This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Isolated iliac artery aneurysm (IIAA) is uncommon. It is frequently treated by endovascular aneurysm repair (EVAR). This study was to evaluate treatment results of IIAA and survey aortic diameter after EVAR.
Methods
Patients treated for IIAA in Seoul St. Mary's Hospital and Bundang Seoul National University from 2005 to April 2016 were retrospectively enrolled. The inclusion criteria of IIAA was >30 mm of iliac artery aneurysm without abdominal aortic aneurysm, which was treated by open surgical repair (OSR) or EVAR. Patients' clinical characteristics, treatment results, and mortality were obtained from electronic medical records. Diameters of aorta and iliac arteries were measured periodically with scheduled interval based on CT scans.
Results
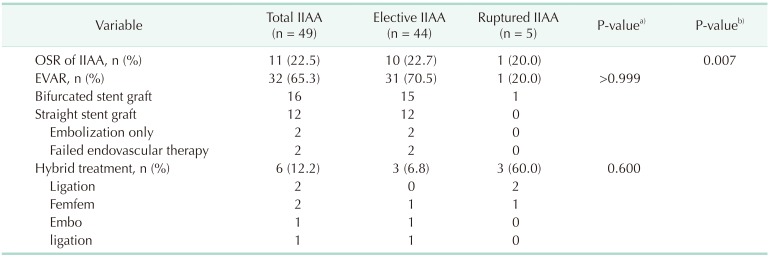
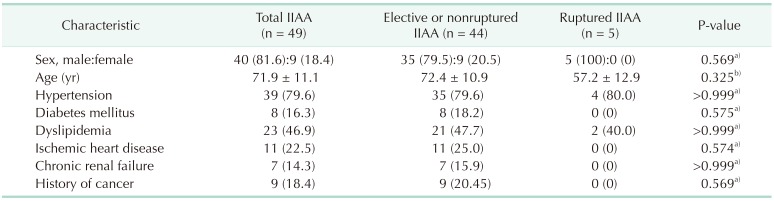
Forty-nine patients (40 males; mean age, 71.9 ± 11.1 years) were enrolled. Five ruptured IIAAs were treated with EVAR (n = 1) or hybrid methods (n = 4). The diameter of ruptured IIAAs was 65 ± 31.4 mm, which was not significantly different from that of elective (44.3 ± 17.0 mm). Forty-four elective IIAA underwent 9 OSR, 31 EVARs, and 3 hybrid treatments (15 bifurcated and 12 straight stent-grafts). Treatment success rate was 93.8% without hospital mortality. There were 4 type I endoleak, 1 type II endoleak, and 1 type III endoleak without aneurysm-related mortality during follow-up. However, the aortic diameter was increased over time though there was no change or decrease in common iliac artery's diameter.
Conclusion
Treatment of IIAA included various endovascular modalities as well as open surgery. Regular surveillance is still needed due to aortic dilatation after its treatment.
Keywords: Aneurysm, Iliac artery, Iliac aneurysm, Endovascular procedure
INTRODUCTION
Isolated iliac artery aneurysm (IIAA) is relatively uncommon, accounting for 2%–7% of all abdominal arterial aneurysms [
123]. Open surgical repair of IIAA has been a treatment of choice. Since elective endovascular aneurysm repair (EVAR) for abdominal aortic aneurysm (AAA) has become a standard treatment [
4], it is also becoming popular for IIAA. However, information on its result remains limited [
5]. Therefore, objective of this study was to evaluate treatment outcomes of IIAA and changed of aortic diameter after EVAR.
METHODS
This was a retrospective study from prospectively registered database of patients who underwent surgical or endovascular treatment of IIAA in Seoul St. Mary's Hospital and Bundang Seoul National University from 2005 to April 2016. This study was approved by the Institutional Review Board of The Catholic University of Korea (approval number: KC18REDI0006). The informed consent was waived due to retrospective study. Inclusion criterion of this study was: IIAA > 30 mm without aortic aneurysm. IIAA was defined as either single or multiple aneurysms located within the common, internal, or external iliac arteries. Patient characteristics, comorbidities, presentation, and symptoms were reviewed using electric medical record and picture archiving and communication system. Contrast enhanced CT images were used to assess IAA location and diameter and plan repair. The decision to proceed with open surgical repair or EVAR was at the discretion of the surgeon based on anatomy and comorbidities as well as urgency of the repair.
