INTRODUCTION
Adequate local anesthesia is required to prevent and manage pain, ensure patient comfort, and allow clinicians to thoroughly perform procedures. Anesthesia for periodontal flap surgery in a maxillary quadrant requires multiple injections including the nasopalatine (NP) and greater palatine (GP) nerve blocks for palatal aspect, apart from several local infiltrations for the facial aspect [
1]. Each of these injections is painful, and anesthetizing the facial aspect unnecessarily affects the upper lip, part of the nose, lower eyelid and muscles of facial expression [
2]. Anterior middle superior alveolar (AMSA) injection was described by Friedman and Hochman in 1997 [
2]. It is so named because it can anesthetize both the anterior and middle superior alveolar nerves with a single palatal injection. The site of AMSA injection is on the palatal mucosa between first and second premolars—half way between the mid-palatine raphe and the free gingival margin [
12345]. This site corresponds with the confluence of the anterior superior alveolar (ASA) nerve, the middle superior alveolar (MSA) nerve, and the associated subneural dental plexus [
4].
Although AMSA injection can be administered using a conventional syringe, computer-controlled local anesthetic delivery (CCLAD) systems confer better outcomes, including higher patient acceptance [
5]. They enable virtually painless injections delivered at a precisely controlled high pressure but with a constant slow rate of volume flow, irrespective of tissue resistance [
1]. Furthermore, CCLAD minimizes anxiety in both patient and operator, and it can be two to three times less painful than manual injection [
6].
The extent and efficacy of AMSA injection have been explored in several studies, with conflicting results. Fukayama et al. reported that CCLAD-administered AMSA injection is highly effective for pulpal anesthesia of the lateral incisors, canines, and premolars [
7]. Friedman and Hochman observed that bilateral AMSA injections anesthetize 10 teeth—from the second premolar on one side to that on the other side [
8]. Some other clinicians have reported that AMSA injection can anesthetize the entire ipsilateral palatal mucosa as well as the maxillary teeth extending from the central incisor to the mesiobuccal root of the first molar and the associated facial gingiva [
910]. However, most of the previous studies evaluated the effect in terms of pulpal anesthesia.
Holtzclaw and Toscano reported five cases of AMSA injection in periodontal surgery [
11]. They reported several advantages, such as improved palatal hemostasis and avoidance of undesirable collateral anesthesia, but they could not provide any conclusive evidence regarding the extent of anesthesia. Acharya et al. were the first to report that AMSA injection was effective till the last standing molar and that it sometimes crossed the midline [
3]. They concluded that it may be sufficient for periodontal surgery in the maxilla. However, they used a 27-gauge needle with a conventional syringe, so they could not administer the injection with precise pressure and speed. Rapid injection tends to displace tissues, whereas CCLAD directs the solution through the connective tissue, periosteum, cortical bone, and medullary bone [
1].
Considering these results, researchers must elucidate whether a single AMSA field block injection can eliminate the conventional need for multiple injections during periodontal flap surgery in a maxillary quadrant. In particular, no previous studies have evaluated the effect of this injection on the palatal and buccal hard and soft tissues, separately around each tooth in a maxillary quadrant. Therefore, the present study had the following objectives: (1) to assess the effectiveness of AMSA injection using CCLAD in anesthesia of the buccal hard tissue (BHT), buccal soft tissue (BST), palatal hard tissue (PHT), and palatal soft tissue (PST) around maxillary teeth, and (2) to assess whether the effectiveness of AMSA injection using CCLAD depends on the position of teeth within the arch.
Go to :

MATERIALS AND METHODS
1. Study design
This was a quasi-experimental study conducted in accordance with the 1975 Declaration of Helsinki for medical research involving human subjects, as revised in 2013. The study was approved by the institutional ethics committee (Ref. No.: MAIDS/Ethical Committee/6721) in September 2012. The significance level was set at 95%, and the power at 80%; on this basis, the minimum required sample size was estimated as 30. The inclusion criteria were as follows: (1) at least one maxillary quadrant with a minimum of six teeth that had a probing pocket depth (PPD) ≥ 5 mm and (2) bleeding on probing (BoP) on any of the six aspects (mesiobuccal, mid-buccal, distobuccal, mesiopalatal, mid-palatal, or distopalatal). The exclusion criteria were (1) acute periodontal or endodontic conditions; (2) mobility of grade II or higher; (3) angular defects that required regenerative procedures in any maxillary quadrant; (4) history of allergy to local anesthetic solution; (5) current smoking; (6) pregnancy; and (7) any medication that may have altered pain threshold, pain perception, onset of anesthesia, or profundity of anesthesia.
