METHODS
Study Eligibility Criteria
Search Methods for Identification of Studies
Data Extraction
Methodological Quality Assessment
RESULTS
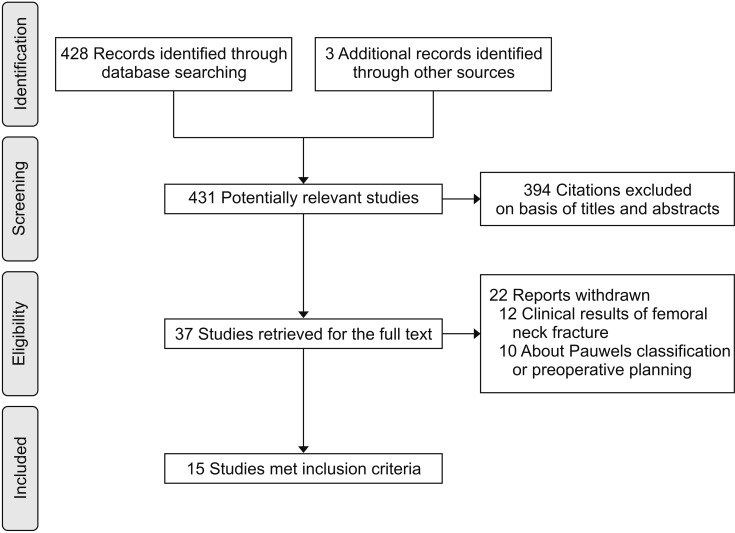
Search Results
Table 1
Number and Type of Subjects and Fixation Device of Included Studies
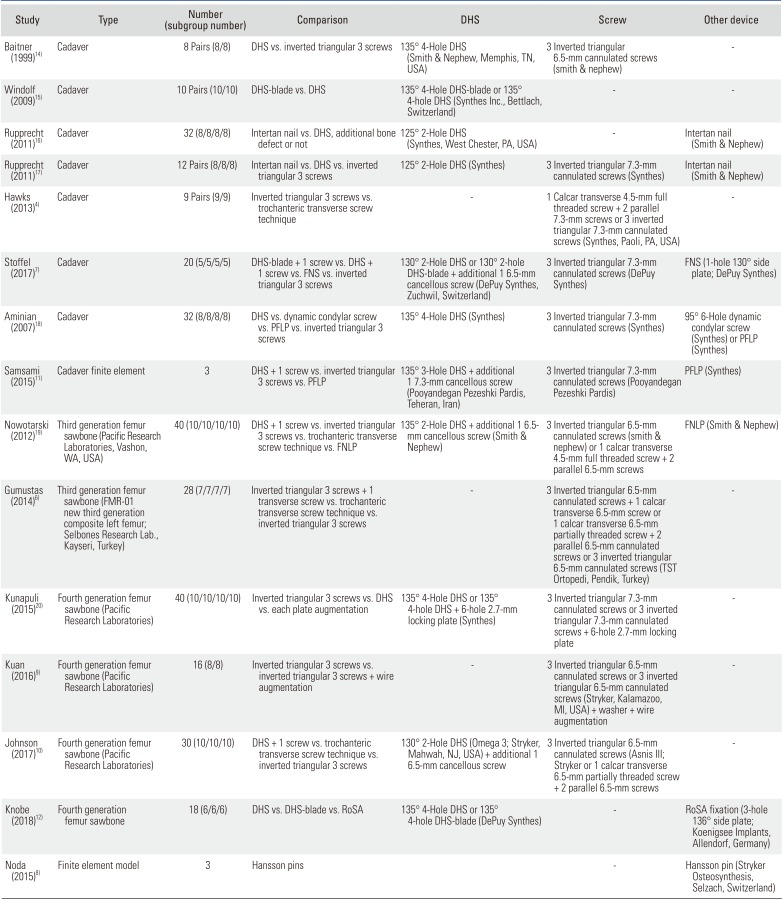
| Study | Type | Number (subgroup number) | Comparison | DHS | Screw | Other device |
|---|---|---|---|---|---|---|
| Baitner (1999)14) | Cadaver | 8 Pairs (8/8) | DHS vs. inverted triangular 3 screws | 135° 4-Hole DHS (Smith & Nephew, Memphis, TN, USA) | 3 Inverted triangular 6.5-mm cannulated screws (smith & nephew) | - |
| Windolf (2009)15) | Cadaver | 10 Pairs (10/10) | DHS-blade vs. DHS | 135° 4-Hole DHS-blade or 135° 4-hole DHS (Synthes Inc., Bettlach, Switzerland) | - | - |
| Rupprecht (2011)16) | Cadaver | 32 (8/8/8/8) | Intertan nail vs. DHS, additional bone defect or not | 125° 2-Hole DHS (Synthes, West Chester, PA, USA) | - | Intertan nail (Smith & Nephew) |
| Rupprecht (2011)17) | Cadaver | 12 Pairs (8/8/8) | Intertan nail vs. DHS vs. inverted triangular 3 screws | 125° 2-Hole DHS (Synthes) | 3 Inverted triangular 7.3-mm cannulated screws (Synthes) | Intertan nail (Smith & Nephew) |
| Hawks (2013)4) | Cadaver | 9 Pairs (9/9) | Inverted triangular 3 screws vs. trochanteric transverse screw technique | - | 1 Calcar transverse 4.5-mm full threaded screw + 2 parallel 7.3-mm screws or 3 inverted triangular 7.3-mm cannulated screws (Synthes, Paoli, PA, USA) | - |
| Stoffel (2017)7) | Cadaver | 20 (5/5/5/5) | DHS-blade + 1 screw vs. DHS + 1 screw vs. FNS vs. inverted triangular 3 screws | 130° 2-Hole DHS or 130° 2-hole DHS-blade + additional 1 6.5-mm cancellous screw (DePuy Synthes, Zuchwil, Switzerland) | 3 Inverted triangular 7.3-mm cannulated screws (DePuy Synthes) | FNS (1-hole 130° side plate; DePuy Synthes) |
| Aminian (2007)18) | Cadaver | (8/8/8/8) | DHS vs. dynamic condylar screw vs. PFLP vs. inverted triangular 3 screws | 135° 4-Hole DHS (Synthes) | 3 Inverted triangular 7.3-mm cannulated screws (Synthes) | 95° 6-Hole dynamic condylar screw (Synthes) or PFLP (Synthes) |
