INTRODUCTION
Endometrial cancer is the most common of the gynecologic malignancies in developed countries, and the age standardized incidence rate (ASR) is 14.7 per 100,000 women-years, especially in Northern America and Central-Eastern Europe (ASR, 19.1 and 15.6 per 100,000 women-years, respectively). However, the average of incidence in South-Central Asia is lowest (ASR, 2.7 per 100,000 women-years) [
1]. In Thailand, the incidence of endometrial cancer increased from; 2.9 to 4.3 per 100,000 women-years, in 1997 through till 2012, respectively [
23]. This was also the same in the Songkhla Province, South of Thailand (ASR, 2.1 and 4.7 per 100,000 women-years in 1997 and 2012, respectively) [
2], and the average of ASR is 3.8 per 100,000 women-years [
4].
The trend in incidence of endometrial cancer increases in accordance with the increasing incidence of the risk factors, and is associated with many factors especially: metabolic syndrome; obesity [
5], hypertension [
6] and diabetic mellitus [
78] (relative risk [RR] = 1.80-19.75). Additional, hormone replacement therapy (HRT) in postmenopausal women, especially estrogen alone, has increased the risk of endometrial cancer (RR=2.3), however, estrogen plus progestin is a risk reducer of endometrial cancer. Hazard ratio (HR) is 0.40–0.83 [
91011], this is the same as oral contraceptives pills, that are used for contraception in premenopausal women. The RR is 0.57–0.69 [
912].
The objectives of this study are to define incidence of uterine cancer in the present, and the trends of incidence in the future. Additional, subgroup analysis in religion, and socio-demographic factors will be analyzed.
RESULTS
A total of 742 cases in this study were diagnosed with uterine cancer, using ICD-10 codes C54 for corpus uteri were 690 cases (93%), and C55 for uterus unspecified were 52 cases (7%). The stage of disease was adjusted, following the International Federation of Gynecology and Obstetrics stage 2009, the patients with stage I, II, III, and IV cancer were 52.7%, 7.5%, 15.4% and 5.9%, respectively. However, 18.5% of patients were unable to inform as to their stage of disease. The ethnicities were recorded as Thai and Chinese; 99.7% and 0.3%, respectively. The religion majority was Buddhism 88.4%, the others being; Islam 10.5%, Christianity 0.4%, and no data 0.7%.
The ASR of uterine cancer in Songkhla Province was 1.54 per 100,000 women-years in 1989, and increased to 5.30 per 100,000 women-years in 2016, with the annual percent change being; 4.6% per year. Using the projections of incidence in 2017–2030, the ASR would increase to 8 per 100,000 women-years, and the trend will be steady in both the Joinpoint and APC models, but increasing in Nordpred analysis (
Fig. 1). The peak incidence of age, at diagnosis, was between 55 to 64 years, which is mainly in postmenopausal women, and the year of birth was between; 1945 and 1960 (
Table 1 and
Fig. 2).
Fig. 1
Uterine cancer incidence trend projections to 2030 by Joinpoint, APC, and the Nordpred model.
APC, age-period-cohort; ASR, age standardized incidence rate.

