The detection of drowsiness during driving a car is of utmost importance to prevent car accidents, especially when driving a long distance on a monotonous route. Drowsy driving can cause critical car accidents and result in severe injuries and even death of innocent people, as well as the driver and passengers.
However, until now, specific methods have not been developed to prevent driver's sleeping or detecting the time point of falling asleep during car driving, let alone alarming technology to prevent falling asleep.
To develop a device or a tool detecting and preventing sleepy driving, vital sign changes, especially heart rate (HR), ought to be investigated. As a general concept and textbook wise, it is well known that in the initial sleeping state, the HR reduces at the non REM step of sleeping, which is the initial step in sleeping.
12
There has been, as far as we know, no study regarding the change of HR while falling asleep in driving a car. Data on HR change while driving a car, not related to sleepiness, is also very rare.
3
We performed this pilot study to assess the change of HR while driving a car, including at the time of falling asleep, and to compare it with day time daily HR and HR at night sleeping.
From July 18, 2016 to April 13, 2017, healthy volunteers aged 20–50 were recruited who were planning to drive a long distance and/or long time and had a high probability of sleeping while driving, which is dependent on the person's experience. They were healthy and had no diseases nor took any regular medications. They were instructed not to take any medication nor coffee, tea, etc. with caffeine within 3 days before the study.
They were all monitored with a 24-hour Holter during driving a car and daily life for 24 hours. The Holter system was applied, detached and analyzed in Hallym University Sacred Heart Hospital Cardiovascular Center in Anyang, Korea. The driving route was determined by the volunteer and was majorly a long highway. For ease of driving, the car was a sedan of the driver's own. Drivers were instructed to have at least one other person sit in the car in the front passenger side to help detect the sleepy time point and to prevent a traffic accident caused by sleepy driving. Sleepiness was rated subjectively by the driver himself or by the passenger with the Karolinska Sleepiness Scale (KSS, 9-point scale from 1-“very alert” to 9-“very sleepy, fighting sleep”).
4 Sleepiness in driving is defined if the sleepiness scale with KSS is over 8 (sleepy, but some effort to keep awake) or 9 (very sleepy, greater effort to keep awake, fighting sleep). The time point of sleepiness is judged by the driver's subjective feeling and by a person in the front passenger side seat who closely monitored the driver's status including talking, yawning, eye lid blinking and closure. The sleepiness time point was reported by the front passenger.
If the driver could not help sleeping and felt unable to drive safely, they were instructed to pull the car over. The assessment of whether the sleepy driving was dangerous enough to stop driving and whether they should change seats was determined by the driver himself or the passenger in the front side seat. The Holter monitoring was sustained after the driving and the whole 24 hours HR was recorded and analyzed. The definition of daytime is from 8 AM to 8 PM. All participants provided a written informed consent.
The outcome measures are, mean HR and day/night mean HR, mean HR during driving a car, mean HR during sleepy state while driving a car and mean HR during normal sleeping at night.
The primary outcome is mean HR change while sleepy driving as compared to that of whole driving time and day time. Secondary outcomes are to compare HR while driving irrespective of sleepy status with day time mean HR.
The protocol was approved by the Institutional Review Board (IRB) at our institution (IRB No. HALLYM 2019-01-012). All patients provided informed, written consent.
