Abstract
Purpose
Methods
Results
Conclusion
Figures and Tables
 | Fig. 1Survival curves according to medical insurance status in all subjects. Overall survival curves (A) and recurrence-free survival curves (B). |
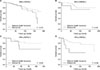
 | Fig. 2Recurrence curves according to medical insurance status. Local recurrence (A), regional recurrence (B), distant recurrence (C), and contralateral breast recurrence (D). |
 | Fig. 3Overall survival curves according medical insurance status in patients with each breast cancer subtype. HRc(+)/HER2(−) (A), HRc(+)/HER2(+) (B), HRc(−)/HER2(+) (C), and HRc(−)/HER2(−) (D). |
Table 1
Clinicopathologic characteristics of subjects according to medical insurance status

Values are presented as mean ± standard deviation or number (%).
HER2, human epidermal growth factor receptor 2.
a)P-value for mean age was calculated by t-test and all the other P-values were calculated by chi-square test. b)Education level was classified into 2 groups according to the length of education period; the high education level group (≥12 years) and the low education level group (<12 years).
Table 2
Subgroup analysis of hazard ratios according to medical insurance status regarding overall survival

CI, confidence interval; HER2, human epidermal growth factor receptor 2; HR, hazard ratio.
a)HRs are the relative risks of Medical Aid with reference of National Health Insurance regarding overall survival by Cox proportional hazards model. b)In the forest plot, a HR value of more than 1 favors National Health Insurance against Medical Aid regarding overall survival. The circles mean statistical significance and the squares mean no statistical significance. The diamond means the result of total subjects. c)Education level was classified into 2 groups according to the length of education period; the high education level group (≥12 years) and the low education level group (<12 years).
Table 3
Univariate and multivariate analysis of medical insurance status regarding overall survival

CI, confidence interval; HER2, human epidermal growth factor receptor 2; HR, hazard ratio.
a)Medical insurance status was adjusted with 11 factors which were significant by univariate analysis including tumor size, nodal positivity, estrogen receptor, progesterone receptor, histologic grade, lymphovascular invasion, age, education level, operation, chemotherapy, and endocrine therapy. b)Medical insurance status was adjusted with 10 clinicopathologic factors including tumor size, nodal positivity, estrogen receptor, progesterone receptor, HER2, histologic grade, lymphovascular invasion, age, body mass index, and education level. c)Medical insurance status was adjusted with 5 treatment factors including operation, radiation therapy, chemotherapy, Herceptin therapy, and endocrine therapy. d)Medical insurance status was adjusted with all 15 factors including 10 clinicopathologic factors and 5 treatment factors. e)Education level was classified into 2 groups according to the length of education period; the high education level group (≥12 years) and the low education level group (<12 years).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download