| Samsami (2015)11) | Cadaver finite element | 3 | DHS + 1 screw vs. inverted triangular 3 screws vs. PFLP | 135° 3-Hole DHS + additional 1 7.3-mm cancellous screw (Pooyandegan Pezeshki Pardis, Teheran, Iran) | 3 Inverted triangular 7.3-mm cannulated screws (Pooyandegan Pezeshki Pardis) | PFLP (Synthes) |
| Nowotarski (2012)19) | Third generation femur sawbone (Pacific Research Laboratories, Vashon, WA, USA) | 40 (10/10/10/10) | DHS + 1 screw vs. inverted triangular 3 screws vs. trochanteric transverse screw technique vs. FNLP | 135° 2-Hole DHS + additional 1 6.5- mm cancellous screw (Smith & Nephew) | 3 Inverted triangular 6.5-mm cannulated screws (smith & nephew) or 1 calcar transverse 4.5-mm full threaded screw + 2 parallel 6.5-mm screws | FNLP (Smith & Nephew) |
| Gumustas (2014)6) | Third generation femur sawbone (FMR-01 new third generation composite left femur; Selbones Research Lab., Kayseri, Turkey) | 28 (7/7/7/7) | Inverted triangular 3 screws + 1 transverse screw vs. trochanteric transverse screw technique vs. inverted triangular 3 screws | - | 3 Inverted triangular 6.5-mm cannulated screws + 1 calcar transverse 6.5-mm screw or 1 calcar transverse 6.5-mm partially threaded screw + 2 parallel 6.5-mm cannulated screws or 3 inverted triangular 6.5-mm cannulated screws (TST Ortopedi, Pendik, Turkey) | - |
| Kunapuli (2015)20) | Fourth generation femur sawbone (Pacific Research Laboratories) | 40 (10/10/10/10) | Inverted triangular 3 screws vs. DHS vs. each plate augmentation | 135° 4-Hole DHS or 135° 4-hole DHS + 6-hole 2.7-mm locking plate (Synthes) | 3 Inverted triangular 7.3-mm cannulated screws or 3 inverted triangular 7.3-mm cannulated screws + 6-hole 2.7-mm locking plate | - |
| Kuan (2016)9) | Fourth generation femur sawbone (Pacific Research Laboratories) | 16 (8/8) | Inverted triangular 3 screws vs. inverted triangular 3 screws + wire augmentation | - | 3 Inverted triangular 6.5-mm cannulated screws or 3 inverted triangular 6.5-mm cannulated screws (Stryker, Kalamazoo, MI, USA) + washer + wire augmentation | - |
