INTRODUCTION
Spontaneous echo contrast (SEC) and thrombus in left atrium (LA) as well as left atrial appendage (LAA) detected in transesophageal echocardiography (TEE) were well known risk factors for cardioembolic stroke. Previous report revealed that decreased LAA emptying velocity (<55 cm/s) is an important contributor of thrombus and SEC.
1)
There has been increased use of 4-dimensional cardiac computed tomography (4DCT) for the evaluation of valve disease particularly before valve surgery or transcatheter aortic valve replacement (TAVR). In clinical field, 4DCT is utilized to evaluate native and prosthetic valve morphology and function, to measure ascending aorta, aortic root and aortic annulus related with TAVR procedure, and to evaluate subvalvular structures such as papillary muscles and chordae tendinae. In addition, volumetric data of cardiac chambers including LAA can be measured.
2)3)
Patients with valve disease are at higher risk of thrombus formation before and after surgery.
4)5) Thus, predicting thromboembolic risk and adopting tailored anticoagulation might be important to avoid catastrophic complications in patients undergoing valve surgery. The aim of this study was to investigate the role of 4DCT performed for the evaluation of valve disease before surgery to predict the risk of thrombus formation.
DISCUSSION
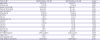
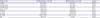
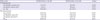
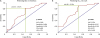
The main findings of this study are as follows: 1) EFCT and VeTEE were significantly lower in SEC/thrombus (+) group. However, FACTEE showed no correlation in regards of the presence of SEC or thrombus. 2) VeTEE was also correlated with EFCT, but FACTEE showed no correlation with EFCT. 3) Best cut-off value of LAA EF by 4DCT predicting thromboembolic risk and LAA peak emptying velocity of <55 cm/s was 37.5%.
Cardiac CT is a useful alternative to TEE for the diagnosis of LAA thrombus. Comparing CT and TEE for the diagnosis of LAA thrombus, the overall sensitivity and specificity were 96% and 92% respectively. Negative predictive value was up to 99%.
8)9) Previous studies have shown that MDCT can find potential cardiac sources of cardioembolic stroke including LAA/LA thrombus, aortic atheroma, circulatory stasis and PFO.
10)11) However, previous studies with CT acquired delayed image to evaluate LAA thrombus which is not routinely performed in most laboratories.
11) The benefit of the current method is that we can apply EF
CT in all CT scan with retrospective protocol. Further benefit of EF
CT in patients with AF or without valvular heart disease need to be investigated.
TEE has been a gold standard for the detection of cardioembolic source in stroke patients. However, there are several drawbacks to use TEE as a routine practice. First, it is a semi-invasive procedure which produces patient discomfort.
10) Patients with neurological dysfunction are more difficult to tolerate the discomfort during procedure. Second, TEE cannot detect extracardiac source of thrombus which is also an important source of embolic stroke.
12) Lastly, the ability of TEE for the detection of cardioembolic source is highly dependent by the physician and post-processing is impossible.
TEE has a superiority for temporal resolution than CT, however it can only visualize cross-sectional image of LAA with complex structure.
13) Moreover, there is a possibility to measure different cross-section during systole and diastole due to the beating effect. Functional measurements are less affected by beating effect since flow measurement is similar among whole LAA chamber regardless of the measurement site. We consider the most accurate measurement of anatomical EF
CT and it is closely related with functional parameters as well as thromboembolic risk.
In our study, LAA EF by 4DCT had benefit for the prediction of SEC or intracardiac thrombus. SEC and intracardiac thrombus are well known risk factors for cardioembolic stroke. It was also correlated with functional parameter of LAA by TEE (LAA emptying velocity <55 cm/s). Best cut-off value predicting SEC or thrombus and emptying velocity <55 cm/s was LAA EF <37.5%.
4DCT can provide useful information for the evaluation of a patient with embolic stroke. Its utility for detecting intracardiac thrombus, patent foramen ovale, aortic atheroma, and coronary artery disease was previously reported.
10)12)14) By 4DCT, we can also acquire functional information which was previously provided only by TEE. Those parameters are frequently used for thromboembolic risk assessment.
The indication of TAVR has been expanded recently, and increasing number of patients are undergoing CT before surgery or procedures. In virtue of advancement in CT protocols, patients get less radiation and contrast. Although, TEE still stands for gold standard of evaluating thromboembolic risk, 4DCT might have an alternative role which provides excellent spatial resolution and additional functional information.
This study is retrospective cross-sectional single center study with small number of patients which might inherit limitations.
Patients with normal sinus rhythm were only enrolled to fairly compare the ability of LAA EF by 4DCT and LAA FAC by TEE with correlation to thromboembolic risk in this retrospective design study. AF is an important source of thromboembolism, but thromboembolic risk still exists in the patients with normal sinus rhythm undergoing valve surgery or procedures. Future study including AF patients might be an interesting topic.
In the present study, we evaluated composite of SEC and thrombus as study endpoint and outcome data (e.g., embolic stroke or death) was not available. However, both dense SEC and thrombus are strong risk factors for future thromboembolism.
15)16)17)18) They are also related with poor clinical outcome and further studies are needed to investigate whether EF
CT is related with hard outcomes such as stroke or death. It is worth to mention that how many actual patients would suffer from true thromboembolic events and we are expecting further prospective design study with larger population to evaluate the role of 4DCT predicting actual thromboembolic event.
In conclusion, the patients who undergo 4DCT before surgical correction of valvular heart disease, LAA EF by volume analysis using 4DCT has additional benefit to evaluate future thromboembolic risk.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download