INTRODUCTION
Table 1
Correlations of Different Uterine Cervical Tumorous Lesions with High-Risk HPV Infection

Cervical Adenocarcinoma
Endocervical Adenocarcinoma, Usual Type (Figs. 2, 3)
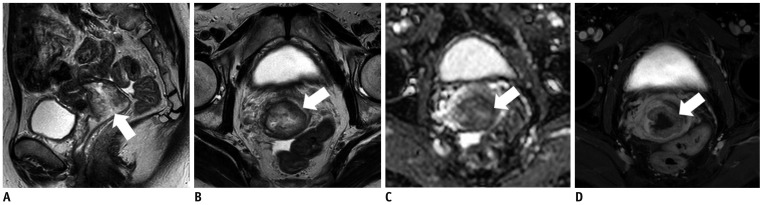
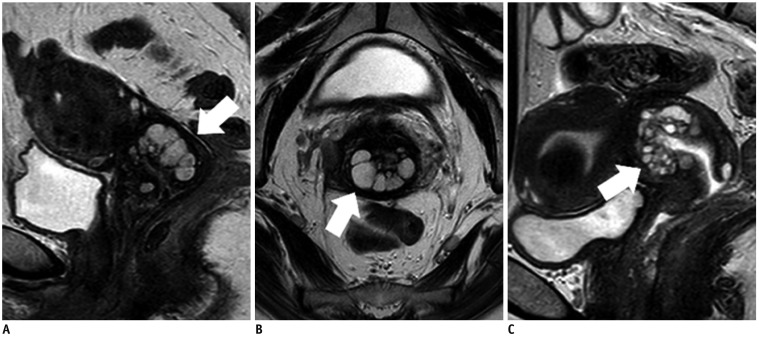
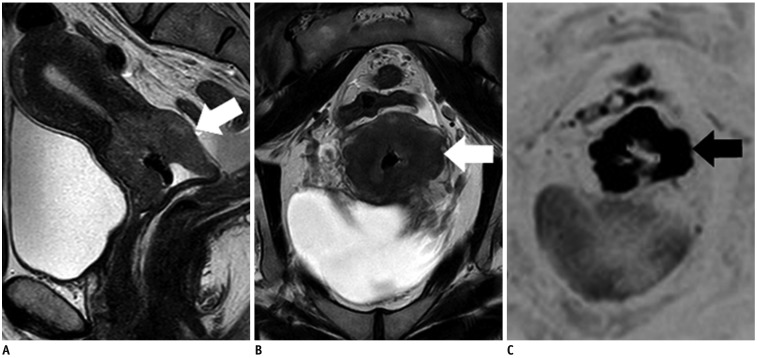
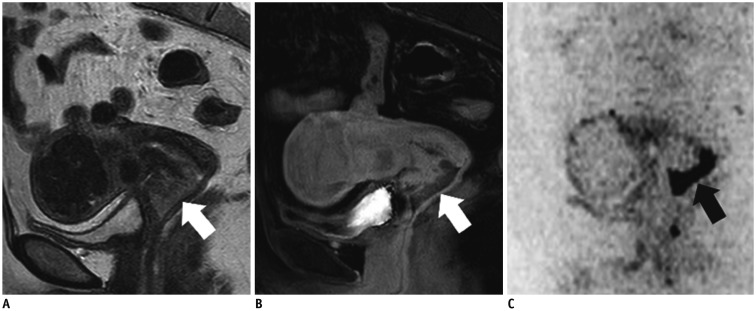 | Fig. 256-year-old woman with endocervical adenocarcinoma, usual type.
