INTRODUCTION
Preventable trauma death rate (PTDR) is defined as the rate of deaths of individuals who are considered to have survived if they would have been properly transported to the appropriate hospital within the appropriate time and received the appropriate treatment.
1 PTDR is widely used as a key indicator of trauma system performance. In Korea, PTDR has been estimated periodically since the late 1990s, declining from 50.4% in 1997–1998 to 35.2% in 2009–2010; however, these values remain high.
234 Since 2012, the Ministry of Health and Welfare in Korea has commenced a project to install regional trauma centers (RTCs) to reduce the PTDR to less than 20% by 2020.
56 The project aims to establish nationwide regionalized trauma system so that patients can be transferred to the RTCs within one hour whenever and wherever serious trauma patients are located in Korea. As of December 2015, 15 hospitals were designated as candidates for RTCs, and 8 RTCs are open officially in Korea. However, the national PTDR has not yet been fully evaluated since the Korean government started running the master plan to establish national trauma system based on the implementation of RTCs.
This study aimed to evaluate not only the current overall PTDR in Korea but also the differences in PRDR between gender, ages, final institutions destined for the death, and transfer status. Furthermore, we explored factors associated with PTDs.
METHODS
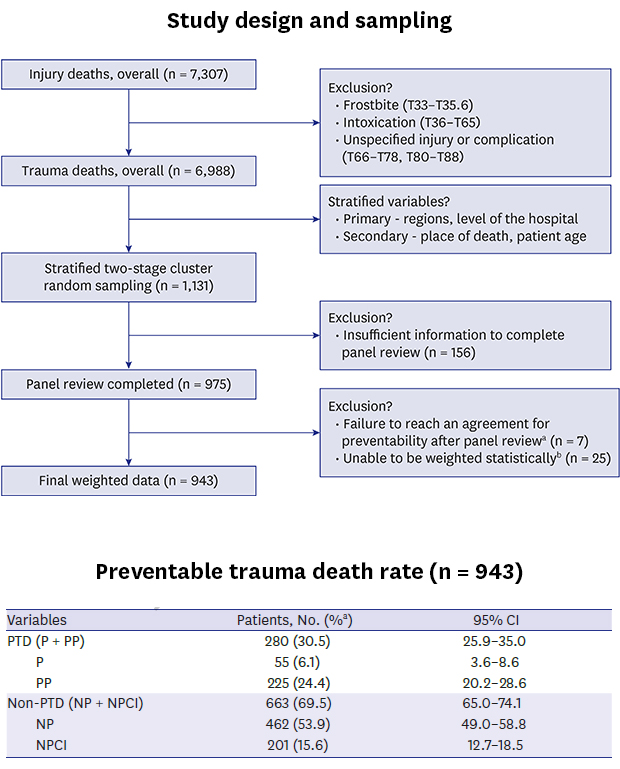
Study design and data collection
The data was extracted from the National Emergency Department Information System (NEDIS) of Korea. The NEDIS is a nationwide database that contains clinical and administrative data of patients visiting emergency department. The target population for sampling of the main survey was selected from 7,307 deaths with a diagnosis code of S, T based on the Korean Standard Classification of Diseases (KCD) 6th edition of patients who visited the emergency medical institution from January 1, 2015 to December 31, 2015. Among them, 6,988 deaths were selected as the final target population, excluding those with associated frostbite, poisoning, or other and unspecified effects of external causes and complications regarding surgical and medical care. Among the final target population, 1,142 cases were dead on arrival (DOA), 599 cases died in the emergency room, 3,257 cases died after hospitalization, and 1,990 cases died after transfer from another hospital. Emergency medical institutions with more than 5 deaths were selected as sampling targets. As a result, approximately 96% of the target population was included in the survey population. For sampling, the stratified two-stage cluster sampling method was applied, and stratification was designed as a double layer. The region (Seoul, Gyeonggi/Incheon, Chungbuk, Chungnam/Gangwon/Daejeon, Jeonbuk, Jeonnam/Jeju, Gyeongbuk, Gyeongnam), type of emergency medical institution (regional emergency medical center, local emergency medical center, local emergency medical institution), and number of deaths (less than 30 deaths, more than 30 deaths) were used as the first stratification variable for sampling hospitals. Next, we used the death place (DOA, death in emergency room, death after hospitalization) and the age of patient (age 14 years or less, age 15–54, age 55 years or more) as the second stratification variable for sampling sample deaths in hospitals. However, children aged 14 years or less were all included in the sample because of the small sample size. In addition, to identify