Operative data included type of repair, anesthetic technique, procedural time, estimated blood loss, intraoperative complications, graft type utilized, and need for hypogastric coil embolization. At the time of endovascular repair, bilateral femoral arterial access was obtained percutaneously on the contralateral side and by cut-down on the ipsilateral side (or through bilateral femoral cut-down if a bifurcated device was to be used). All patients underwent intraoperative aortic and pelvic angiography with a marker catheter for appropriate length measurement. A proximal and distal fixation zone of 15 mm was desirable for endovascular repair of common and external IAA to obtain a good sealing zone. Coil embolization of the origin of the internal iliac artery (IIA) was performed to achieve an appropriate distal fixation zone in common iliac aneurysms extending into the external iliac artery while avoiding type II endoleak. For aneurysm involving the hypogastric artery or isolated hypogastric aneurysms, distal branches of the hypogastric (anterior and posterior division) were coil-embolized and the origin of the internal iliac was covered by a stent-graft extending to the external iliac artery. In cases of bilateral common iliac artery aneurysm (CIAAs) or CIAAs with short proximal necks (<1.5 cm), bifurcated modular devices were used. For most cases, at least one hypogastric artery was tried to be preserved. Open surgical repair included aortoiliac reconstructions or crossover femorofemoral bypass with iliac ligation. Acute kidney injury was defined following RIFLE classification; an increase of creatinine level greater than 50% of the patient's baseline, or decrease of glomerular filtration rate greater than 25%. Bowel ischemia was either endoscopically documented or clinically suspected based on elevated WBC and physical examination findings. Myocardial infarction was identified by consulting cardiologists based on electrocardiogram changes and troponin values. Wound infection was identified based on clinical factors and wound cultures. On follow-up, late aneurysm-related and systemic complications were recorded, including the presence of claudication. All patients who underwent EVAR had computed tomography angiogram postoperatively at 1 month, 6 months, and yearly thereafter for uncomplicated cases to monitor the aneurysm diameter and the presence of any endoleak. An increase in IAA short-axis diameter of >5 mm or attachment site endoleak prompted further workup with angiography and possible secondary intervention. Follow-up after open repair included physical examination at 2 weeks postoperatively and then yearly thereafter. Imaging was not routinely obtained. It was used selectively to address specific clinical situations. Diameters of aorta and both iliac arteries after EVAR were measured with CT scan at 1 month, 6 months, 1 year and yearly thereafter to evaluate chronologic change of arteries depending on treatment options for isolated IAA. The diameter of the vessel was measured from outer wall to outer wall across the short axis of the vessel in the largest image slice.
Patients' demographics, pathologic characteristics of IAA, and treatment options were summarized and compared. Categorical variables were compared with Fisher exact test while means were compared using Student t-test. Annual changes in diameters of arteries including aorta, right common iliac artery, and left common iliac artery after IAA treatment were analyzed using mixed model with autoregressive covariance structure for repeated measures. For this analysis, diameter values of arteries were log-transformed due to their non-normality. All statistical analyses were performed using SAS version 9.1.3 (SAS Institute Inc., Cary, NC, USA). Statistical significance was considered at P < 0.05.
RESULTS
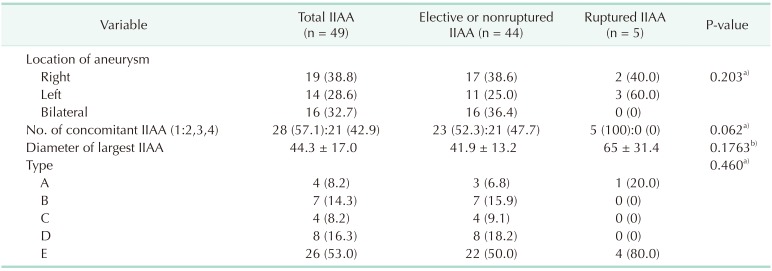
From 2005 to April 2016, 49 patients (9 females and 40 males) with a mean age of 71.9 ± 11.1 years were enrolled, including 44 cases of elective aneurysm repairs (2 mycotic aneurysms) and 5 ruptured aneurysms (
Table 1). Common iliac artery was the most frequently involved (77.6%, 38 patients). Sixteen patients (33.3%) had internal IAA while 9 patients had isolated internal IAA (
Table 2).
