Abstract
Purpose
To evaluate the changes of axial length (AXL) in eyes with unilateral idiopathic central serous chorioretinopathy (CSC) after resolution of serous retinal detachment.
Methods
A total of 31 patients diagnosed with idiopathic unilateral CSC were included in this study. The changes of AXL according to serous retinal detachment were examined. The keratometric value and AXL were measured using partial coherence interferometry. Serous retinal detachment and central macular thickness (CMT) were measured by spectral domain optical coherence tomography.
Results
The mean age of the 31 CSC patients, including 19 males, was 42.7 years. The AXL was significantly increased from 23.41 to 23.58 mm after resolution of serous retinal detachment (p < 0.001). The CMT was significantly decreased from 413.4 to 226.8 µm after resolution of serous retinal detachment (p < 0.001). The differences in AXL correlated with CMT differences and subretinal fluid height (r = −0.616, p < 0.001 and r = −0.637, p < 0.001, respectively), and the best-corrected visual acuity was significantly different after resolution of serous retinal detachment (p < 0.001).
Cataract surgery is a very common procedure in elderly patients, and the final refractive outcome is the major determining factor for patient satisfaction following the procedure. To maximize visual acuity, a precise intraocular lens (IOL) power calculation must be performed; in particular, axial length (AXL) measurements are essential for determining the accuracy of IOL power calculations. Because cataract is frequently accompanied by retinal diseases in the elderly, macular abnormalities are common in patients undergoing cataract surgery. Hirnschall et al. reported that the prevalence of macular abnormalities determined by swept-source optical coherence tomography biometry was approximately 54% among patients who were scheduled to undergo cataract surgery [1]. Moreover, previous studies reported that macular abnormalities affected AXL measurement [23].
The AXL is usually measured using contact ultrasound biometry and partial optical coherence interferometry (PCI) techniques. Previous studies have reported that, because ultrasound determines the AXL between the corneal vertex and internal limiting membrane, patients with a thickened macula have shorter AXL measurements [456]. In contrast, PCI measures the AXL between the corneal vertex and retinal pigment epithelium (RPE), so the AXL measurement is less likely to be affected by macular thickness [789].
Central serous chorioretinopathy (CSC) is a disorder characterized by serous detachment of the neurosensory retina and/or RPE detachment at the posterior pole. CSC typically affects young to middle-aged males, with mild to moderate visual loss. In most cases, CSC spontaneously resolves within several months, without sequelae [101112].
To the best of our knowledge, there have been no prospective studies that have examined the effect of serous retinal detachment on AXL measurements. Therefore, we used PCI and spectral-domain optical coherence tomography (SD-OCT) to compare the AXL of idiopathic CSC eyes with serous retinal detachment with those showing serous retinal detachment resolution.
The protocol was approved by the institutional review board of Chungnam National University Hospital (2013-11-008). All patients signed an informed consent form, and the study adhered to the tenets of the Declaration of Helsinki.
We prospectively reviewed the medical records of patients with idiopathic CSC who were diagnosed at Chungnam National University Hospital between January 2014 and January 2016. Idiopathic CSC was diagnosed as the presence of a serous retinal detachment involving the macula, confirmed by SD-OCT, with one or a few leaks seen in the RPE using fluorescein angiography. We included patients with unilateral involvement at the time of diagnosis and after resolution of serous retinal detachment was confirmed using OCT and who were analyzed with both partial coherence interferometry and SD-OCT. Exclusion criteria were 1) systemic steroid use; 2) older than 55 years of age; 3) any vitreoretinal disease such as age-related macular degeneration, diabetic retinopathy, or retinal vascular occlusion; 4) OCT signal strength < 7; and 5) lack of a PCI measurement due to media opacity.
Both eyes were examined using autorefraction, intraocular pressure using a non-contact tonometer, best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, and a dilated fundus examination. Medical record information comprised age, sex, laterality, and duration of subjective symptoms.
All IOL Master (Carl Zeiss, Jena, Germany) and Cirrus OCT (Carl Zeiss Meditec, Dublin, CA, USA) examinations were performed by the same experienced examiner. During AXL measurements, all patients were asked to stare at the system's fixation target. The mean value of at least 10 valid measurements was defined as the AXL. Numeric values were automatically calculated by IOL Master software. According to the manufacturer's recommendations, valid measurements should have a signal-to-noise ratio >2.0 and acceptable waveform graphs. Keratometric value, AXL, and anterior chamber depth (ACD) were measured using PCI.