| Johnson (2017)10) | Fourth generation femur sawbone (Pacific Research Laboratories) | 30 (10/10/10) | DHS + 1 screw vs. trochanteric transverse screw technique vs. inverted triangular 3 screws | 130° 2-Hole DHS (Omega 3; Stryker, Mahwah, NJ, USA) + additional 1 6.5-mm cancellous screw | 3 Inverted triangular 6.5-mm cannulated screws (Asnis III; Stryker or 1 calcar transverse 6.5-mm partially threaded screw + 2 parallel 6.5-mm screws | - |
| Knobe (2018)12) | Fourth generation femur sawbone | 18 (6/6/6) | DHS vs. DHS-blade vs. RoSA | 135° 4-Hole DHS or 135° 4-hole DHS-blade (DePuy Synthes) | - | RoSA fixation (3-hole 136° side plate; Koenigsee Implants, Allendorf, Germany) |
| Noda (2015)8) | Finite element model | 3 | Hansson pins | - | Hansson pin (Stryker Osteosynthesis, Selzach, Switzerland) |
Table 2
Experimental Setting of Included Studies
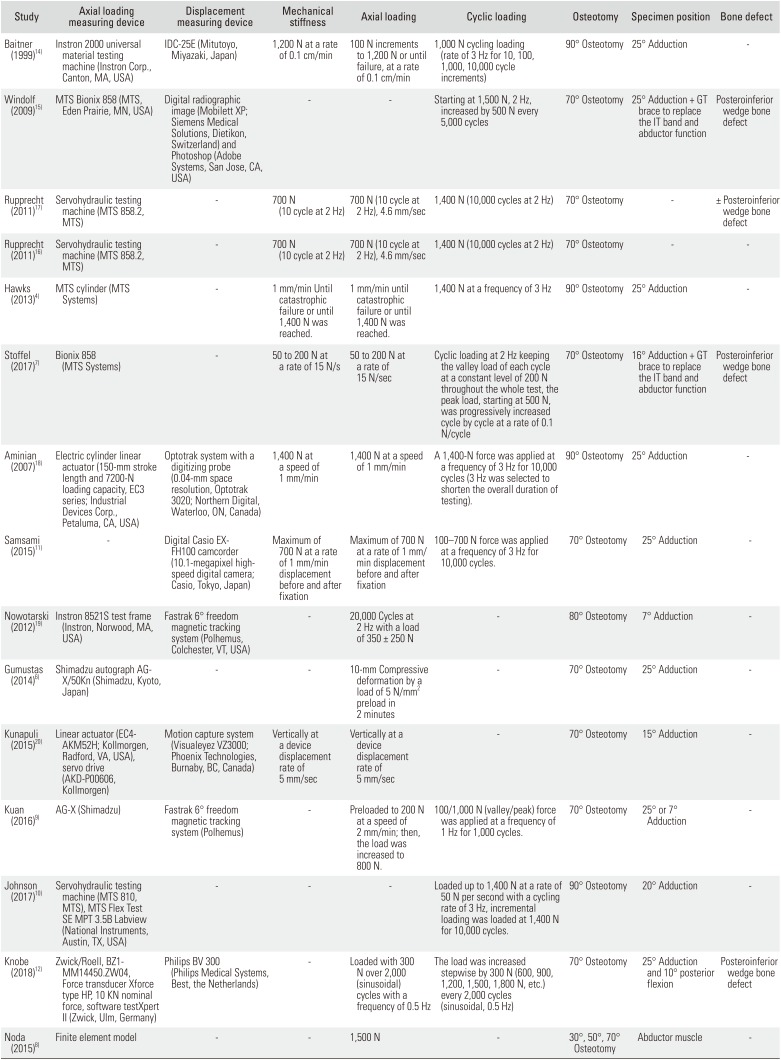
| Study | Axial loading measuring device | Displacement measuring device | Mechanical stiffness | Axial loading | Cyclic loading | Osteotomy | Specimen position | Bone defect |
|---|---|---|---|---|---|---|---|---|
| Baitner (1999)14) | Instron 2000 universal material testing machine (Instron Corp., Canton, MA, USA) | IDC-25E (Mitutoyo, Miyazaki, Japan) | 1,200 N at a rate of 0.1 cm/min | 100 N increments to 1,200 N or until failure, at a rate of 0.1 cm/min | 1,000 N cycling loading (rate of 3 Hz for 10, 100, 1,000, 10,000 cycle increments) | 90° Osteotomy | 25° Adduction | - |
| Windolf (2009)15) | MTS Bionix 858 (MTS, Eden Prairie, MN, USA) | Digital radiographic image (Mobilett XP; Siemens Medical Solutions, Dietikon, Switzerland) and Photoshop (Adobe Systems, San Jose, CA, USA) | - | - | Starting at 1,500 N, 2 Hz, increased by 500 N every 5,000 cycles | 70° Osteotomy | 25° Adduction + GT brace to replace the IT band and abductor function | Posteroinferior wedge bone defect |
