1. Brady RO, Gal AE, Bradley RM, Martensson E, Warshaw AL, Laster L. Enzymatic defect in Fabry's disease. Ceramidetrihexosidase deficiency. N Engl J Med. 1967; 276(21):1163–1167.

2. Desnick RJ, Blieden LC, Sharp HL, Hofschire PJ, Moller JH. Cardiac valvular anomalies in Fabry disease. Clinical, morphologic, and biochemical studies. Circulation. 1976; 54(5):818–825.


3. Desnick RJ, Ioannou YA, Eng CM. α-Galactosidase A deficiency: Fabry disease. The Metabolic and Molecular Bases of Inherited Disease. 8th ed. New York, NY: McGraw-Hill;2001. p. 3733–3774.
4. McNary WF, Lowenstein LM. A morphological study of the renal lesion in angiokeratoma corporis diffusum universale (Fabry's disease). J Urol. 1965; 93(6):641–648.


5. Pabico RC, Atancio BC, McKenna BA, Pamukcoglu T, Yodaiken R. Renal pathologic lesions and functional alterations in a man with Fabry's disease. Am J Med. 1973; 55(3):415–425.


6. Eng CM, Guffon N, Wilcox WR, Germain DP, Lee P, Waldek S, et al. Safety and efficacy of recombinant human alpha-galactosidase A replacement therapy in Fabry's disease. N Engl J Med. 2001; 345(1):9–16.

7. Weidemann F, Niemann M, Breunig F, Herrmann S, Beer M, Störk S, et al. Long-term effects of enzyme replacement therapy on Fabry cardiomyopathy: evidence for a better outcome with early treatment. Circulation. 2009; 119(4):524–529.

8. Meikle PJ, Hopwood JJ, Clague AE, Carey WF. Prevalence of lysosomal storage disorders. JAMA. 1999; 281(3):249–254.


10. Shelley ED, Shelley WB, Kurczynski TW. Painful fingers, heat intolerance, and telangiectases of the ear: easily ignored childhood signs of Fabry disease. Pediatr Dermatol. 1995; 12(3):215–219.


11. Hagège AA, Caudron E, Damy T, Roudaut R, Millaire A, Etchecopar-Chevreuil C, et al. Screening patients with hypertrophic cardiomyopathy for Fabry disease using a filter-paper test: the FOCUS study. Heart. 2011; 97(2):131–136.


12. DeMaria AN, Blanchard DG. The echocardiogram. Hurst's the Heart: Arteries and Veins. 10th ed. New York, NY: McGraw-Hill;2001. p. 343–460.
13. Herman MV, Gorlin R. Implications of left ventricular asynergy. Am J Cardiol. 1969; 23(4):538–547.


14. Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol. 1995; 26(2):135–136.

15. Nakao S, Takenaka T, Maeda M, Kodama C, Tanaka A, Tahara M, et al. An atypical variant of Fabry's disease in men with left ventricular hypertrophy. N Engl J Med. 1995; 333(5):288–293.


16. Blanch LC, Meaney C, Morris CP. A sensitive mutation screening strategy for Fabry disease: detection of nine mutations in the alpha-galactosidase A gene. Hum Mutat. 1996; 8(1):38–43.

17. Yousef Z, Elliott PM, Cecchi F, Escoubet B, Linhart A, Monserrat L, et al. Left ventricular hypertrophy in Fabry disease: a practical approach to diagnosis. Eur Heart J. 2013; 34(11):802–808.


18. Sachdev B, Takenaka T, Teraguchi H, Tei C, Lee P, McKenna WJ, et al. Prevalence of Anderson-Fabry disease in male patients with late onset hypertrophic cardiomyopathy. Circulation. 2002; 105(12):1407–1411.


20. Chimenti C, Pieroni M, Morgante E, Antuzzi D, Russo A, Russo MA, et al. Prevalence of Fabry disease in female patients with late-onset hypertrophic cardiomyopathy. Circulation. 2004; 110(9):1047–1053.