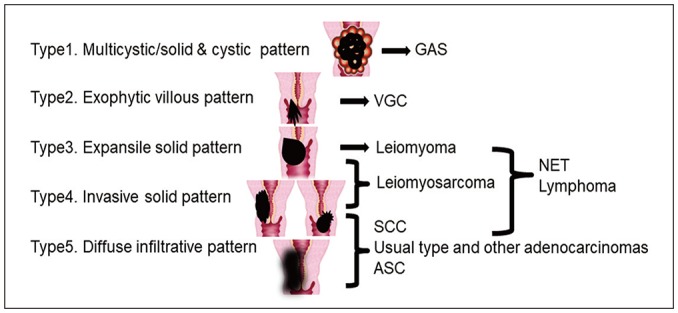
A. Sagittal T2WI shows exophytic tumor (protruding inside canal) in cervical lip (arrow) and indicates invasive solid pattern (Fig. 1; Type 4). This is typical pattern for usual type adenocarcinoma. B. Sagittal contrast-enhanced fat-saturated T1WI shows weak enhancement of tumor (arrow). C. Sagittal DWI shows marked restricted diffusion (arrow). DWI = diffusion-weighted imaging, T1WI = T1-weighted imaging, T2WI = T2-weighted imaging
|
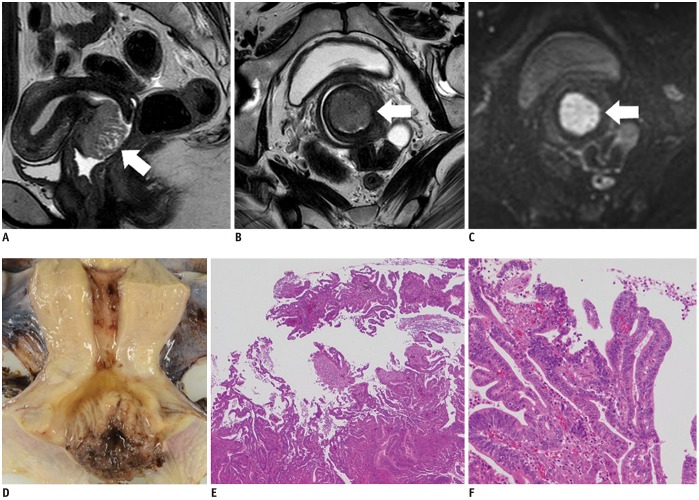
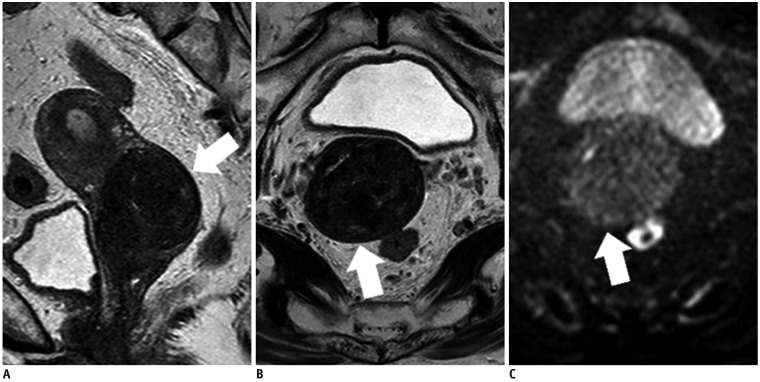
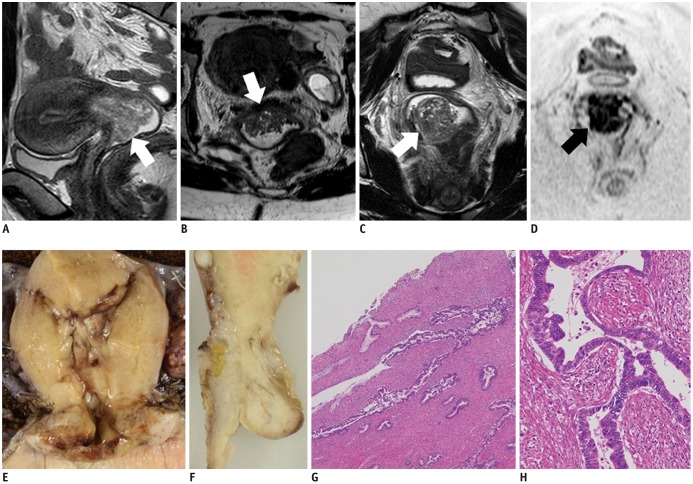 | Fig. 330-year-old woman with endocervical adenocarcinoma, usual type.