| Rupprecht (2011)17) | Servohydraulic testing machine (MTS 858.2, MTS) | - | 700 N (10 cycle at 2 Hz) | 700 N (10 cycle at 2 Hz), 4.6 mm/sec | 1,400 N (10,000 cycles at 2 Hz) | 70° Osteotomy | - | ± Posteroinferior wedge bone defect |
| Rupprecht (2011)16) | Servohydraulic testing machine (MTS 858.2, MTS) | - | 700 N (10 cycle at 2 Hz) | 700 N (10 cycle at 2 Hz), 4.6 mm/sec | 1,400 N (10,000 cycles at 2 Hz) | 70° Osteotomy | - | - |
| Hawks (2013)4) | MTS cylinder (MTS Systems) | - | 1 mm/min Until catastrophic failure or until 1,400 N was reached. | 1 mm/min until catastrophic failure or until 1,400 N was reached. | 1,400 N at a frequency of 3 Hz | 90° Osteotomy | 25° Adduction | - |
| Stoffel (2017)7) | Bionix 858 (MTS Systems) | - | 50 to 200 N at a rate of 15 N/s | 50 to 200 N at a rate of 15 N/sec | Cyclic loading at 2 Hz keeping the valley load of each cycle at a constant level of 200 N throughout the whole test, the peak load, starting at 500 N, was progressively increased cycle by cycle at a rate of 0.1 N/cycle | 70° Osteotomy | 16° Adduction + GT brace to replace the IT band and abductor function | Posteroinferior wedge bone defect |
| Aminian (2007)18) | Electric cylinder linear actuator (150-mm stroke length and 7200-N loading capacity, EC3 series; Industrial Devices Corp., Petaluma, CA, USA) | Optotrak system with a digitizing probe (0.04-mm space resolution, Optotrak 3020; Northern Digital, Waterloo, ON, Canada) | 1,400 N at a speed of 1 mm/min | 1,400 N at a speed of 1 mm/min | A 1,400-N force was applied at a frequency of 3 Hz for 10,000 cycles (3 Hz was selected to shorten the overall duration of testing). | 90° Osteotomy | 25° Adduction | - |
| Samsami (2015)11) | - | Digital Casio EXFH100 camcorder (10.1-megapixel highspeed digital camera; Casio, Tokyo, Japan) | Maximum of 700 N at a rate of 1 mm/min displacement before and after fixation | Maximum of 700 N at a rate of 1 mm/ min displacement before and after fixation | 100–700 N force was applied at a frequency of 3 Hz for 10,000 cycles. | 70° Osteotomy | 25° Adduction | - |