the exact cause of PTD, all deaths of patients who visited the regional emergency medical center, which mainly deals with the treatment of severe emergency patients, were included in the sample subjects. Ultimately, the target sample size was designed to be 1,131 deaths in 60 emergency medical institutions. The number of regional sample sizes was 11 hospitals in Seoul (161 deaths, 14.2%), 12 hospitals in Gyeonggi/Incheon (240 deaths, 21.2%), 12 hospitals in Gangwon/Daejeon/Chungbuk, Chungnam (240 deaths, 21.2%), 11 hospitals in Jeonbuk, Jeonnam/Jeju (210 deaths, 18.6%), and 14 hospitals in Gyeongbuk, Gyeongnam (280 deaths, 24.8%) (
Table 1).
Table 1
Distribution of the sample institutions and the trauma deaths according to the regions and types of institutions

|
Regions |
Total |
Regional emergency medical center |
Local emergency medical center |
Local emergency medical institution |
|
< 30 deaths |
≥ 30 deaths |
< 30 deaths |
≥ 30 deaths |
|
Total |
60 (1,131)a
|
20 (571) |
12 (120) |
14 (280) |
12 (120) |
2 (40) |
|
Seoul |
11 (161) |
1 (11) |
3 (30) |
4 (80) |
2 (20) |
1 (20) |
|
Gyeonggi/Incheon |
12 (240) |
5 (150) |
3 (30) |
2 (40) |
2 (20) |
0 (0) |
|
Gangwon/Daejeon/Chungbuk, Chungnam |
12 (240) |
5 (140) |
2 (20) |
2 (40) |
2 (20) |
1 (20) |
|
Jeonbuk, Jeonnam/Jeju |
11 (210) |
4 (120) |
2 (20) |
2 (40) |
3 (30) |
0 (0) |
|
Gyeongbuk, Gyeongnam |
14 (280) |
5 (150) |
2 (20) |
4 (80) |
3 (30) |
0 (0) |
Constituting the panel and multidisciplinary review
The panels for the case review mainly comprised trauma specialists working at the RTCs. A total of 10 teams were formed, and each team consisted of two general surgeons, one thoracic surgeon, one neurosurgeon, and one emergency physician. Apart from this, the Trauma Death Review Committee (TDRC), which was also comprised five trauma specialties, was responsible for developing the guidelines for the whole review process and for training the panels. A workshop was held for the purpose of introducing the guidelines and training regarding the panel review process. Furthermore, when preventability was not decided by the primary panel review, the committee reviewed the cases again and confirmed final decisions for inclusion and preventability. To evaluate the reliability of panel review, three panel teams were selected. They repeated review for the 8% of overall cases that had already been reviewed by other panel teams. The cases were selected from the three hospitals, which were selected one by one from each region throughout the country after the country was divided into 3 regions based on the location mapping of 15 RTCs.
Criteria for preventability of trauma deaths
The criteria for preventability of trauma deaths were based on World Health Organization guidelines for trauma quality improvement programs.
7 The main factors underlying the decision regarding preventability of trauma deaths comprised severity of injuries and appropriateness of trauma care. Definitions were as follows.
1) “PTDs” were deaths that could have been prevented if appropriate steps had been taken, with accompanying injuries and sequelae considered survivable. These cases had frank deviations from standard of care that, directly or indirectly, caused the patient's death.
2) “Potentially PTDs” were deaths that potentially could have been prevented if appropriate steps had been taken, with accompanying injuries and sequelae considered severe but survivable. These cases had some deviations from standard of care that, directly or indirectly, caused the patient's death.