2. Sample selection
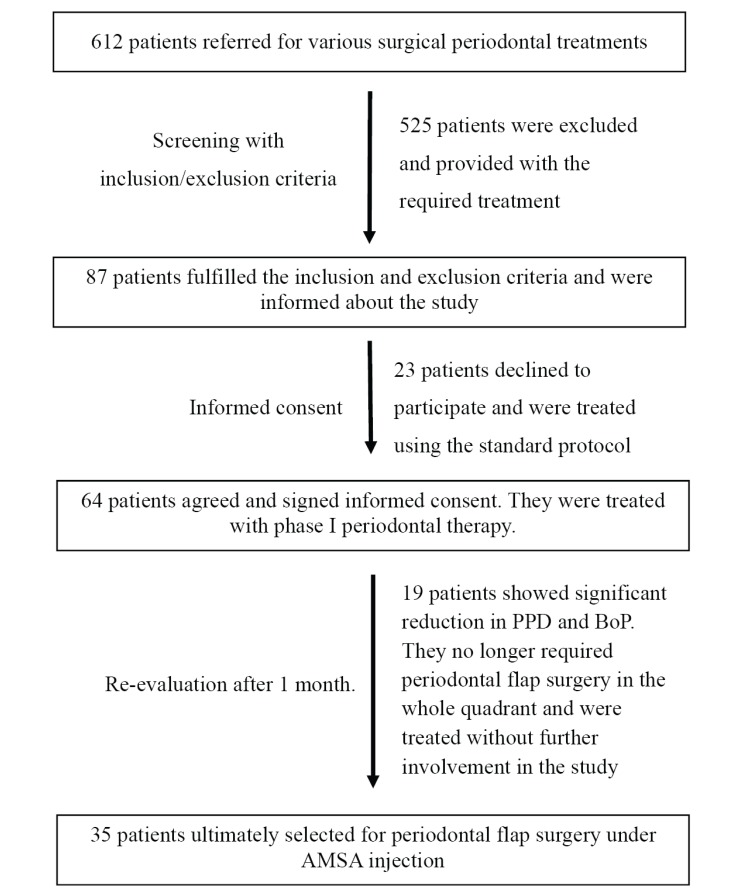
Applying the inclusion and exclusion criteria, we screened 612 patients referred from the outpatient Department of Periodontics to the postgraduate clinic for periodontal surgery (mucogingival surgery, pocket reduction/elimination, implant placement, or pre-prosthetic surgery). Ultimately, 87 patients were selected. After study information was provided, only 64 patients signed informed consent. They were subsequently provided phase I therapy, which included scaling and root planing (SRP), restoration of caries, correction of occlusal prematurities, and instruction on oral hygiene. All of them were recalled 1 month later to assess their response to phase I therapy. However, only 54 patients complied, out of which 19 were excluded as their PPD was reduced to 3–4 mm in most of the teeth, with significant reduction in BoP. They no longer required periodontal flap surgery in the whole quadrant and were treated without further involvement in the study. Thus, 35 patients were ultimately selected for periodontal flap surgery under AMSA injection.
Fig. 1 outlines the sample selection.