| Nowotarski (2012)19) | Instron 8521S test frame (Instron, Norwood, MA, USA) | Fastrak 6° freedom magnetic tracking system (Polhemus, Colchester, VT, USA) | - | 20,000 Cycles at 2 Hz with a load of 350 ± 250 N | - | 80° Osteotomy | 7° Adduction | - |
| Gumustas (2014)6) | Shimadzu autograph AGX/50Kn (Shimadzu, Kyoto, Japan) | - | - | 10-mm Compressive deformation by a load of 5 N/mm2 preload in 2 minutes | - | 70° Osteotomy | 25° Adduction | - |
| Kunapuli (2015)20) | Linear actuator (EC4-AKM52H; Kollmorgen, Radford, VA, USA), servo drive (AKD-P00606, Kollmorgen) | Motion capture system (Visualeyez VZ3000; Phoenix Technologies, Burnaby, BC, Canada) | Vertically at a device displacement rate of 5 mm/sec | Vertically at a device displacement rate of 5 mm/sec | - | 70° Osteotomy | 15° Adduction | - |
| Kuan (2016)9) | AG-X (Shimadzu) | Fastrak 6° freedom magnetic tracking system (Polhemus) | - | Preloaded to 200 N at a speed of 2 mm/min; then, the load was increased to 800 N. | 100/1,000 N (valley/peak) force was applied at a frequency of 1 Hz for 1,000 cycles. | 70° Osteotomy | 25° or 7° Adduction | - |
| Johnson (2017)10) | Servohydraulic testing machine (MTS 810, MTS), MTS Flex Test SE MPT 3.5B Labview (National Instruments, Austin, TX, USA) | - | - | - | Loaded up to 1,400 N at a rate of 50 N per second with a cycling rate of 3 Hz, incremental loading was loaded at 1,400 N for 10,000 cycles. | 90° Osteotomy | 20° Adduction | - |
| Knobe (2018)12) | Zwick/Roell, BZ1-MM14450.ZW04, Force transducer Xforce type HP, 10 KN nominal force, software testXpert II (Zwick, Ulm, Germany) | Philips BV 300 (Philips Medical Systems, Best, the Netherlands) | - | Loaded with 300 N over 2,000 (sinusoidal) cycles with a frequency of 0.5 Hz | The load was increased stepwise by 300 N (600, 900, 1,200, 1,500, 1,800 N, etc.) every 2,000 cycles (sinusoidal, 0.5 Hz) | 70° Osteotomy 25° Adduction and 10° posterior flexion | Posteroinferior wedge bone defect | - |