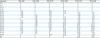
Table 1
The age-specific incidence rate of uterine cancer by age group, and 5-year intervals from 1989–2016
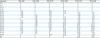
|
Age group |
1989–1991 |
1992–1996 |
1997–2001 |
2002–2006 |
2007–2011 |
2012–2016 |
|
0–4 |
0 |
0 |
0 |
0 |
0 |
0 |
|
5–9 |
0 |
0 |
0 |
0 |
0 |
0 |
|
10–14 |
0 |
0 |
0 |
0 |
0 |
0 |
|
15–19 |
0 |
0 |
0 |
0 |
0 |
0 |
|
20–24 |
0.37 |
0 |
0.34 |
0.32 |
0 |
0 |
|
25–29 |
0.39 |
0 |
0.35 |
0.35 |
0.70 |
0.72 |
|
30–34 |
0.89 |
0.41 |
0.74 |
0 |
0.98 |
1.76 |
|
35–39 |
1.64 |
2.36 |
1.18 |
2.13 |
1.65 |
2.30 |
|
40–44 |
0 |
2.31 |
4.61 |
0.79 |
2.45 |
6.77 |
|
45–49 |
2.47 |
4.90 |
8.03 |
7.02 |
7.67 |
5.77 |
|
50–54 |
2.62 |
4.88 |
15.53 |
14.96 |
16.83 |
17.45 |
|
55–59 |
2.15 |
11.08 |
12.00 |
14.89 |
27.73 |
23.44 |
|
60–64 |
5.21 |
5.77 |
12.91 |
12.14 |
23.44 |
29.83 |
|
65–69 |
10.19 |
8.3 |
9.05 |
8.82 |
18.43 |
25.85 |
|
70–74 |
5.03 |
8.34 |
8.3 |
13.82 |
15.27 |
24.11 |
|
75–79 |
3.47 |
3.14 |
0 |
4.09 |
10.28 |
17.04 |
|
80–84 |
0 |
0 |
8.79 |
6.63 |
4.76 |
7.09 |
|
85+ |
0 |
0 |
0 |
0 |
13.12 |
10.10 |
Fig. 2
The APC trend analysis of uterine cancer. AP-C (orange) and AC-P (blue) models.
APC, age-period-cohort.

The habitat of patients in the Songkhla Province; the incidence of uterine cancer in the urban areas was significantly more than within the rural areas by; 2.21 times (risk ratio=2.21; 95% CI=1.30–3.12; p<0.001), however the increasing rate was slower (annual percent change was 3.27% [p<0.001] and 5.44% [p<0.001] per year, respectively) (
Fig. 3).
Fig. 3
Trend in incidence of uterine cancer by habitat of patients; urban (blue) and rural (orange), by log10 ASR per 100,000 population.
APC, annual percent change; ASR, age standardized incidence rate.

The religion of patients in the Songkhla Province, before the year 2000, had the incidence of uterine cancer in Buddhists lower than in Muslims, however after the year 2000, the incidence was more within the Buddhist population. The overall incidence in Buddhists was more than in Muslim by; 1.19 times, this was, however, not statistically significant (95% CI=0.21–2.17; p=0.02), although the increasing rate was faster (annual percent change was 4.30% [p<0.001] and 2.13% [p=0.2] per year, respectively) (
Fig. 4).
Fig. 4
Trend in incidence of uterine cancer by religion of patient; Muslim (blue) and Buddhist (orange).
APC, annual percent change; ASR, age standardized incidence rate; BPSP, Buddhists predominant subpopulations; MPSP, Muslims predominant subpopulation.

DISCUSSION
The ASR of uterine cancer in Songkhla Province was; 1.5–5.3 per 100,000 women-years, including C54 and C55, which was a minimal difference in the results, when compared to analyze by C54 alone. The ASR in this study was lower than in the USA, United Kingdom and Singapore. The trends in incidence are increasing, much the same as in the United Kingdom and Singapore, while as in the USA there has been a steady decrease by; 19 per 100,000 women-years since 1985 (
Fig. 5) [
19]. The ASR of endometrial cancer, from a population-based study in the Songkhla Province, was lower than in Korea [
20] Taiwan [
21], Romania [
22], Turkey [
23], Croatia [
24], and Netherland [
25], which were 7.0, 7.5, 8.2, 10.4, 11.4, and 20.1 per 100,000 women-years, respectively, but higher than in; Tunisia [
26] and mainland China [
27], which were 3.1 and 5.0 per 100,000 women-years, respectively. The annual percentage change of uterine cancer within the Songkhla Province was; 4.6% per year, which was lower than Tunisia [
26] (7.1% per year), but higher than Turkey [
23] and the Netherlands [
25] (2.4% and 3.4% per year, respectively). However, these studies reported incidence between 2003 and 2013, in this study we reported recently in 2016. The projections of ASR in 2017–2013 were; 8 per 100,000 women-years, which was steady in both the Joinpoint and APC model, but increasing in Nordpred analysis. The Joinpoint model calculated the projection, according to the period-effected, but not on the age-structure of the population, whereas both the APC and Nordpred models accounted for all the ages, periods and birth cohort-effects. The projection of the APC and Nordpred models was based on the age-period-cohort effects, while the Nordpred model based its calculation on 5-year periods. The projection of ASR in this study was lower than the United Kingdom (ASR, 20.0 and 33.1 per 100,000 women-years in 2007–2030 [
18] and in 2015–2035 [
28], respectively). The incidence of endometrial cancer was increasing in correlation with the increasing risk factors of uterine cancer. The highest of the RR was morbid obesity [