The macular cube 512 × 128 combination scan mode of the Cirrus HD-OCT was used for this study. This mode had 6 × 6 mm macular areas scanned into 512 × 128 dots to measure the thickness. The 6 × 6 mm circle belonged to the Early Treatment of Diabetic Retinopathy Study subfield and was divided into three concentric circles with diameters of 1, 3, and 6 mm as the central, inner, and outer circles, respectively; all of these circles were again split into four sides (superior, inferior, nasal, and temporal). We analyzed the central macular thickness (CMT). The presence of serous retinal detachment and CMT was measured using SD-OCT (Fig. 1). Subretinal fluid (SRF) height was measured manually between the outer segment of the photoreceptor layer and the apical face of the RPE layer.
Statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Comparisons of ocular biometrics before and after resolution of serous retinal detachment were analyzed using Student's paired t-test. Correlation and linear regression analyses were used to define clinical variables associated with AXL differences. A value of p < 0.05 was considered statistically significant.
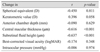
This study included 31 patients (19 males and 12 females) who were diagnosed with unilateral idiopathic CSC. The mean patient age was 42.7 ± 9.0 years. Both eyes were phakic in all patients without cataract. There were 12 affected right eyes and 19 affected left eyes. The mean time from onset of subjective symptoms to the initial visit was 3.4 ± 2.5 weeks. The mean value of SRF height was 185.8 ± 94.5 µm in the acute phase (Table 1).
The AXL significantly increased from 23.41 to 23.58 mm after resolution of serous retinal detachment (p < 0.001). CMT significantly decreased from 413.4 to 226.8 µm after resolution of serous retinal detachment (p < 0.001). The BCVA was significantly different after resolution of serous retinal detachment (0.20 ± 0.24 vs. 0.05 ± 0.18, p < 0.001), while the spherical equivalent, keratometric value, and ACD did not significantly change (−0.13 ± 1.33 vs. −0.17 ± 1.29 diopters [D], 43.95 ± 1.59 vs. 44.01 ± 1.58 D, and 3.36 ± 0.50 vs. 3.40 ± 0.48 D, respectively; p = 0.478, p = 0.174, and p = 0.070, respectively) (Table 2). Table 3 shows the correlations of clinical variables associated with AXL differences. The differences in AXL were significantly associated with CMT differences and SRF height differences (r = −0.616, p < 0.001, and r = −0.637, p < 0.001, respectively) (Fig. 2).
CSC is a common retinal disorder characterized by accumulation of serous fluid under the neurosensory retina in healthy, young adults. CSC is five- to six-fold more common in males than females. In the current study, the mean age of patients was 42.7 years, which included 19 (61.3%) males.
Evaluation of the macula is important in the diagnoses of many retinal diseases. Before introduction of OCT, macular edema was subjectively diagnosed using funduscopic observations. Thereafter, introduction of OCT provided cross-sectional images of retinal layers and quantified macular thickness. OCT advances have therefore facilitated imaging of the pathological features of numerous retinal diseases, including qualitative analyses of SRF and intraretinal cysts, enabling OCT to be used in the diagnosis and treatment of numerous retinal diseases.
Macular edema caused by the epiretinal membrane does not manifest significant short-term changes. Macular edema associated with diabetes or age-related macular degeneration requires more aggressive treatment such as intravitreal injection, and frequent relapses may damage the macula. In contrast, acute CSC develops a serous retinal detachment; in most cases, CSC spontaneously resolves without sequelae. Based on these results, we characterized the effects of serous retinal detachment on AXL measurements in CSC patients.
Because cataract is frequently accompanied by retinal diseases in the elderly, macular abnormalities are common in patients with cataract surgery. When macular edema is present, visual acuity may not be fully corrected after cataract surgery. For this reason, accurate postoperative refractive predictability is an important factor. To ensure a better quality of visual acuity after cataract surgery, accurate IOL power calculation is essential, and accurate biometric measurements (e.g., corneal curvature and AXL) are necessary. Inaccurate biometric measurements may significantly affect the refractive outcomes [1314]. However, many studies have reported that both autokeratometry and PCI provide biometric measurements with high accuracy, precision, and reproducibility [151617].
AXL is usually measured using ultrasound and PCI. However, the two techniques have different measurement principles; the PCI-based A XL is longer than that measured by ultrasound by approximately 0.1 to 0.2 mm [8918]. Previous studies have reported that, in macular edema, the AXL measurements using the IOL Master are more precise than those of ultrasound biometry, because the AXL is defined as the distance from the corneal vertex to the RPE, whereas ultrasound measures the distance to the anterior retinal surface. In cases of retinal detachment, which can affect the reflected peak or segmentation algorithm, AXL can be measured incorrectly [1920].