| Noda (2015)8) | Finite element model | - | - | 1,500 N | - | 30°, 50°, 70° Osteotomy | Abductor muscle | - |
Load-to-Failure and Axial Stiffness Using Cadavers
Table 3
Stiffness, Axial Loading, and Cyclic Loading Results
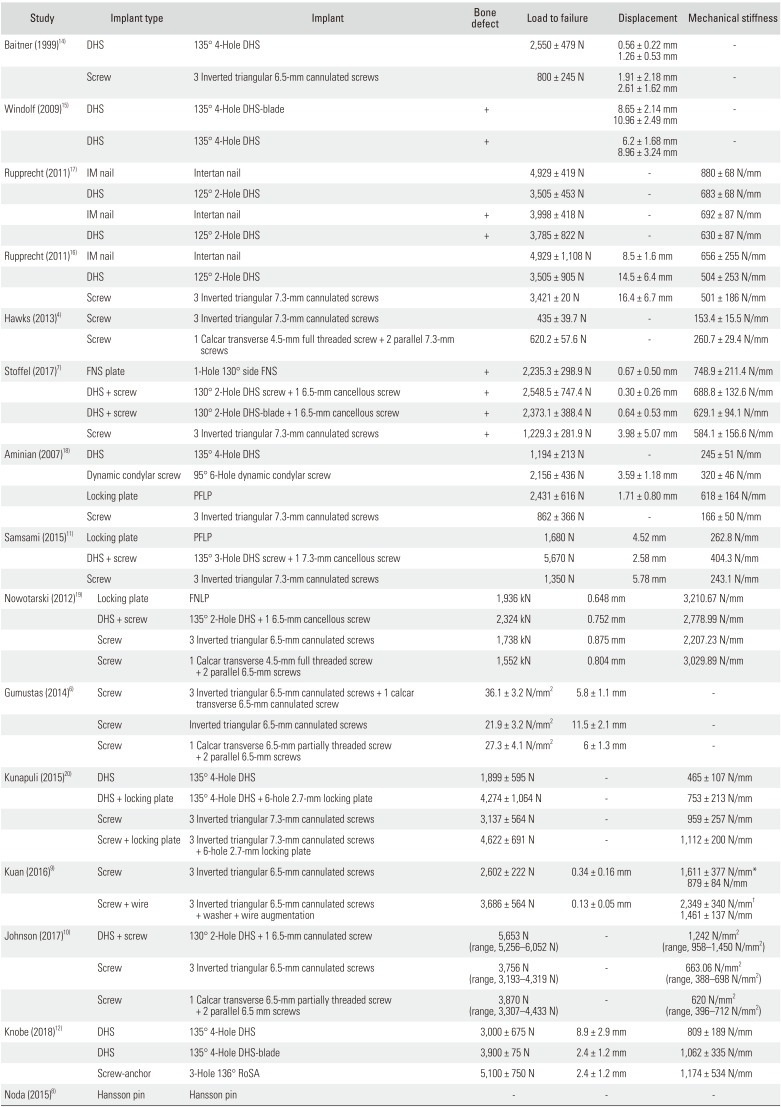
| Study | Implant type | Implant | Bone defect | Load to failure | Displacement | Mechanical stiffness |
|---|---|---|---|---|---|---|
| Baitner (1999)14) | DHS | 135° 4-Hole DHS | 2,550 ± 479 N | 0.56 ± 0.22 mm | - | |
| 1.26 ± 0.53 mm | ||||||
| Screw | 3 Inverted triangular 6.5-mm cannulated screws | 800 ± 245 N | 1.91 ± 2.18 mm | - | ||
| 2.61 ± 1.62 mm | ||||||
| Windolf (2009)15) | DHS | 135° 4-Hole DHS-blade | + | 8.65 ± 2.14 mm | - | |
| 10.96 ± 2.49 mm | ||||||
| DHS | 135° 4-Hole DHS | + | 6.2 ± 1.68 mm | - | ||
| 8.96 ± 3.24 mm | ||||||
| Rupprecht (2011)17) | IM nail | Intertan nail | 4,929 ± 419 N | - | 880 ± 68 N/mm | |
| DHS | 125° 2-Hole | DHS | 3,505 ± 453 N | - | 683 ± 68 N/mm | |
| IM nail | Intertan nail | + | 3,998 ± 418 N | - | 692 ± 87 N/mm | |
| DHS | 125° 2-Hole DHS | + | 3,785 ± 822 N | - | 630 ± 87 N/mm | |
| Rupprecht (2011)16) | IM nail | Intertan nail | 4,929 ± 1,108 N | 8.5 ± 1.6 mm | 656 ± 255 N/mm | |
| DHS | 125° 2-Hole DHS | 3,505 ± 905 N | 14.5 ± 6.4 mm | 504 ± 253 N/mm | ||
| Screw | 3 Inverted triangular 7.3-mm cannulated screws | 3,421 ± 20 N | 16.4 ± 6.7 mm | 501 ± 186 N/mm | ||
| Hawks (2013)4) | Screw | 3 Inverted triangular 7.3-mm cannulated screws | 435 ± 39.7 N | - | 153.4 ± 15.5 N/mm | |
| Screw | 1 Calcar transverse 4.5-mm full threaded screw + 2 parallel 7.3-mm screws | 620.2 ± 57.6 N | - | 260.7 ± 29.4 N/mm | ||
| Stoffel (2017)7) | FNS plate | 1-Hole 130° side FNS | + | 2,235.3 ± 298.9 N | 0.67 ± 0.50 mm | 748.9 ± 211.4 N/mm |
| DHS + screw 130° | 2-Hole DHS screw + 1 6.5-mm cancellous screw | + | 2,548.5 ± 747.4 N | 0.30 ± 0.26 mm | 688.8 ± 132.6 N/mm | |
| DHS + screw 130° | 2-Hole DHS-blade + 1 6.5-mm cancellous screw | + | 2,373.1 ± 388.4 N | 0.64 ± 0.53 mm | 629.1 ± 94.1 N/mm | |