5] (body mass index [BMI] ≥40 kg/m
2; RR=19.79; 95% CI=11.18–35.03). The RR of diabetic mellitus and hypertension in endometrial cancer were; 1.63–2.10 [
78] and 1.61 [
6], respectively. The incidence of females, who had BMI ≥25 kg/m
2, diabetic mellitus and hypertension, in South of Thailand was increasing from 36.3%, 9.9%, and 11.6% in 2003 to 43.7%, 10.6%, and 18.0% in 2014, respectively [
2930]. These factors occurred in high-income countries, although Thailand is one of the middle-income counties, the income of the country is increasing. Gross domestic product; GDP per capita (purchasing power parity) was; $4,298 in 1990, and $16,913 in 2016 [
31]. Socio-economic status was associated with lifestyle, especially food-styles, which might lead to an increase in these risk factors. The possible role of diet in endometrial cancer was not significantly related; however, there was a protective risk in healthy dietary patterns (RR=0.83; 95% CI=0.67–1.04), and an increasing risk in unhealthy dietary patterns (RR=1.19; 95% CI=0.99–1.43) [
32].
Fig. 5
ASR (World) of endometrial cancer in the USA, the United Kingdom, Singapore, and Thailand. The data were used from CI5 plus [19], and the data of Songkhla, Thailand was used from this study).
ASR, age standardized incidence rate; SEER, Surveillance, Epidemiology, and End Results Program.

The culture as well as values of women in Thailand, including; the age of marriage coupled with the number of children, has changed from that of the past, with the average age of marriage increasing, whereas the parity was decreasing. The average age of marriage was increasing from 22 years in 1970, to 24.9 years in 2010, and the number of singlehood in each age group was increasing, too. The number of singlehood in the age-group 20–24, 25–29, 30–34, 35–39, and 40–44 was 37.9%, 15.6%, 8.1%, 5.2% and 3.9% in 1970; and 59.7%, 38.3%, 23.5%, 14.6% and 10.6% in 2010, respectively [
33]. The total fertility rate (TFR) was 6.147, 5.595, 3.392, 2.113, 1.671, and 1.482 in 1960, 1970, 1980, 1990, 2000, and 2016, respectively [
31], although, the age at last birth has decreased, endometrial cancer risk, when the age at last birth was increasing (odd ratio [OR]=0.87; 95% CI=0.85–0.90). The women, who had their last child at age 40 or older, had a 44% decreased risk of endometrial cancer, compared to women who had their last child under the age of 25 (OR=0.56; 95% CI=0.47–0.66) [
34].
The peak incidence of age at diagnosis was between; 55 to 64 years, the same as in Korea [
20], Taiwan [
21] and Turkey [
23], but lower than Romania [
22], and Tunisia [
26]. The peak incidence in these age groups was mainly in postmenopausal women, and the year of birth was between; 1945 and 1960 (
Fig. 2). The period after World War II, which promoted an increase in fertility, hence people born in 1946–1964 are known as ‘the baby boomer generation.’ The incidence of obesity was also increasing in the baby boomer generation, when compared to an earlier generation in the USA [
35]. At the same time, in 1937 the government of Thailand promoted high parity too, but the data of obesity in Thai people could not be noticed. The policy of family planning was first introduced in 1961, with contraceptive pills and condoms being initially used in 1970. The intrauterine device and the injection of contraception were additional used, and obtained full coverage of 100% in 1985 [
36], which was for females born in 1945-1960, entering into their reproductive period during in this period. The birth rate decreased from; 42.7 per 1,000 people in 1960, to 22.1 per 1,000 people in 1985, and 10.3 per 1,000 people in 2016 [
31]. Estrogen replacement therapy was strongly associated with the increased risk of endometrial cancer, but the combined estrogen and progesterone replacement therapy along with oral contraceptive pills decreased the incidence of endometrial cancer [
10123738]. The dose of estrogen in oral contraceptives was a high-dose (100 µg or more) before 1970, and decreased to a medium-dose (50 µg) between 1970 and 1980, then to a low-dose (35 µg) by 1980, however the dose of estrogen was not associated to the risks of endometrial cancer, rather is was associated with duration of usage [
39]. The peak of incidence in the years of birth was; between 1945 and 1960, in Songkhla, and this may have affected the ‘baby boomers,’ and HRT, after that the rate decrease might have been affected from careful HRT, and commonly used contraceptive pills.