21. Arad M, Maron BJ, Gorham JM, Johnson WH Jr, Saul JP, Perez-Atayde AR, et al. Glycogen storage diseases presenting as hypertrophic cardiomyopathy. N Engl J Med. 2005; 352(4):362–372.


22. Morita H, Larson MG, Barr SC, Vasan RS, O'Donnell CJ, Hirschhorn JN, et al. Single-gene mutations and increased left ventricular wall thickness in the community: the Framingham Heart Study. Circulation. 2006; 113(23):2697–2705.

23. Monserrat L, Gimeno-Blanes JR, Marín F, Hermida-Prieto M, García-Honrubia A, Pérez I, et al. Prevalence of Fabry disease in a cohort of 508 unrelated patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2007; 50(25):2399–2403.


24. Havndrup O, Christiansen M, Stoevring B, Jensen M, Hoffman-Bang J, Andersen PS, et al. Fabry disease mimicking hypertrophic cardiomyopathy: genetic screening needed for establishing the diagnosis in women. Eur J Heart Fail. 2010; 12(6):535–540.


25. Elliott P, Baker R, Pasquale F, Quarta G, Ebrahim H, Mehta AB, et al. Prevalence of Anderson-Fabry disease in patients with hypertrophic cardiomyopathy: the European Anderson-Fabry Disease survey. Heart. 2011; 97(23):1957–1960.


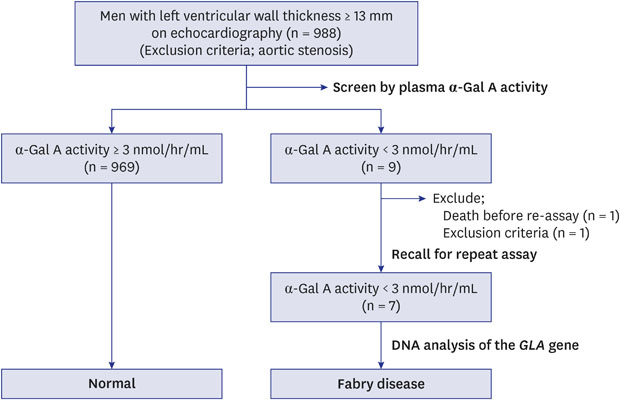
26. Mawatari K, Yasukawa H, Oba T, Nagata T, Togawa T, Tsukimura T, et al. Screening for Fabry disease in patients with left ventricular hypertrophy. Int J Cardiol. 2013; 167(3):1059–1061.


27. Terryn W, Deschoenmakere G, De Keyser J, Meersseman W, Van Biesen W, Wuyts B, et al. Prevalence of Fabry disease in a predominantly hypertensive population with left ventricular hypertrophy. Int J Cardiol. 2013; 167(6):2555–2560.


28. Palecek T, Honzikova J, Poupetova H, Vlaskova H, Kuchynka P, Golan L, et al. Prevalence of Fabry disease in male patients with unexplained left ventricular hypertrophy in primary cardiology practice: prospective Fabry cardiomyopathy screening study (FACSS). J Inherit Metab Dis. 2014; 37(3):455–460.


29. Herrera J, Miranda CS. Prevalence of Fabry's disease within hemodialysis patients in Spain. Clin Nephrol. 2014; 81(2):112–120.


30. Yasuda M, Shabbeer J, Benson SD, Maire I, Burnett RM, Desnick RJ. Fabry disease: characterization of α-galactosidase A double mutations and the D313Y plasma enzyme pseudodeficiency allele. Hum Mutat. 2003; 22(6):486–492.


31. Togawa T, Tsukimura T, Kodama T, Tanaka T, Kawashima I, Saito S, et al. Fabry disease: biochemical, pathological and structural studies of the α-galactosidase A with E66Q amino acid substitution. Mol Genet Metab. 2012; 105(4):615–620.









 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download