| Screw | 3 Inverted triangular 7.3-mm cannulated screws | + | 1,229.3 ± 281.9 N | 3.98 ± 5.07 mm | 584.1 ± 156.6 N/mm | |
| Aminian (2007)18) | DHS | 135° 4-Hole DHS | 1,194 ± 213 N | - | 245 ± 51 N/mm | |
| Dynamic condylar screw | 95° 6-Hole dynamic condylar screw | 2,156 ± 436 N | 3.59 ± 1.18 mm | 320 ± 46 N/mm | ||
| Locking plate | PFLP | 2,431 ± 616 N | 1.71 ± 0.80 mm | 618 ± 164 N/mm | ||
| Screw | 3 Inverted triangular 7.3-mm cannulated screws | 862 ± 366 N | - | 166 ± 50 N/mm | ||
| Samsami (2015)11) | Locking plate | PFLP | 1,680 N | 4.52 mm | 262.8 N/mm | |
| DHS + screw | 135° 3-Hole DHS screw + 1 7.3-mm cancellous screw | 5,670 N | 2.58 mm | 404.3 N/mm | ||
| Screw | 3 Inverted triangular 7.3-mm cannulated screws | 1,350 N | 5.78 mm | 243.1 N/mm | ||
| Nowotarski (2012)19) | Locking plate | FNLP | 1,936 kN | 0.648 mm | 3,210.67 N/mm | |
| DHS + screw | 135° 2-Hole DHS + 1 6.5-mm cancellous screw | 2,324 kN | 0.752 mm | 2,778.99 N/mm | ||
| Screw | 3 Inverted triangular 6.5-mm cannulated screws | 1,738 kN | 0.875 mm | 2,207.23 N/mm | ||
| Screw | 1 Calcar transverse 4.5-mm full threaded screw + 2 parallel 6.5-mm screws | 1,552 kN | 0.804 mm | 3,029.89 N/mm | ||
| Gumustas (2014)6) | Screw | 3 Inverted triangular 6.5-mm cannulated screws + 1 calcar transverse 6.5-mm cannulated screw | 36.1 ± 3.2 N/mm2 | 5.8 ± 1.1 mm | - | |
| Screw | Inverted triangular 6.5-mm cannulated screws | 21.9 ± 3.2 N/mm2 | 11.5 ± 2.1 mm | - | ||
| Screw | 1 Calcar transverse 6.5-mm partially threaded screw + 2 parallel 6.5-mm screws | 27.3 ± 4.1 N/mm2 | 6 ± 1.3 mm | - | ||
| Kunapuli (2015)20) | DHS | 135° 4-Hole DHS | 1,899 ± 595 N | - | 465 ± 107 N/mm | |
| DHS + locking plate | 135° 4-Hole DHS + 6-hole 2.7-mm locking plate | 4,274 ± 1,064 N | - | 753 ± 213 N/mm | ||
| Screw | 3 Inverted triangular 7.3-mm cannulated screws | 3,137 ± 564 N | - | 959 ± 257 N/mm | ||
| Screw + locking plate | 3 Inverted triangular 7.3-mm cannulated screws + 6-hole 2.7-mm locking plate | 4,622 ± 691 N | - | 1,112 ± 200 N/mm | ||