The incidence of uterine cancer in urban areas was significantly more than that of rural areas by; 2.21 times, the same as in China (ASR, 6.2 and 3.0, respectively) [
27]. The risk of endometrial cancer in people, who live in urban areas, was null or decreases in number of parity, obesity, and a higher incidence of metabolic syndrome. The annual percent change in the rural areas was more than the urban areas, due to; life-style changes in rural areas as well as the migration of the population.
There were 3 sub-nationalities of people in Songkhla – Thai, Thai-Chinese, and Thai-Malay; however, most people were registered as Thai-ethnicity. Thai-Malay's were mostly Muslim, with most living in the 3 districts of; Chana, Saba Yoi, and Thepa, whereas the Thai and Thai-Chinese were Buddhist. Our analysis of the incidence of uterine cancer used the age-period-cohort and joinpoint models, because we did not have the denominators of religious groups by age group, and gender of the Songkhla population, which were required for a Poisson model. Hence, we chose the 3 districts of Chana, Saba Yoi, and Thepa where, as the percentage of Muslim was around 75%, and we could use this as a proxy, sub-population representing Thai-Malay Muslims. The other 13 districts were representative of Thai/Thai-Chinese, and in turn we could approximate the Buddhist sub-population of Songkhla. The incidence of cancer in Buddhists was lower than in Muslims, however, this was higher, and increasing faster in trends than in Muslims after 2000. Singapore has many different ethnicities in their country; incidence of endometrial cancer was more in the Chinese population, much the same in Songkhla (
Fig. 5). There were differences in the risk factors of endometrial cancer in both Buddhists and Muslims; number of parity and contraception. In the data from Thai National Statistical Office in 2004, the Buddhists had a lesser, average number of parity (1.94 and 2.74 persons), that increased the risk of cancer, but used more contraception, which decreased the risk of cancer (83.2% and 49.5%, respectively) [
40].
The information in this study was extracted from the cancer registry in Songkhla, which was population-based, and the prospective data had a long period of collection (Beginning in 1989 until the present), thus there was no bias from the collecting method. However, the data from the cancer registry lacks data of a demographic type, and the risk factors for endometrial cancer for each individually person, such as: actual ethnicity, income status, parity, contraception, or HRT, nutritional data, BMI, presence of diabetic mellitus, and hypertension. Therefore, some risk factors of endometrial cancer were indirectly analysis from the national data, instead of the provincial data. Additional, the data of habitat and religion were not true values; these were only representatives of each group. However, the result from this study might represent the overall results of the population in Songkhla. Since the cancer registry is aimed at collecting the incidence cases, and deaths are identified through the registration system for the compilation of cause-specific survival, the mortality rate for endometrial cannot be directly calculated from the cancer registry, as it is always over estimated by other causes of death, which may complicate the course of the disease. Thus, the researchers are going to report the cause-specific net survival of the disease in another analysis.
The incidence of uterine cancer, in Songkhla Province has been increasing from; 1.5 to 5.3 per 100,000 women-years in 2016, and 8 per 100,000 women-years in 2030. The incidence was more in urban areas and in Buddhists. A policy, which promotes protective factors, and control risk factors would decrease incidence of endometrial cancer as well as other estrogen dependent cancers, additional to chronic diseases from cardiovascular system.








 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download