3) “Non-PTDs” were deaths that were unavoidable, as accompanying injuries and sequelae were considered non-survivable even with optimal management. Evaluation and management were appropriate according to accepted standards. If the patient had co-morbid factors that were major contributors to death, such cases were considered non-PTDs.
Statistical analysis
The weight of sample for deaths is

, where

is the design weight of sample hospitals. The non
adjh is the adjustment value for non-response of sample hospitals, and

corresponds to death weight in the sample hospitals. In the benchmarking adjustment using the population information, the death distribution of the population in respect of region × type of emergency medical institutions, type of emergency medical institutions × characterization of deaths, region × characterization of deaths was used. The characteristic layer of death distinguished between age and location of death, divided into 7 layers. We applied the raking ratio method to the population information to calculate the final weights by correcting the primary weights of the sample deaths.
We used a modified Clopper-Pearson method to analyze the PTDR and 95% confidence intervals (CI) for each factor. The PTDRs and their 95% CIs were calculated according to the components of risk factors to cause PTDR differences and the PTDR difference among groups by factors was conducted with Pearson's χ2 test, and the difference between the RTC and non-RTC was calculated using the Cochran-Mantel-Haenszel test. The agreement between the first and the second reviews and between review panel teams were evaluated using Cohen's Kappa index.
To examine the association between the likelihood of preventable death and its relating factors, we constructed two multivariate logistic regression models with weights such as (Model 1: F(Y) = α + β1[Age] + β2[Hospital type] + β3[Regions] + β4[Transfer status]; Model 2: F(Y) = α + β1[Age] + β2[Hospital type] + β3[Regions] + β4[Time from accident to death]). We did not construct one model considering both variables of [Transfer] and [Time from accident to death] because all subjects experienced in twice or more hospital transfer (n = 14) were included in only the category of [time duration from accident to death > 24 hours]. The likelihood of PTD according to relating factors was expressed with odds ratios (ORs) and their 95% CIs relative to reference value.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Seoul National University (IRB No. E-1607-001-771). Informed consent was waived by the board due to the observational nature of the study.
DISCUSSION
This study shows that the overall PTDR in Korea has been decreasing since its initial measurement in the late 1990s, but the rate is still high (30.5%; 95% CI, 25.9%–35.0%) compared with that in countries with an established trauma care system such as the US and Canada. In particular, the overall PTDR was substantially lower in RTCs than that in non-RTCs. The PTDR was 21.4% (95% CI, 16.4%–26.4%) when the final destined institution for the patient was an RTC; this was lower than the PTDR of 33.9% (95% CI, 28.0%–39.9%) in non-RTCs. In addition, the PTDR was higher with an increase in the number of times passing other hospitals or the elapsed time from the accident to the death. In case of passing two or more hospitals before arrival of the final destined institution, the PTDR was 58.9% (95% CI, 24.9%–92.9%), which was much higher than 28.4% (95% CI, 22.9%–34.0%) when directly visiting the final destined institution. These results imply that to reduce the PTDR in Korea, trauma patients need to be transferred to the RTC urgently from the time of the accident.
The PTDR in Korea has been slowly declining since its initial measurement in the late 1990s. Using data from emergency medical centers of secondary and tertiary hospitals, the PTDR was 50.4% in Korea from 1997–1998.
2 Kim et al.
3 reported a PTDR of 39.6% in 2003–2004 in a survey conducted in 9 hospitals in Korea. Furthermore, Kim et al.
4 reported a PTDR of 35.2% in the 20 trauma specialization centers across the country in 2009–2010. All of these studies were done by multidisciplinary panel review, and our results showed similar level of agreement when compared inter-rater reliability of preventable death judgements between panel teams with these previous studies in Korea and the United States.
2348 Although a direct comparison is difficult due to differences in the study subjects, judgment of prevention possibilities, and statistical methods, the PTDR in Korea has been consistently higher than that of some other industrialized countries. Recently, Motomura et al.