A. Sagittal T2WI shows exophytic tumor (arrow) in uterine cervix. Axial (B) and coronal (C) T2WIs show similar to fern leaf-like appearance, i.e., exophytic villous pattern (arrows) (Fig. 1; Type 2). D. Coronal DWI shows restricted diffusion (arrow). E, F. Fixed samples (E, coronal; F, sagittal) show diffuse enlargement of cervix, with invasive solid and diffuse infiltrative pattern, not exophytic villous pattern. G, H. On microscopic examination (G, hematoxylin-eosin staining, original magnification, × 40; H, hematoxylin-eosin staining, original magnification, × 200), tumor shows papillary surface, although it is composed of stromal hyperplasia caused by inflammation. Tumor cell glandules exist in inner part and show concave shape. Pseudostratification and necrotic debris within gland space are typical features of endocervical adenocarcinoma, usual type. Coexistence with CIN also indicates correlation with human papilloma virus infection. CIN = cervical intraepithelial neoplasia
|
Mucinous Carcinoma, Gastric Type (Figs. 4, 5)
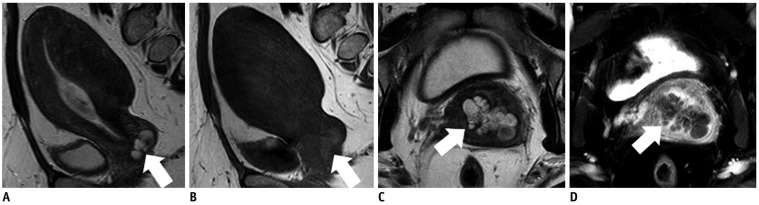
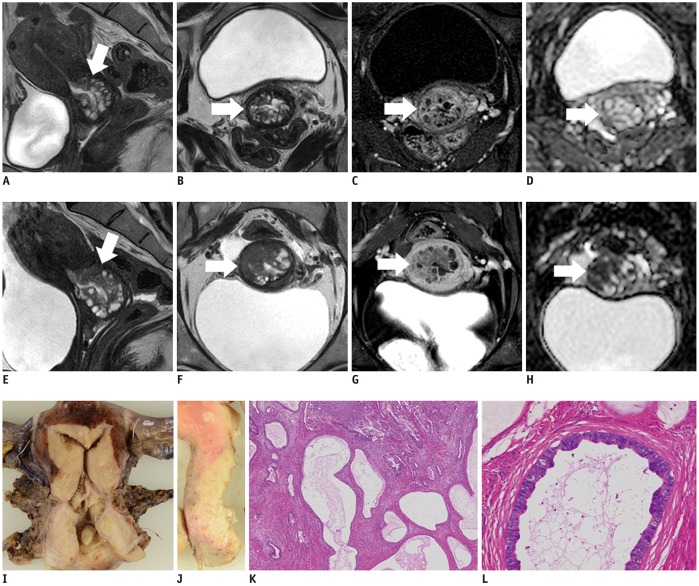 | Fig. 446-year-old woman with GAS (A–D: 1 year prior).
