsular enucleation with resection of fascicle. |
 | Fig. 3Locations of the schwannomas and the nerves involved (left: forearm, right: hand, red: radial nerve, yellow: median nerve, blue: ulnar nerve). |
References
1. Erlandson RA, Woodruff JM. Peripheral nerve sheath tumors: an electron microscopic study of 43 cases. Cancer. 1982; 49:273–287.


3. Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg. 2005; 102:246–255.


5. Sawada T, Sano M, Ogihara H, Omura T, Miura K, Nagano A. The relationship between pre-operative symptoms, operative findings and postoperative complications in schwannomas. J Hand Surg Br. 2006; 31:629–634.


6. Knight DM, Birch R, Pringle J. Benign solitary schwannomas: a review of 234 cases. J Bone Joint Surg Br. 2007; 89:382–387.

7. Park MJ, Seo KN, Kang HJ. Neurological deficit after surgical enucleation of schwannomas of the upper limb. J Bone Joint Surg Br. 2009; 91:1482–1486.


8. Kim SM, Seo SW, Lee JY, Sung KS. Surgical outcome of schwannomas arising from major peripheral nerves in the lower limb. Int Orthop. 2012; 36:1721–1725.



9. Mizushima H. Neurological deficits before and after surgical resection of schwannomas in the upper extremities. J Reconstr Microsurg. 2016; 32:371–377.


10. Donner TR, Voorhies RM, Kline DG. Neural sheath tumors of major nerves. J Neurosurg. 1994; 81:362–373.


11. De Flaviis L, Nessi R, Del Bo P, Calori G, Balconi G. High-resolution ultrasonography of wrist ganglia. J Clin Ultrasound. 1987; 15:17–22.


12. Kehoe NJ, Reid RP, Semple JC. Solitary benign peripheral-nerve tumours. Review of 32 years' experience. J Bone Joint Surg Br. 1995; 77:497–500.


13. Holdsworth BJ. Nerve tumours in the upper limb. A clinical review. J Hand Surg Br. 1985; 10:236–238.


14. Reynolds DL Jr, Jacobson JA, Inampudi P, Jamadar DA, Ebrahim FS, Hayes CW. Sonographic characteristics of peripheral nerve sheath tumors. AJR Am J Roentgenol. 2004; 182:741–744.


15. Chinn DH, Filly RA, Callen PW. Unusual ultrasonographic appearance of a solid schwannoma. J Clin Ultrasound. 1982; 10:243–245.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download