9 reported a PTDR of 29.0% in Chiba, Japan, Sandal et al.
10 reported a PTDR of 6.7% in Utah, USA in 2005, and Teixeira et al.
11 reported a PTDR of 2.4% in California, USA from 1998 to 2005.
The PTDR in the hospitals running RTCs was 21.4% (95% CI, 16.4%–26.4%), which was significantly lower than that in non-RTCs. Similar results were derived in the multivariate analysis. In Korea, RTCs began to be designated in 2012 and have been opened and operated from 2014. The RTC differs from the former domestic trauma treatment system. The RTC requires the operation of essential equipment and dedicated personnel in the operating room, an intensive care unit, trauma resuscitation room, and angiogram room to perform the treatment immediately after the severe trauma patient is transferred to the hospital. A general surgeon, thoracic surgeon, neurosurgeon, and orthopedic surgeon must be assigned to the trauma team.
5 The operation of the nationwide RTC is estimated to be one of the factors contributing to the reduction of PTDR in Korea.
The results of this study show that the PTDR increases when the time from accident to death is lengthened or the time to final treatment is delayed (data not shown here). When factors associated with inappropriate treatment were divided into pre-hospital and hospital phases, factors such as delayed transfer between hospitals (29.5%) and inappropriate hospital selection (25.1%) accounted for the largest portion following circulatory assistance (30.3%) at the pre-hospital stage. When problems associated with the pre-hospital stage was divided by means of transportation, for 119 paramedics, delayed transfer was the main reason, whereas for hospital ambulances, inappropriate transfer hospital selection was the main reason.
3 Furthermore, when comparing PTDR-related problems in Korea and Australia, Korea had a relatively higher rate of problems than did Australia in the pre-hospital stage and the transfer stage between hospitals.
4 Therefore, to reduce the PTDR in Korea, it is necessary to transfer within a short time to the appropriate treatment institution to receive the final treatment.
This study has the following limitations. Despite the number of samples increased from the previous studies, there still existed regions where accurate PTDR could not be calculated for each metropolitan city or health service region due to an insufficient number of samples. Therefore, there is a need to increase the number of samples to calculate a more accurate regional PTDR. Furthermore, we could not consider individual patient factors such as the residential area, socioeconomic status, and concomitant diseases that might be associated with preventability of death, as the NEDIS dataset used for this study does not include this detailed information.
Despite these limitations, this study has implications for the purpose of calculating the PTDR in Korea using structured panel review methods and nationally representative samples. Although the PTDR in Korea has been steadily declining, it is still high compared with the PTDR in developed countries. In this study, the PTDR was lower as the time elapsed from accident to death was shorter and the final destined institution was an RTC. To reduce the PTDR in Korea, it is necessary to make an effort to transfer trauma patients to RTCs directly within an appropriate time after the proper field triage is performed. This study showed that continuous and systematic evaluation of PTDR is essential to monitor the trauma system performance and identify opportunities for improvement.

 , where
, where  is the design weight of sample hospitals. The nonadjh is the adjustment value for non-response of sample hospitals, and
is the design weight of sample hospitals. The nonadjh is the adjustment value for non-response of sample hospitals, and  corresponds to death weight in the sample hospitals. In the benchmarking adjustment using the population information, the death distribution of the population in respect of region × type of emergency medical institutions, type of emergency medical institutions × characterization of deaths, region × characterization of deaths was used. The characteristic layer of death distinguished between age and location of death, divided into 7 layers. We applied the raking ratio method to the population information to calculate the final weights by correcting the primary weights of the sample deaths.
corresponds to death weight in the sample hospitals. In the benchmarking adjustment using the population information, the death distribution of the population in respect of region × type of emergency medical institutions, type of emergency medical institutions × characterization of deaths, region × characterization of deaths was used. The characteristic layer of death distinguished between age and location of death, divided into 7 layers. We applied the raking ratio method to the population information to calculate the final weights by correcting the primary weights of the sample deaths.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download