A, E. Sagittal T2WIs show multicystic mass with solid components (arrows) that increases in size. B, F. Axial T2WIs show solid components that have increased in size over year (arrows). Solid and cystic (Fig. 1; Type 1) as well as invasive solid patterns (Fig. 1; Type 4) are seen in this tumor. C, G. Axial contrast-enhanced fat-saturated T1WIs show mild enhancement of solid components (arrows). D, H. Restricted diffusion becomes clear on axial ADC map (arrows) over a year. I, J. Fixed samples (I, coronal; J, sagittal) show solid tumor with multiple cystic components. K. Microscopic examination (hematoxylin-eosin staining, original magnification, × 40) shows tumor cells diffusely infiltrating and involving glandules of LEGH lesion, while maintaining its glandular cavities. L. Microscopic examination (hematoxylin-eosin staining, original magnification, × 200) shows tumor cells with abundant clear cytoplasm. p16 negativity indicated lack of correlation with human papilloma virus infection (not displayed), which is characteristic of GAS. ADC = apparent diffusion coefficient, LEGH = lobular endocervical glandular hyperplasia
|
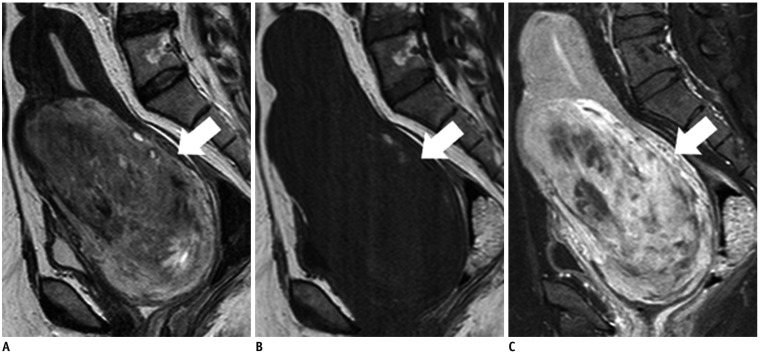
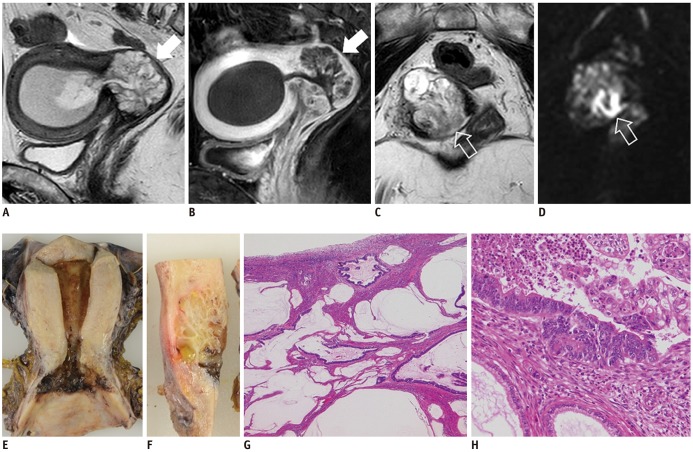 | Fig. 556-year-old woman with GAS.
A. Sagittal T2WI shows multicystic mass (arrow) in uterine cervix, consistent with Type 1 appearance (Fig. 1). B. Sagittal contrast-enhanced fat-saturated T1WI shows well enhanced septa in multicystic mass (arrow). C. Axial T2WI shows core-like hypointense lesion in center of multicystic mass (void arrow). D. Axial DWI shows restricted diffusion in solid core (void arrow), and solid component with restricted diffusion suggests GAS occurring in LEGH lesion. E, F. Fixed samples (E, coronal; F, sagittal) show multicystic tumor in uterine cervix. G, H. Microscopic examination (G, hematoxylin-eosin staining, original magnification, × 40; H, hematoxylin-eosin staining, original magnification, × 200) shows tumor composed of abundant mucinous lakes. Cluster of tumor cells exist in core, and tumor cells are widely spread to line mucinous lakes. p16 negativity indicated lack of correlation with human papilloma virus infection (not displayed).