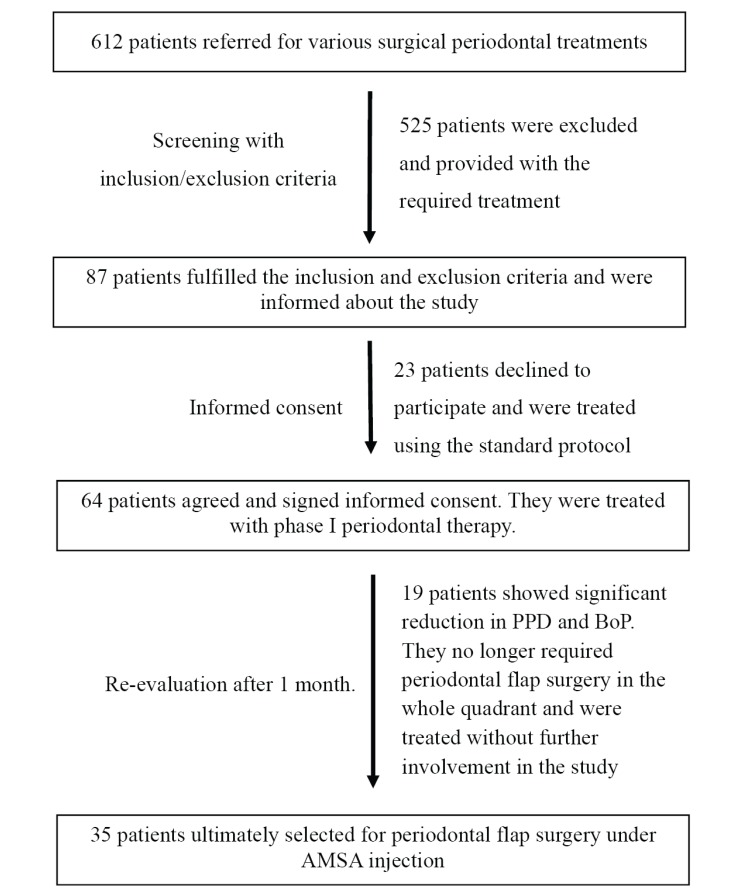 | Fig. 1An outline of the sample selection process
|
3. Local anesthesia and surgical procedure
All patients were instructed not to take any analgesics for 24 hours before the planned surgery. The CCLAD system used (Wand®; Milestone Scientific Inc., Livingston, NJ, USA) had a disposable, lightweight, pen-like needle linked by microtubing to a local anesthetic cartridge. It is operated using a foot control that automates local anesthetic delivery. After presurgical preparation, AMSA injection was delivered using a 30-gauge, ultra-short needle by a single operator (S.T.) who had previously administered AMSA injection using CCLAD to more than 100 patients in various dental procedures. This operator was not involved in any further steps of the investigation, including assessment of the anesthesia or flap surgery. The injection site was the point that bisected the maxillary first and second premolars—half way between the free gingival margin and the mid-palatine raphe (
Fig. 2). Patients were placed in a supine position, with slight hyperextension of the head and neck. The needle was then oriented at 45°, with the bevel facing the palatal soft tissue, and inserted by axial rotation (45° clockwise and 45° counterclockwise). An entire 1.8 mL cartridge of 2% lignocaine hydrochloride (Lignospan special; Septodont, Saint-Maur-des-Fossés, France; with 1:80,000 adrenaline) was administered in 3–4 minutes. During this period, the operator had a direct view of the injection site to check for any leakage. To allow the local anesthetic solution to dissipate within the tissue and minimize dripping during needle withdrawal, the operator waited for 10 seconds after completing the injection before retracting the needle. Since a small portion of local anesthetic solution is lost during the purge cycle of CCLAD and some volume remains unused in the tubing, approximately 1.4 mL is injected from the 1.8 mL cartridge [
5].
 | Fig. 2Delivery of AMSA injection using the CCLAD system
|
4. Evaluation of the outcome parameters
After 10 minutes, the objective parameters were evaluated by two experienced examiners (A.K.L. and F.F.) to check the effectiveness and extent of local anesthesia. They showed high inter-examiner reliability (Cohen's kappa = 0.9). Objective evaluation (Anaesthetized/Non-Anaesthetized) was done for the BHT and the BST on the mesio-buccal, mid-buccal and disto-buccal aspects of each tooth of the quadrant. Similarly, the mesiopalatal, mid-palatal, and distopalatal aspects of the PHT and PST were evaluated. The effectiveness of pulpal anesthesia was not recorded, as it is less relevant in periodontal flap surgery. The parameters were recorded as anesthetized if there was a complete absence of pain and non-anesthetized if even the minimal pain was present during the entire process of surgery. Objective soft tissue parameters were recorded on the basis of (1) gentle probing through the gingival sulcus using a periodontal probe (UNC-15; Hu-Friedy, Chicago, IL, USA) and (2) pressure testing using the blunt end of a mirror handle. To test the effects on the hard tissues, parameters were recorded on the basis of pain during (1) trans-gingival probing/sounding of bone through the gingival sulcus, and (2) flap reflection and/or debridement. Tissue was considered as anesthetized only if the above procedures did not elicit any verbal or visual response suggestive of pain. The extent of blanching was recorded separately as a subjective parameter.