| Kuan (2016)9) | Screw | 3 Inverted triangular 6.5-mm cannulated screws | 2,602 ± 222 N | 0.34 ± 0.16 mm | 1,611 ± 377 N/mm* | |
| 879 ± 84 N/mm | ||||||
| Screw + wire | 3 Inverted triangular 6.5-mm cannulated screws + washer + wire augmentation | 3,686 ± 564 N | 0.13 ± 0.05 mm | 2,349 ± 340 N/mm† | ||
| 1,461 ± 137 N/mm | ||||||
| Johnson (2017)10) | DHS + screw | 130° 2-Hole DHS + 1 6.5-mm cannulated screw | 5,653 N (range, 5,256–6,052 N) | - | 1,242 N/mm2 (range, 958–1,450 N/mm2) | |
| Screw | 3 Inverted triangular 6.5-mm cannulated screws | 3,756 N (range, 3,193–4,319 N) | - | 663.06 N/mm2 (range, 388–698 N/mm2) | ||
| Screw | 1 Calcar transverse 6.5-mm partially threaded screw + 2 parallel 6.5 mm screws | 3,870 N (range, 3,307–4,433 N) | - | 620 N/mm2 (range, 396–712 N/mm2) | ||
| Knobe (2018)12) | DHS | 135° 4-Hole DHS | 3,000 ± 675 N | 8.9 ± 2.9 mm | 809 ± 189 N/mm | |
| DHS | 135° 4-Hole DHS-blade | 3,900 ± 75 N | 2.4 ± 1.2 mm | 1,062 ± 335 N/mm | ||
| Screw-anchor | 3-Hole 136° RoSA | 5,100 ± 750 N | 2.4 ± 1.2 mm | 1,174 ± 534 N/mm | ||
| Noda (2015)8) | Hansson pin | Hansson pin | - | - | - |
Load-to-Failure and Axial Stiffness Using Sawbones
Displacement
Risk of Bias
Table 4
Quality Assessment of the Included Studies by the Newcastle-Ottawa Scale
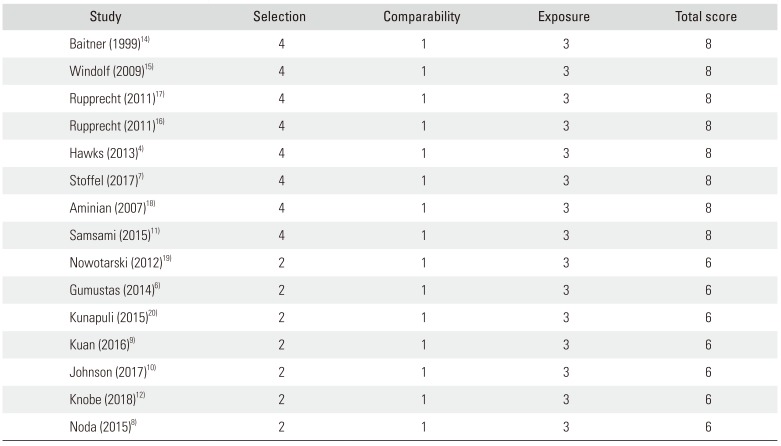
| Study | Selection | Comparability | Exposure | Total score |
|---|---|---|---|---|
| Baitner (1999)14) | 4 | 1 | 3 | 8 |
| Windolf (2009)15) | 4 | 1 | 3 | 8 |
| Rupprecht (2011)17) | 4 | 1 | 3 | 8 |
| Rupprecht (2011)16) | 4 | 1 | 3 | 8 |
| Hawks (2013)4) | 4 | 1 | 3 | 8 |
| Stoffel (2017)7) | 4 | 1 | 3 | 8 |
| Aminian (2007)18) | 4 | 1 | 3 | 8 |
| Samsami (2015)11) | 4 | 1 | 3 | 8 |
| Nowotarski (2012)19) | 2 | 1 | 3 | 6 |
| Gumustas (2014)6) | 2 | 1 | 3 | 6 |
| Kunapuli (2015)20) | 2 | 1 | 3 | 6 |
| Kuan (2016)9) | 2 | 1 | 3 | 6 |
| Johnson (2017)10) | 2 | 1 | 3 | 6 |
| Knobe (2018)12) | 2 | 1 | 3 | 6 |
| Noda (2015)8) | 2 | 1 | 3 | 6 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download