Five patients (14.3%) with ruptured IAA were emergently treated by endovascular method (n = 1) or hybrid method (n = 4). The mean diameter of ruptured cases was 65 ± 31.4 mm, which was not significantly (P = 0.176) different from that of elective cases (41.9 ± 13.2 mm). Technical success rate and in-hospital mortality of emergency treatment of ruptured IIAA were 100% and 0%, respectively.
Among 44 elective cases, open surgical repair was performed for 9 patients and EVAR was performed for 31 patients. Two open surgical repairs were done during kidney transplantation (
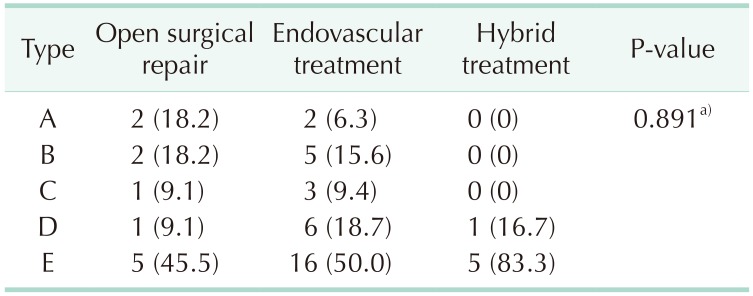
Table 3). EVAR included 15 bifurcated stent-grafts (coil embolization, n = 8; sandwich technique, n = 5; straight stentgrafts with/without coil embolization, n = 12; and isolated coil embolization, n = 2). These cases were classified according to Sandhu classicification [
6] (
Table 4). At least one IIA was saved in 93.9% (46 of 49) of cases by stenting in CIA (1 of 46), unilateral IIA embolization (22 of 46), ligation (15 of 46), bell-button tech (2 of 46), or sandwich tech (6 of 46).
There were 10 bilateral CIAAs (20.4%). They were treated by open surgical repair (2 of 10) or EVAR (bell button technique, 2 of 10; and sandwich technique, 6 of 10). For 2 patients with IIAA and iliac artery occlusion, the endovascular approach failed. Technical success rate and in-hospital mortality for the group with elective treatment for IIAA were 95.5% and 0%, respectively.
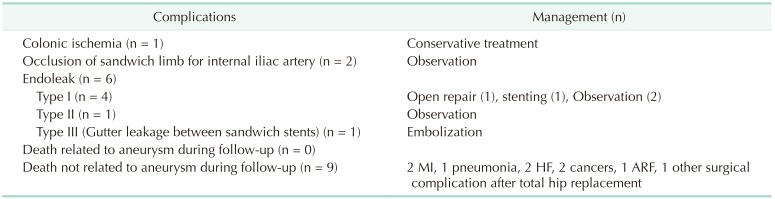
There was no mortality in the emergency or elective treatment group. There was one colonic ischemia in ruptured IIAA which was improved with conservative methods. There were 2 occlusions of sandwich stent graft for IIA in EVAR with sandwich technique during the procedure. The mean follow-up duration was 35.0 months. Nine patients died during the followup period. These deaths were not related to aneurysm. Causes of death were myocardial infarction (n = 2), pneumonia (n = 1), heart failure (n = 2), cancer (n = 2), acute renal failure (n = 1), and other surgical complication after total hip replacement (n = 1). There were type I endoleak in 6 patients during the follow-up. Four cases of type I endoleak were managed by open surgical repair (n = 1), stenting (n = 1), and observation (n = 2). Type II endoleak was observed in one case. One type III endoleak after EVAR with sandwich technique was embolized with n-butyl histoacrylate. Complications are summarized in
Table 5.