When anesthesia was inadequate to start flap surgery, appropriate local infiltration was administered using a 27-gauge needle by the conventional technique. All 35 surgeries were performed by the same team of periodontists (K.A., A.A., and N.Y.) and were completed within 1 hour without any need for additional injection during surgery.
5. Statistical analysis
Outcome parameters (anesthetized or non-anesthetized) were recorded separately on the BHT, BST, PHT, and PST of each tooth in the quadrant. The percentage of anesthetized and non-anesthetized areas was calculated. The Chi-square test was used to calculate the correlation between patient sex and outcome parameters. Anesthetic success in the anterior (central incisor to premolars) and posterior (molars) regions was also compared using the Chi-square test. Significance was defined as a P-value < 0.05.
Go to :

DISCUSSION
The present study evaluated the extent and effectiveness of anesthesia achieved by a single AMSA injection prior to periodontal flap surgery. Therefore, it is important to briefly discuss the nerve supply of the maxillary hard and soft tissues.
All maxillary teeth, associated periodontium, PHT, and PST are supplied by different branches of the maxillary nerve. While the palatal hard and soft tissues are innervated by the GP and NP nerves, the rest is supplied by three major branches: the posterior superior alveolar (PSA), MSA, and ASA nerves. The individual roots of all teeth and their associated periodontium are innervated by the network of terminal branches of larger nerves in the region, known as the subneural dental plexus. This network is the target site for AMSA injection [
4].
When adequate local anesthetic solution (0.6–0.9 mL) [
1] is deposited onto the palatal aspect of the apices of premolars, it diffuses through the nutrient canals and porous cortical bone to envelop the subneural dental plexus, anesthetizing the areas supplied by the ASA, MSA and PSA nerves [
5910]. Anesthetic solution also diffuses beneath the palatal mucoperiosteum to reach the branches of the GP and NP nerves [
12]. In particular, CCLAD facilitates this diffusion more easily because it ensures a uniform, slow injection speed, providing adequate time for the local anesthetic solution to reach the areas that must be anesthetized during flap surgery in a maxillary quadrant. Thus, AMSA injection can be considered a kind of field block.
In the present study, the areas successfully anesthetized by AMSA injection required no supplementary infiltration during surgery, which lasted up to 60 minutes, confirming previous reports in which the duration of anesthesia was 45-120 minutes after AMSA injection [
13].
Although several studies have suggested that blanching of the palate is ipsilateral [
510], we observed that blanching extended beyond the mid-palatine raphe in some cases, perhaps because we used a higher volume of local anesthetic solution (1.8 mL). Acharya et al., who used 2 mL of same local anesthetic solution, also reported that the effects of AMSA injection sometimes crossed the midline [
3].