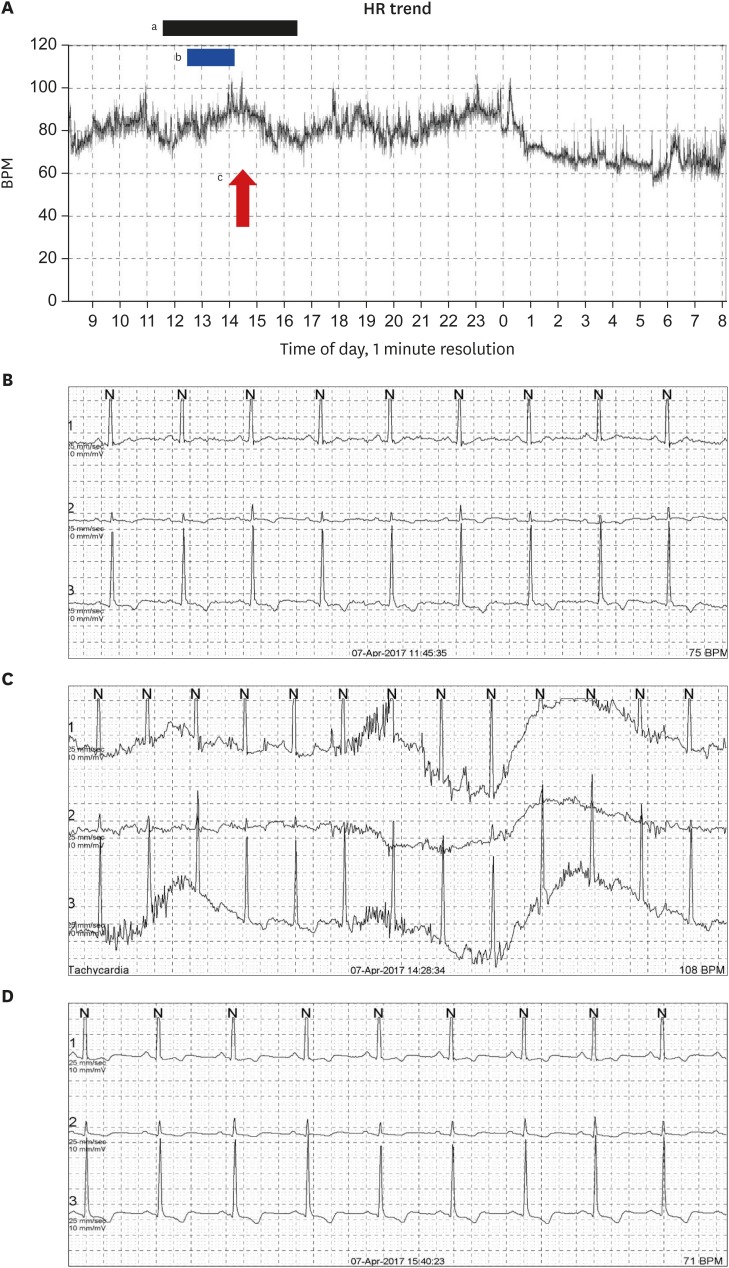
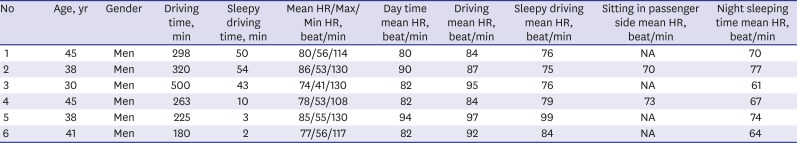
Six healthy volunteers who were planning to drive a long journey were enrolled. They were all men and 39.5 ± 5.6 years old of mean age (median, 39.5; interquartile range [IQR], 9). Their mean and median driving time was 297.7 ± 111 minutes and 280.5 minutes (IQR, 151). They drove mostly on an express way. They felt sleepy 2 ± 1 hours after starting driving and the mean and median duration of sleepy time while driving were 27 ± 24.5 and 26.5 minutes (IQR, 48), respectively (
Table 1).
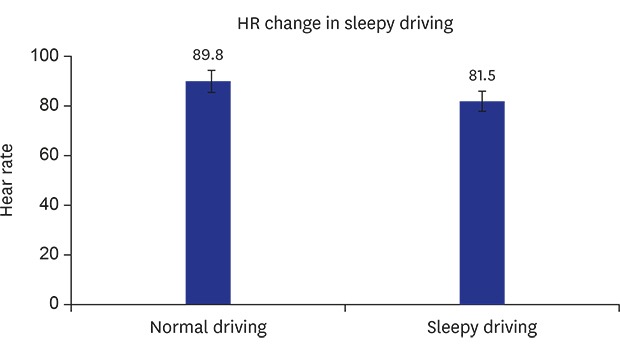
The mean HR while driving significantly increased from 80 ± 4.7 beats/min (total period HR) to 89.8 ± 5.6 beats/min by 12.6% (P = 0.028 by Wilcoxon singed rank test). Driving HR showed the trend for increment as compared to day time mean HR of 85 ± 5.6 beats/min (by 7%) (P = 0.093 by Wilcoxon singed rank test).