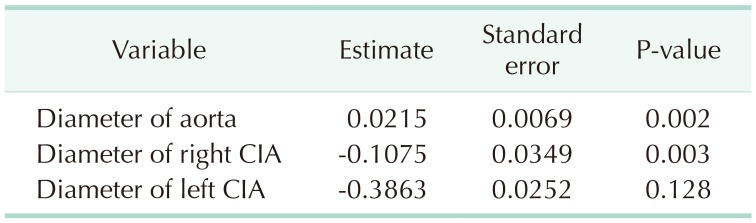
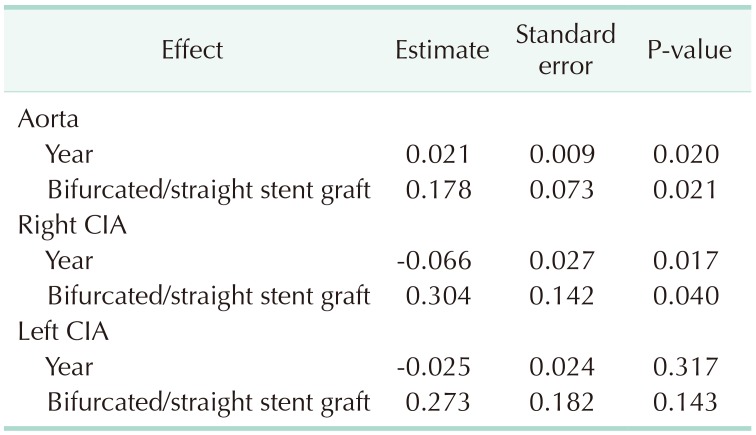
Aorta, right CIA, left CIA diameter were serially measured over time and analyzed using the mixed model for repeated measures. Results are shown in
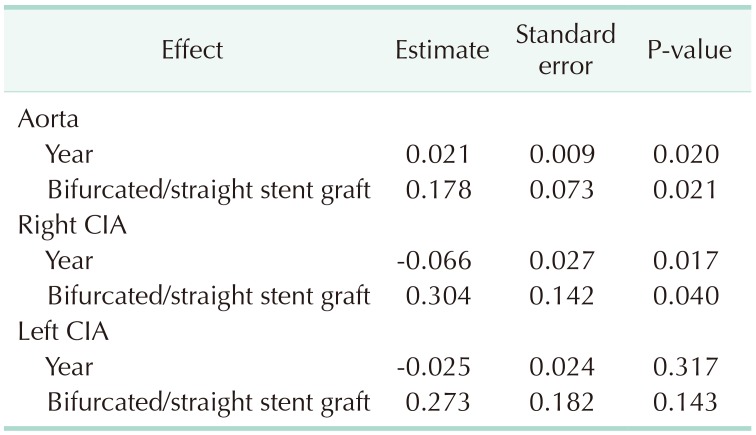
Table 6. During 35 months of follow up after EVAR or hybrid treatment of IIAA, the diameter of aorta was increased after straight stent graft while the diameter of aorta remained unchanged after bifurcated stent graft (
Table 7). However, diameter of aorta or right common iliac artery did not change after bifurcated stent graft (
Table 7).
DISCUSSION
Symptomatic IIAAs including rupture with abdominal pain with or without cardiovascular stability and large aneurysm compressing adjacent tissue such as the ureter need to be intervened. The mean diameter of symptomatic IIAA is 4.5 to 8.5 cm [
78]. However, there is no clear recommendation for aneurysm size in treating asymptomatic IIAA. It is obvious in that IIAA needs to be treated in smaller diameter compared to AAA because of its small nature in healthy tissue. Many researchers have recommended treatment for asymptomatic IIAA with diameter > 3.0–3.5 cm [
8]. In this study, IAAs with diameters > 3.0 cm were treated following Korean health insurance reimbursement assessment. The mean diameter of unruptured IIAA was 44.3 ± 17.0 mm.
Open surgical repair of IIAA has been a treatment of choice for many years until endovascular treatment becomes popular in treating IIAA. However, there is no endovascular device specifically recommended for IAA patients [
910]. Endovascular treatment for isolated CIAA is a non-IFU (indication for use) procedure considering IFU of AAA. Current procedure in treating bilateral IAA is limited by pelvic ischemia including buttock claudication, colonic ischemia, and spinal cord ischemia. Saving one IIA has been an important principle. Common methods of sacrificing one IIA include embolization and surgical ligation. In this study, at least one IIA was saved for 93.9% (46 of 49) of cases by stent grafting within common iliac artery (1 of 46), unilateral IIA embolization (22 of 46), surgical ligations (15 of 46), bell-button techniques (2 of 46), and sandwich techniques saving IIA (6 of 46). There was one bilateral IIA embolization without symptomatic pelvic ischemia.