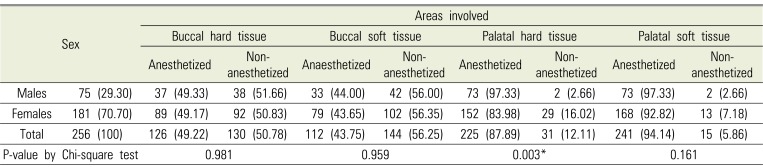
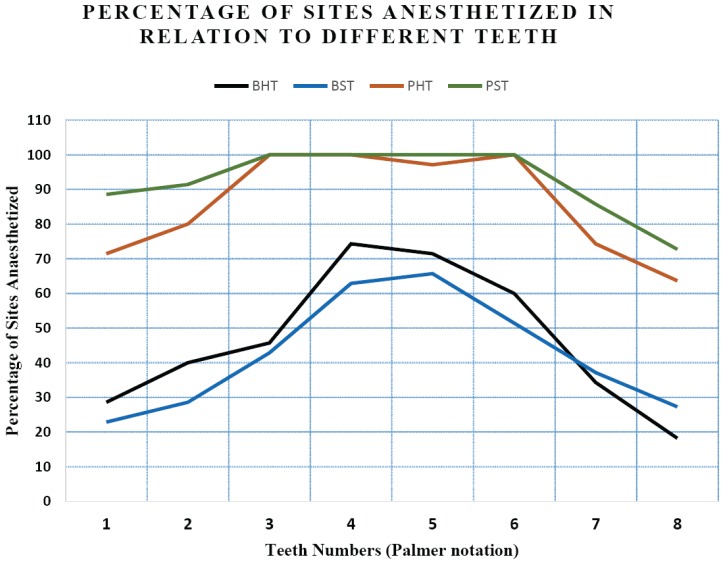
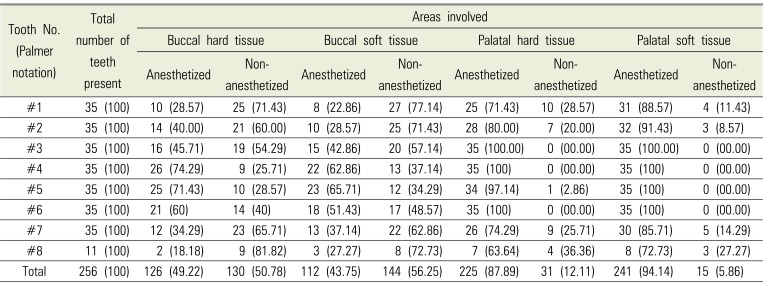
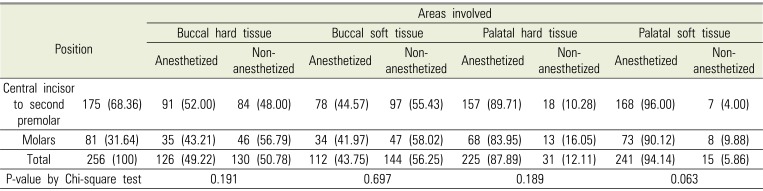
Since there is a lack of adequate data regarding the effectiveness of AMSA injection separately on hard and soft tissues, which are important in periodontal surgical procedures, we explored this issue individually in all maxillary teeth. AMSA injection appears to be highly predictable in the PHT and PST, wherein 87.89% and 94.14% of sites in the whole maxillary quadrant were anesthetized, respectively. Regarding the buccal aspect, the data obtained in the present study were disappointing. The overall frequency of successful anesthesia in the BHT and BST was just 49.22% and 43.75%, respectively.
Most previous studies have claimed that AMSA injection is effective from the central incisor to the second premolar [
12458]. However, Acharya et al. reported that AMSA injection using a conventional syringe is effective to the last molar in a maxillary quadrant, concluding that it may be a valuable technique for periodontal surgery in the maxilla [
3]. We found that anesthetic success rates were higher in the anterior region (central incisor to second premolar) than in the posterior region (molars). However, the difference was insignificant in all four tissue types (
Table 3).
We confirmed the findings of Acharya et al. [
3] for the palatal aspect, but not for the buccal aspect, as injection was effective in 83.95% of PHT and 90.12% of PST sites around the molars. Shirmohammadi et al. also used a conventional syringe for the injections and concluded that AMSA technique could be recommended for the anesthesia of palatal tissues in periodontal surgery [
13].
For anesthesia of the buccal tissues, which often corresponds with pulpal anesthesia, we found that AMSA injection is least effective around the central incisors (28.57%) and third molars (18.18%). This finding corroborates the previous results of Fukayama et al [
7], who observed that lateral incisors, canines, and premolars were more frequently anesthetized than central incisors and first molars. Velasco and Soto observed that, as a first-line treatment, AMSA injection is unpredictable, being effective in only 16.7%, 23.3%, 60%, 40%, and 66% of cases for the central incisor, lateral incisor, canine, first premolar, and second premolar, respectively [
14]. Corbett et al. assessed the effectiveness of AMSA injection using electric pulp testing, concluding that it was ineffective for the central incisors [
15].