|
Mucinous Carcinoma, Intestinal Type (Fig. 6)
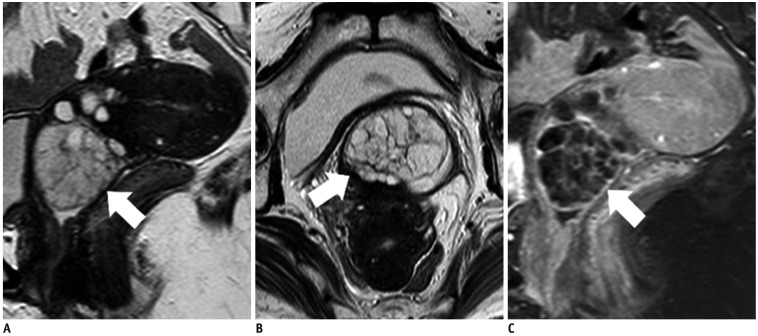
 | Fig. 657-year-old woman with mucinous carcinoma, intestinal type.Sagittal (A) and axial (B) T2WIs show high signal-intensity mass with invasive solid pattern (Fig. 1; Type 4) in uterine cervix (arrows). C. Tumor shows weak restricted diffusion on axial ADC map (arrow). Relatively high signal intensities on T2WI and weak restricted diffusion seem to reflecting intracellular mucinous components. D. Tumor is mildly enhanced on axial contrast-enhanced fat-saturated T1WI (arrow).
|
Villoglandular Carcinoma (Fig. 7)
 | Fig. 736-year-old woman with villoglandular carcinoma.Sagittal (A) and axial (B) T2WIs show cervical tumor with fern leaf-like appearance (exophytic villous pattern, Fig. 1; Type 2) (arrows). C. On axial DWI, tumor shows restricted diffusion (arrow), and malignancy is suggested. D. Fixed sample shows cervical tumor with fern leaf-like appearance. E, F. Microscopic examination (E, hematoxylin-eosin staining, original magnification, × 40; F, hematoxylin-eosin staining, original magnification, × 20) shows exophytic tumor with villous fronds lined by well-differentiated tumor cells. Coexistence with CIN also indicates correlation of this tumor with human papilloma virus infection.
|
Clear Cell Carcinoma (Fig. 8)
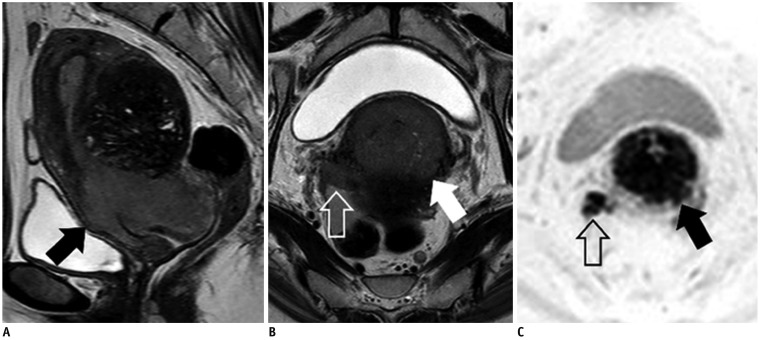 | Fig. 853-year-old woman with clear cell carcinoma.Sagittal (A) and axial (B) T2WIs show invasive solid tumor (Fig. 1; Type 4) in uterine cervix (arrows) with right parametrial invasion reaching pelvic wall (void arrow). C. On axial DWI, tumor (arrow) and parametrical invasion (void arrow) both show restricted diffusion. It is difficult to distinguish clear cell carcinoma from SCC and endocervical adenocarcinoma, usual type, by MRI alone.