EVAR for AAA was improved to be durable in EVAR 1 trial. A recent follow-up paper showed inferior results of EVAR for AAA compared to open repair for AAA [
5]. Durability of EVAR for IIAA can be an issue during follow-up. It can be influenced by its indication for use. EVAR within IFU has shown less complications and better durability compared to EVAR outside IFU. EVAR of IIAA is outside IFU. Its durability can be an issue during long-term follow-up [
1112]. Therefore, devices for IIAA are needed. Iliac artery bifurcated device can make EVAR of IIAA within IFU, leading to less complications [
13].
Proximal sealing zone of isolated CIAA is important when selecting devices such as aortic bifurcated devices and straight stent graft [
1314]. This strategy can influence short-term and long-term outcomes. IIAA without proximal sealing zone needs aortic bifurcated devices that can cover aortoiliac arteries including patent inferior mesenteric artery (IMA). There is a possibility of colonic ischemia when patent IMA and IIA become occluded during EVAR. Its durability will be similar to the case of EVAR outside of IFU of AAA due to IAA. Straight stent graft with IIA embolization and proximal sealing zone of IAA seems an easy procedure. However, its durability needs to be evaluated due to possible type I endoleak during follow-up and new aneurysm in other aortoiliac arteries.
Bilateral CIAA without aortic involvement is challenging because saving at least one IIA is technically difficult. Aortic bifurcated devices have been used to save at least one IIA strategy, including external iliac artery to IIA bypass [
15], sandwich stent grafting to IIA [
16], bellbutton technique, and iliac artery bifurcated devices [
17]. Recent retrospective study reported iliac artery bifurcated device is applicable to most Korean patients with AAA and CIAA [
18].
In this study, our options included open surgical repair (2 of 10), sandwich stent grafting to IIA (6 of 10), and belly button technique (2 of 10). External iliac artery to IIA bypass or iliac artery bifurcated device was not done. Embolization stent graft to external iliac artery with IIA embolization has risk of limb occlusion compared to EVAR with belly button technique. Since belly button technique is also known to have risk of type Ib endoleak during follow-up, iliac bifurcated device seems to be an optimal choice based on literature review.
The authors of the present study experienced 2 cases of open repair of IIAA with renal transplantation. Any artificial graft material with renal transplantation can have a risk of graft infection during follow up due to immunosuppression. When combined treatment of aneurysm repair and renal transplantation is needed, complications such as postoperative bleeding should be minimized to prevent graft infection.
The improve trial reported the same result of endovascular treatment ruptured AAA compared to open repair with 1-year follow-up. Emergency EVAR for ruptured IIAA can control active bleeding because proximal sealing zone in its aorta is better than that of ruptured AAA.
Follow-up data of diameter of aorta and common iliac arteries showed opposite results. The aortic diameter was increased while the common iliac artery showed decrease or no change in diameter over time. These results were influenced by treatment options (straight stent graft vs. bifurcated stent graft), implying that concomitant treatment of aorta might be needed regardless of its size. If type I endoleak develops after treatment with straight stent graft, it is difficulty to deploy additional bifurcated device. Thus, interventionist should consider possible placement of bifurcated device during follow-up when straight stent graft is needed for treatment of IIAA.
In conclusion, this study documents various options for emergency and elective treatment of IIAA. Considering aortic size change and additional treatment due to endoleak, durability of endovascular treatment of IIAA needs to be evaluated with regular surveillance program. EVAR with bifurcated stent graft can be a better option for IIAA patient compared to straight iliac stent graft if there is enough proximal landing zone.