Controversy exists regarding the correlation between AXL and macular thickness measured with OCT. Kovacs et al. [2] reported a postoperative myopic shift of −0.79 D when AXL was measured for IOL power calculations in combined cataract surgery and vitrectomy in patients with macular edema, suggesting that the observed myopic shifts because of erroneous IOL calculations resulted from underestimation of AXL due to a thicker macula associated with macular edema. Ueda et al. [3] also reported a significant difference between AXL measurements using ultrasound and those with PCI in patients with diabetic macular edema. The differences in AXL measurements were positively correlated with macular thickness. However, Attas-Fox et al. [19] did not find a correlation between the differences in AXL and macular thickness, although they reported a significant difference between AXL measurements using ultrasound and PCI.
Previous reports compared the biometric characteristics of unilateral acute CSC eyes with SRF with those of nonsymptomatic fellow eyes. Moon et al. [21] performed ultrasound AXL measurements and noted that the AXL of CSC eyes with serous retinal detachment was potentially shorter due to anterior shifting of the vitreoretinal surface. Oh et al. [22] used the same PCI as the current study for AXL measurements and reported that the AXL was significantly shorter in CSC eyes than in fellow eyes (23.76 vs. 24.00 mm). The difference in AXL between eyes significantly correlated with the difference in ACD and subfoveal choroidal thickness but did not correlate with central subfoveal retinal thickness. Since we measured only CMT using SD-OCT, additional studies on the relationship between choroidal thickness and AL are needed using enhanced depth imaging-OCT.
In the present study, the AXL of CSC eyes significantly increased from 23.41 to 23.58 mm after resolution of serous retinal detachment (p < 0.001), and the difference in AXL significantly correlated with the differences in CMT and in SRF height. However, there was no significant difference in ACD between CSC eyes (3.36 mm with serous retinal detachment vs. 3.40 mm after resolution of serous retinal detachment), which did show significant difference in Oh et al. The reason for these different results may be the difference in study design between the two studies in that we compared affected eyes before and after resolution of serous retinal detachment, while Oh et al. [22] compared affected eyes with fellow eyes. Other ocular biometrics, such as spherical equivalent, average keratometry, ACD, BCVA, and IOP, did not show a significant difference before and after resolution of serous retinal detachment.
Mayer et al. [23] reported that IOL Master was not able to differentiate RPE from a dense posterior membrane and the anterior surface of the macular edema. In the present study, the AXL was shorter in CSC eyes with serous retinal detachment. This process resulted from the following possible mechanisms: 1) AXL measurements were performed on other retinal layers, not the RPE layer, because of serious retinal detachment, or RPE layers were detected more anteriorly because of increased subfoveal choroidal thickness; 2) AXL in areas other than the fovea was measured because of poor fixation associated with the accompanying visual loss (incorrect alignment would result in underestimation of AXL); and 3) light scattering of the incoming and outgoing rays can cause inaccurate AXL measurements. The amount of SRF under the macula may serve as an impediment to light penetration, resulting in erroneous measurement [24].
This study was limited by a relatively small sample size. Unlike other studies, which were retrospective, we prospectively analyzed AXL changes. In addition to the prospective study design, another advantage of this study was that it determined the longitudinal changes of unilateral CSC eyes in AXL measurements with respect to the natural course of SRF absorption, rather than using a cross-sectional study in CSC and fellow eyes.
In conclusion, the results of our study demonstrated that shortened AXL in the acute phase was restored after resolution of serous retinal detachment. Further prospective studies are needed to compare AXL measured with ultrasound biometry and that with PCI in CSC eyes, as well as studies about the effects of serious retinal detachment on AXL measurements in eyes with other retinal diseases.
Figures and Tables
 | Fig. 1Representative optical coherence tomography images of a patient with serous macular elevation with left central serous chorioretinopathy. (A) The central macular thickness was 491 µm, and the axial length measured by partial coherence interferometry was 23.31 mm in the presence of serous retinal detachment; (B) the central macular thickness decreased to 240 µm and the axial length increased to 23.75 mm after resolution of serous retinal detachment. ILM-RPE = internal limiting membrane retinal pigment epithelium; AL = axial length; SD = standard deviation; SNR = signal-to-noise ratio; K1 = flat keratometric value; D = diopters; K2 = steep keratometric value; SE = spherical equivalent; opt. ACD = optical anterior chamber depth. |
 | Fig. 2A scatterplot of the differences in central macular thicknesses and subretinal fluid height with axial lengths between eyes before and after resolution of serous retinal detachment. The differences in axial lengths were significantly associated with differences of (A) central macular thickness and (B) subretinal fluid height (r = −0.616, p < 0.001 and r = −0.637, p < 0.001, respectively) |
References
1. Hirnschall N, Leisser C, Radda S, et al. Macular disease detection with a swept-source optical coherence tomography-based biometry device in patients scheduled for cataract surgery. J Cataract Refract Surg. 2016; 42:530–536.