|
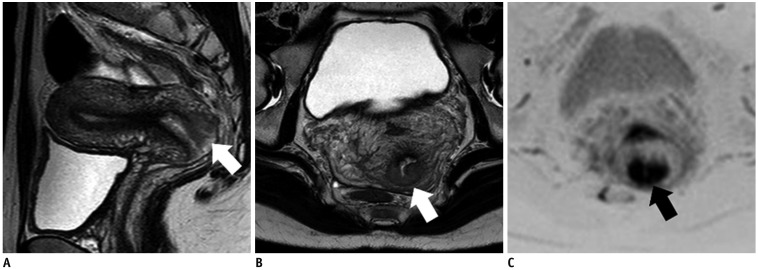
Endometrioid Carcinoma (Fig. 9)
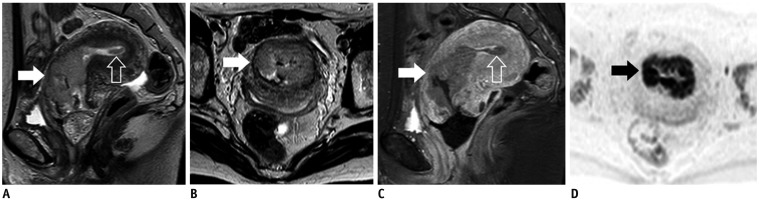 | Fig. 947-year-old woman with endometrioid carcinomaSagittal (A) and axial (B) T2WIs show invasive solid tumor (Fig. 1; Type 4) mainly located in cervical canal (arrows). Small tumor is also present in uterine corpus (void arrow). C. Sagittal contrast-enhanced fat-saturated T1WI shows mild enhancement of both tumors (arrow, void arrow). D. On axial DWI, tumor shows restricted diffusion (arrow). Pathological diagnosis was uterine corpus carcinoma, stage II, but final clinical diagnosis, which was based on main tumor location, was uterine cervical endometrioid carcinoma, stage IB2, with dissemination in uterine body cavity.
|
Other Cervical Tumors and Tumor-Like Lesions
Lobular Endocervical Glandular Hyperplasia (Fig. 10)
 | Fig. 1045-year-old woman with cosmos pattern LEGH (A, B) and 47-year-old woman with microcystic pattern LEGH (C).Sagittal (A) and axial (B) T2WIs show multicystic lesion in uterine cervix (arrows) with Type 1 appearance (Fig. 1). Microcytic parts surrounded by medium-sized to large cysts, indicating cosmos pattern. C. Sagittal T2WI shows multicystic lesion in uterine cervix (arrow) (Fig. 1; Type 1). Aggregation of small cysts without peripheral large cysts, indicating microcystic pattern.
|
Nabothian Cyst (Fig. 11)
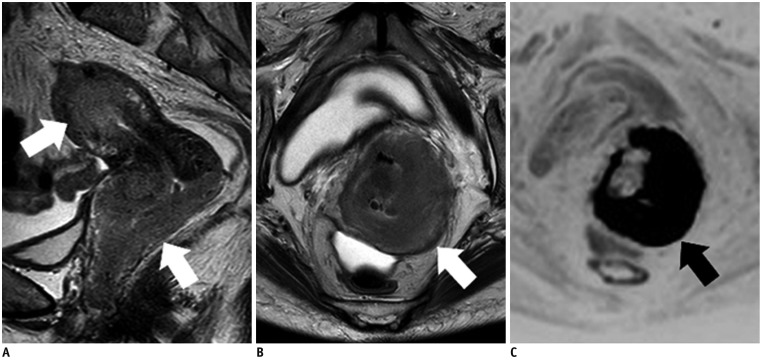
 | Fig. 1145-year-old woman with Nabothian cyst.
A. Sagittal T2WI shows multicystic lesion near surface of cervical lip (arrow). B. On axial T1WI, cysts show slightly high signal intensity (arrow). C. On axial T2WI, cysts show high to intermediate signal intensity (arrow). Intermediate signal intensities on T2WI and slightly high signal intensities on T1WI indicate mucus contents, and this is characteristic imaging finding of Nabothian cysts. D. There is no enhanced solid component in cysts (arrow) on axial contrast-enhanced fat-saturated T1WI.
|
Endocervical Polyp (Fig. 12)
 | Fig. 1253-year-old woman with cervical polyp.Sagittal (A) and axial (B) T2WIs show exophytic, oval, multicystic lesion protruding from cervix into vagina (arrows). C. Sagittal contrast-enhanced fat-saturated T1WI shows well-enhanced septa in multicystic lesion (arrow). Fibrovascular core is not clear; therefore, it is difficult to distinguish cervical polyp from LEGH in this case.