Table 1
Clinical characteristics of patients of isolated iliac artery aneurysm (IIAA)
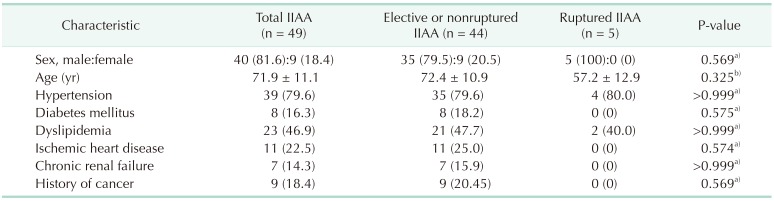
Table 2
Characteristics of isolated iliac artery aneurysm (IIAA) according to Sandhu classification
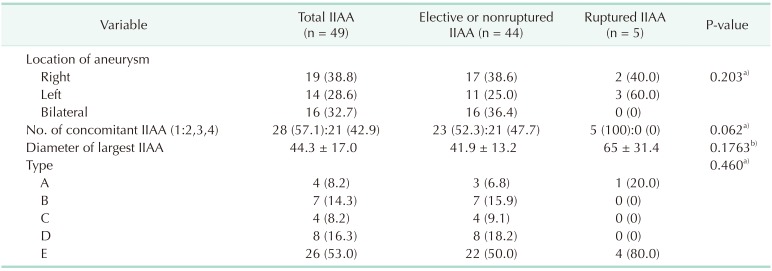
Table 3
Treatment options of isolated iliac artery aneurysm (IIAA)
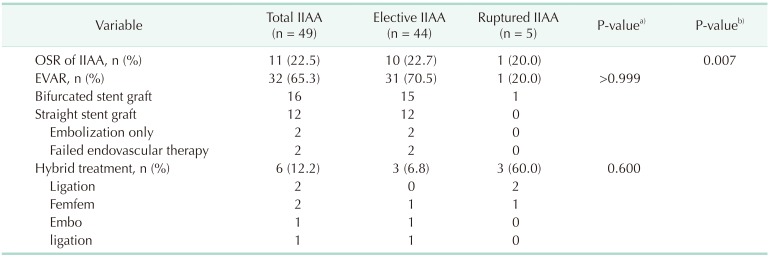
Table 4
Treated options of isolated iliac artery aneurysm (IIAA) according to Sandhu classification
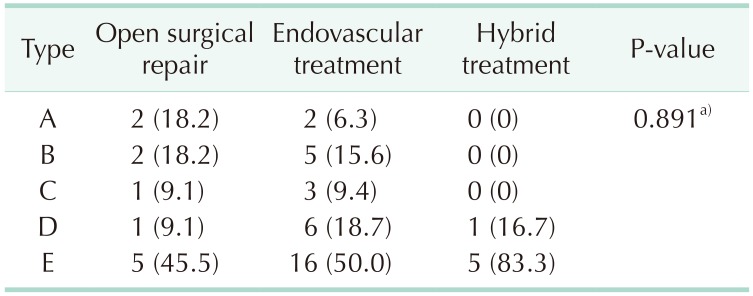
Table 5
Complications after treatment of isolated iliac artery aneurysm
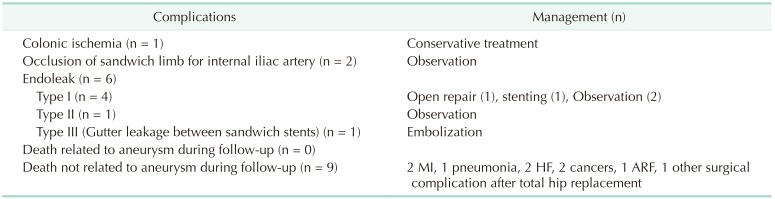
Table 6
Changes in diameter of aorta, right common iliac artery (CIA), or and left CIA over time after treatment of isolated iliac artery aneurysm
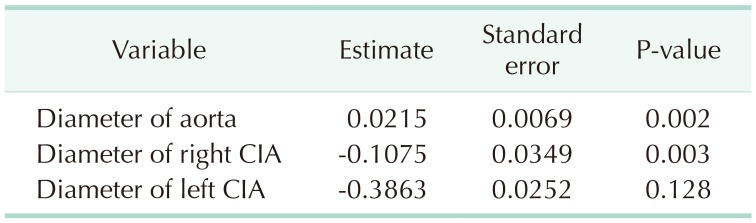
Table 7
Influence of type of stent graft on diameter of aorta, right common iliac artery (CIA), or left CIA over time




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download