Their mean HR while sleepy driving was significantly decreased by 9.3% ± 7.4% from 89.8 ± 5.6 beats/min (driving HR) to 81.5 ± 9.2 beats/min (
P = 0.046 by Wilcoxon singed rank test) (
Fig. 1).
When they slept at night, the HR significantly decreased from 85 ± 5.6 beats/min (day time) to 68.8 ± 6.0 beats/min (sleeping at night) by 19% ± 4.9% (P = 0.028 by Wilcoxon singed rank test).
Two volunteers changed seats from drivers' side to passengers' side when they could not help sleeping. Their HR deceased more prominently from 81.5 ± 9.2 while sleepy driving to 71.5 ± 2.1 beats/min while sleeping in passenger's side.
Drowsy driving is a social problem because it causes big traffic accidents. However, there have been few research studies to prevent drowsy driving in the medical research area, and even in the mechanical and electrical fields. Researchers in the non-medical area have pursued the change of eye lid closure, ocular movement, neck motion, and gaze change during sleepy driving and have tried to make an algorithm of these changes in combination with driving circumstances like driving time etc. to detect the sleepy status.
5678
Driving itself is a very complex procedure, enough to draw all the body senses. Accordingly, the sympathetic tone might increase and thus, blood pressure and HR could be expected to increase. However, there has been no data regarding the change of HR and blood pressure while sleepy driving.
The cause of lack of data is mainly attributed to the fact that this kind of study is very hard to perform in humans because drowsy driving is very dangerous and may cause a big traffic accident and even death.
Our study is, as far as we know, the first investigation regarding the HR change in driving a car and even more importantly in the situation of sleepy car driving. Therefore, our pilot study has the value in pioneering those veiled areas and is a promising approach that can be applied in various areas like developing monitoring and alarming devices for drowsy driving.
The main results of our study are that the HR decreases significantly in sleepy driving as compared to the overall driving HR by 9.3% and increased insignificantly in driving by 7% as compared to day time HR.
It is well known that in routine natural sleeping at night, the HR decreases at the initial stage of sleeping which is also demonstrated in our study. However, in the setting of driving, the HR change could increase or decrease or stay neutral because the parasympathetic and sympathetic activation due to both sleepiness and driving itself could be mixed.
9 Our data support the decrement of HR in sleepy driving.
There are some limitations of this study. First this is a small pilot study including very specific volunteers who are healthy. In the real world, a variety of people are driving and sleepy driving. However, this pilot study has value in attempting for the first time to find the HR change during drowsy sleeping. Secondly, the time point of falling asleep is not definite because we are totally dependent on the driver' subjective talk or passengers' feeling regarding the drowsy driving. Therefore the time point may not be accurate. Theoretically we ought to use electroencephalography for detecting the true sleeping status. However, we used objective methods of estimating the sleepiness level with KSS. Thirdly, this pilot study could cause a traffic accident. But a passenger accompanied the driver in the front side and kept an eye on him and continuously talked to him to detect the time point of his drowsiness. They switched drivers if the driver told that he could not help sleeping or the passenger considered that the driver could not drive anymore. Therefore, this pilot study was completed safely without any accident. Fourthly, the driving route and driving time were not standardized, but just chosen by the driver's needs. This could matter because the conditions of the road and traffic jams might influence the ease or level of arousal of the driver.
Despite those limitations, our study has the strength in that it is the first one dealing with the HR change of drivers in actual driving situation not a simulated driving. More importantly, this is the first study that collected data regarding sleepy driving.
In conclusion, our study for the first time revealed that HR decreased while sleepy driving and the HR increased in car driving. Although larger clinical data will be needed to confirm our findings, our results will help to develop alarming methods for preventing sleepy driving.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download