Our findings contradict those of Tolentino et al. who compared the effect of AMSA injection on buccal periodontium with that of supraperiosteal infiltration using conventional syringes [
16]. They performed SRP only on the buccal aspect of the central incisors to premolars and recorded the patients' pain perception. They concluded that both the techniques were effective in controlling pain in the buccal tissues of the maxilla during subgingival SRP. However, they did not evaluate the effect of AMSA injection beyond the premolars.
In the present study, the facial and palatal aspects differed for several reasons—most importantly because the normal anatomical nerve pathways vary among individuals [
17]. While the sensory fibers from the pulp of maxillary teeth are primarily carried through the ASA, MSA, and PSA nerves, which also supply the buccal hard and soft tissues, accessory pulpal innervation occurs via branches of the GP and NP nerves [
17]. This may explain why the success rate of AMSA injection was higher on the buccal aspect in some previous studies [
1316].
On the palatal aspect, the sufficient volume and uniform slow speed of injection facilitate the diffusion of local anesthetic through the whole ipsilateral palate, as evidenced clinically by blanching of this area [
5]. This diffusion helps to anesthetize the branches of GP and NP nerves [
12], resulting in profound anesthesia of the PHT and PST. However, on the buccal aspect, many anatomical factors may lead to a low success rate of AMSA injection in the BHT and BST. One recent study claimed that the palatal aspect has significantly more and wider canals penetrating the whole cortex than the buccal aspect in the same region [
18]. These canals facilitate the diffusion of local anesthetic solution to the subneural dental plexus in the trabecular bone [
18]. In particular, the presence of the MSA nerve varies among individuals, as it may be duplicated [
12] or absent in 28% [
19] to 54% [
20] of individuals. The site of origin of the MSA nerve also varies, from the posterior part of the infraorbital canal to the anterior part near the infraorbital foramen [
4]. The course of the ASA nerve, which forms part of the subneural dental plexus, also varies. Usually, it arises from the midpoint of the infraorbital canal, but sometimes it originates near the infraorbital foramen [
4]. The porosity and thickness of cortical bone plates also vary among persons and even among different areas of a bone [
4]. This may limit the diffusion of local anesthetic to the subneural dental plexus [
1].
Age, sex, anxiety, fear, and even cultural factors affect pain perception by patients [
2122]. Tolentino et al. observed that, although AMSA injection was generally effective on the buccal periodontium, it was less effective in females [
16]. In the present study, we compared the effect of AMSA injection between males and females and found no significant difference, except in the PHT, which was more predictably anesthetized in males (97.33%) than in females (83.98%; P = 0.003), perhaps because of sex-based anatomical differences. Cetkovic et al. investigated morphological parameters in the palatal cortex and found that the maximum number of nutrient canals is present in the palatal process in females and in the border zone between the palatal and alveolar processes in males [
18]. These findings could be applied clinically to optimize needle positioning according to sex and thus achieve more predictable anesthesia.
In any case, single AMSA injection using CCLAD significantly reduces the pain and discomfort associated with NP and GP nerve blocks, which can be the most traumatic intraoral injections [
423]. It also offers better hemostasis in palatal tissue than these nerve blocks [
14]. In this regard, Holtzclaw and Toscano observed adequate hemostasis in the surgical field, concluding that although AMSA injection cannot replace traditional dental anesthetic methods, it may prove useful in certain situations. They also mentioned several potential disadvantages of AMSA injection, including its long administration time, which could be frustrating for some patients [
11].
Although this study had several limitations, AMSA injection using CCLAD appeared to be highly predictable for palatal anesthesia until the last molar, allowing periodontal flap surgery. Its effect on the buccal tissues was less predictable, particularly around the central incisors and third molars. We suggest that the technique could be used as a first-line local anesthesia in maxillary periodontal flap surgery and supplemented by supraperiosteal infiltration when required. It is likely to reduce the necessary number of injections, as well as the cumulative amount of local anesthetic and vasoconstrictor used, resulting in a more pleasant experience for both patient and operator.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download