2. Kovacs I, Ferencz M, Nemes J, et al. Intraocular lens power calculation for combined cataract surgery, vitrectomy and peeling of epiretinal membranes for macular oedema. Acta Ophthalmol Scand. 2007; 85:88–91.

3. Ueda T, Nawa Y, Hara Y. Relationship between the retinal thickness of the macula and the difference in axial length. Graefes Arch Clin Exp Ophthalmol. 2006; 244:498–501.


4. Binkhorst RD. The accuracy of ultrasonic measurement of the axial length of the eye. Ophthalmic Surg. 1981; 12:363–365.


5. Giers U, Epple C. Comparison of a-scan device accuracy. J Cataract Refract Surg. 1990; 16:235–242.


6. Olsen T. The accuracy of ultrasonic determination of axial length in pseudophakic eyes. Acta Ophthalmol (Copenh). 1989; 67:141–144.

7. Drexler W, Findl O, Menapace R, et al. Partial coherence interferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol. 1998; 126:524–534.


8. Tehrani M, Krummenauer F, Kumar R, Dick HB. Comparison of biometric measurements using partial coherence interferometry and applanation ultrasound. J Cataract Refract Surg. 2003; 29:747–752.


9. Vogel A, Dick HB, Krummenauer F. Reproducibility of optical biometry using partial coherence interferometry: intraobserver and interobserver reliability. J Cataract Refract Surg. 2001; 27:1961–1968.


10. Liew G, Quin G, Gillies M, Fraser-Bell S. Central serous chorioretinopathy: a review of epidemiology and pathophysiology. Clin Exp Ophthalmol. 2013; 41:201–214.


11. Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013; 58:103–126.



12. Schatz H. Central serous chorioretinopathy and serous detachment of the retinal pigment epithelium. Int Ophthalmol Clin. 1975; 15:159–168.


13. Olsen T. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 1992; 18:125–129.


14. Olsen T. Prediction of the effective postoperative (intraocular lens) anterior chamber depth. J Cataract Refract Surg. 2006; 32:419–424.

15. Connors R 3rd, Boseman P 3rd, Olson RJ. Accuracy and reproducibility of biometry using partial coherence interferometry. J Cataract Refract Surg. 2002; 28:235–238.


16. Eleftheriadis H. IOLMaster biometry: refractive results of 100 consecutive cases. Br J Ophthalmol. 2003; 87:960–963.



17. Rose LT, Moshegov CN. Comparison of the Zeiss IOLMaster and applanation A-scan ultrasound: biometry for intraocular lens calculation. Clin Exp Ophthalmol. 2003; 31:121–124.


18. Packer M, Fine IH, Hoffman RS, et al. Immersion A-scan compared with partial coherence interferometry: outcomes analysis. J Cataract Refract Surg. 2002; 28:239–242.

19. Attas-Fox L, Zadok D, Gerber Y, et al. Axial length measurement in eyes with diabetic macular edema: a-scan ultrasound versus IOLMaster. Ophthalmology. 2007; 114:1499–1504.

20. Lege BA, Haigis W. Laser interference biometry versus ultrasound biometry in certain clinical conditions. Graefes Arch Clin Exp Ophthalmol. 2004; 242:8–12.


21. Moon H, Lee DY, Nam DH. Axial length in unilateral idiopathic central serous chorioretinopathy. Int J Ophthalmol. 2016; 9:717–720.



22. Oh JH, Oh J, Togloom A, et al. Biometric characteristics of eyes with central serous chorioretinopathy. Invest Ophthalmol Vis Sci. 2014; 55:1502–1508.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download