|
Adenosquamous Carcinoma (Fig. 13)
 | Fig. 1330-year-old woman with ASC.Sagittal (A) and axial (B) T2WIs show invasive solid tumor (Fig. 1; Type 4) located in posterior cervical lip (arrows). C. Axial DWI shows markedly restricted diffusion (arrow). It is difficult to distinguish ASC from SCC and endocervical adenocarcinoma, usual type.
|
Neuroendocrine Tumor (Fig. 14)
 | Fig. 1463-year-old woman with large cell neuroendocrine carcinoma.Sagittal (A) and axial (B) T2WIs show invasive solid tumor (Fig. 1; Type 4) in uterine cervix (arrows). C. Axial DWI shows markedly restricted diffusion (arrow). This lesion is also difficult to distinguish from SCC and endocervical adenocarcinoma, usual type.
|
Leiomyoma (Fig. 15)
 | Fig. 1570-year-old woman with leiomyoma.Sagittal (A) and axial (B) T2WIs show well-defined, homogeneous, hypointense mass (Fig. 1; Type 3) in stroma of uterine cervix (arrows). C. Axial DWI does not show restricted diffusion (arrow).
|
Leiomyosarcoma (Fig. 16)
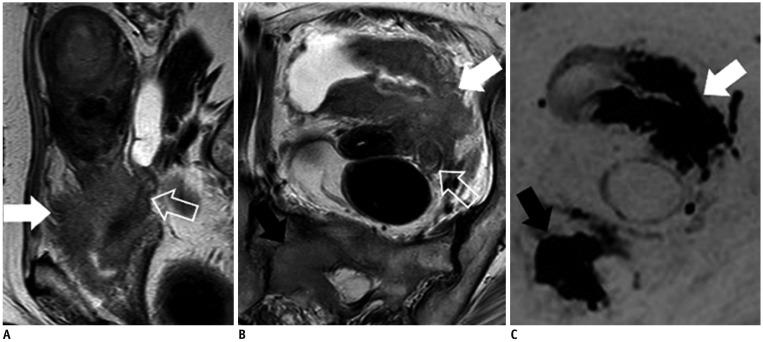
 | Fig. 1650-year-old woman with leiomyosarcoma.
A. Sagittal T2WI shows invasive solid tumor (Fig. 1; Type 4) in myometrium of uterine cervix (arrow), with relatively high signal intensity. B. Sagittal T1WI shows foci of high signal intensity in tumor (arrow), which are considered to be hemorrhagic foci. C. Heterogeneous enhancement is seen in tumor (arrow) on sagittal contrast-enhanced fat-saturated T1WI. Nonenhanced areas indicate tumor necrosis with hemorrhage.
|
Lymphoma (Fig. 17)
 | Fig. 1763-year-old woman with primary lymphoma of uterus, diffuse large B-cell type.Sagittal (A) and axial (B) T2WIs show infiltrating masses (Fig. 1; Type 5) located in cervix and corpus (arrows). C. Tumors show markedly restricted diffusion (arrow) on axial DWI, suggesting rich cellularity.
|
Secondary Tumors (Fig. 18)
 | Fig. 1880-year-old woman with urothelial carcinoma.Sagittal (A) and axial (B) T2WIs show diffuse infiltrating mass (Fig. 1; Type 5) involving bladder (white arrows), left ureter (void arrows), parametrium, and uterine cervix. Bladder is mainly replaced with mass and urothelial carcinoma is speculated by MRI. C. On DWI, main tumor (white arrow) and bone metastasis show restricted diffusion (black arrow). Biopsy specimen from bladder shows urothelial carcinoma, which pathologically suggests that uterine cervix is secondarily involved by bladder cancer.
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download