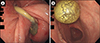
A 61-year-old man presented to the author's department with vomiting during enteral nutrition. Four months previously, the patient underwent a percutaneous endoscopic gastrostomy (PEG) due to disuse syndrome after a brain tumor surgery. In addition, a gastrostomy tube with a balloon tip had been used. The gastrostomy tube was opened to allow gastric content to flow out; however, no outflow could be observed. Emergency endoscopy revealed that the balloon tip had migrated and was stuck in the duodenal bulb (Fig. 1A), causing a gastric outlet obstruction called ball valve syndrome (BVS). Prompt deflation of the balloon was performed, and the balloon tip was returned to its proper position (Fig. 1B).
BVS was first described in 1946 by Hobbs and Cohen1 and usually refers to the gastroduodenal invagination of a large gastric polyp causing intermittent gastric outlet obstruction. BVS caused by a tip of a PEG catheter is quite rare. In this case, gastric puncture had been performed at the antrum, and the external bolster was loosened; these findings are the risk factors for BVS. Esophagogastroduodenoscopy is useful in both diagnosis and treatment of BVS. For the prevention of BVS, it is important to check whether the position of the external bolster is adequate, especially in patients using catheters with long shafts. Since BVS can lead to acute pancreatitis2 or dumping syndrome,3 prompt diagnosis and treatment are necessary.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download