This article has been
cited by other articles in ScienceCentral.
Abstract
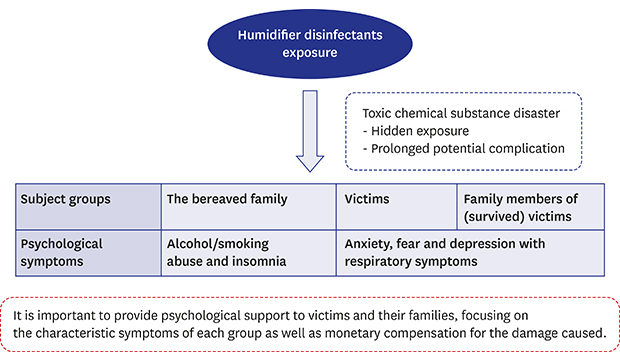
To substantiate psychological symptoms following humidifier disinfectant (HD) disasters, counseling records of 26 victims and 92 family members of victims (45 were bereaved) were analyzed retrospectively. Among the victims, 34.6% had Clinical Global Impression-Severity scores of over 4, which meant they were moderately ill. While anxiety/fear and depression with respiratory symptoms were frequently observed in victims and family members, chronic psychological distress such as alcohol/smoking abuse and insomnia was relatively high in bereaved family members. In conclusion, it is important to provide mental health support for victims and their families, focusing on the characteristic symptoms of each group as well as monetary compensation.
Keywords: Humidifier Disinfectant Disaster, Humidifier Disinfectant-associated Lung Injury, Victims and Families, Psychological Response, Toxic Chemical Substances
INTRODUCTION
In Korea, several types of chemical disinfectants that had been widely used in humidifiers since 1994 were found to be associated with lung injury, including interstitial pneumonitis and widespread lung fibrosis,
12 collectively referred to as humidifier disinfectant-associated lung injury (HDLI). In 2011, the Korea Centers for Disease Control and Prevention and the Korean Ministry of Environment began a program to collect information on individuals with respiratory disease, including lung injury, who presumed their disease to be related to the use of humidifier disinfectants (HDs), in order to determine the veracity of these claims. Approximately 75.6% of Korean children used humidifiers, and 31.1% of children were exposed to HDs.
3 As of March 2018, the number of cases of respiratory damage reported by people who thought their diseases were related to HDs exceeded 6,000. Among these cases, to date, a total of 416 people (179 deaths and 237 survivors) have been judged as having suffered from HDLI.
4
Though there have been various studies on related issues such as the examination of causal relationships between respiratory damage and HD use,
156789 discussion on a national surveillance system to track toxic chemical substances,
10 and the government's legal liability,
11 few studies focusing on psychological responses among victims have been conducted. Considering that several studies related to the sequelae of toxic chemical substance disasters pointed out physical and psychological symptoms such as posttraumatic stress disorder (PTSD), anxiety, and depression among victims,
121314 it is important to investigate psychological responses in the aftermath of HD disasters.
METHODS
After the Ministry of Environment set out to monitor physical and psychological health among HD disaster victims and their family members mainly in cooperation with Asan Medical Center (Seoul), the National Center for Mental Health, affiliated to the Ministry of Health and Welfare, was requested to conduct psychological assessment and counseling support.
In May 2016, it was decided that mental health support would be provided to 138 victims and 205 family members, as well as 288 bereaved family members who were confirmed to be suffering from respiratory diseases resulting from HDs. Subjects were assigned to 5 regional National Mental Health Centers corresponding to their areas of residence. The National Center for Mental Health (NCMH) provided psychological support to subjects in Seoul and Gyeonggi province.
The aim of the psychological support from NCMH was to screen the high risk group regarding mental health via telephone, and in case of need, refer them to the local mental health centers in communities for psychological treatment. Psychological support was carried out in accordance with the psychological support guidelines which had been shared with Asan Medical Center (Seoul) and 5 regional National Mental Health Centers. Also, trained mental health specialists and psychiatrists in charge of intervention via telephone had been educated about the procedure and the interview process in advance, and all results of the telephone counseling were shared with the psychological support team in the NCMH every day. Based on the same psychological support guidelines, mental health specialists or psychiatrists conducted primary telephone counseling and visited each subject in case of necessity from June to December 2016. A mental health specialist conducted psychological evaluation through open-ended conversations using semi-structured questions (e.g., “Have you experienced insomnia since the event?”). The evaluation interview included previous physical or mental illness, respiratory symptoms, emotional responses (e.g., sadness, depression, anger, anxiety, fear, and guilt), and behavioral responses (e.g., insomnia, avoidance, and isolation). Subjects were informed of the purpose of the counseling as well as the fact that continued counseling would be available if they provided consent.
General impressions about psychological distress were rated using the Clinical Global Impression-Severity (CGI-S)
15 scale, which has a range of responses from 1 (normal) to 7 (among the most severely ill patients). To determine the need to monitor subjects and make referrals to psychiatric hospitals or local mental health centers, the severity of psychological distress was classified into 4 levels corresponding to CGI-S scores: level 1, “normal” (CGI-S score = 1, not at all ill); level 2, “slightly normal” (CGI-S score between 2 and 3, borderline to mildly ill); level 3, “slightly bad” (CGI-S score between 4 and 5, moderately-markedly ill and possibly in need of medical treatment); and level 4, “very bad” (CGI-S score from 6–7, severely to most extremely ill, in need of support from others and possible hospitalization).
Counseling records of 118 people (26 victims, 47 family members of victims, 45 bereaved family members of victims) who cooperatively engaged in the call or counseling services provided by the NCMH were retrospectively analyzed. Family members were divided into 2 groups—bereaved because of HDs and others—to compare psychological responses. HD disaster-related symptoms were compared between 3 groups (victims, the bereaved, other family members) using χ2 tests.
Ethics statement
The study and consent exemptions were authorized by the Institutional Review Board (IRB) of the NCMH (IRB No. 116271-2016-03).
RESULTS
Among 26 victims (10 men, 38.5%; mean age, 46.2 years; standard deviation [SD], 11.2), 11 (42.3%) had reported the exposure period to HD substances, which was a minimum of 3 months to a maximum of 120 months (median 6 months). Forty-seven family members of victims (21 men, 44.7%; mean age, 42.7 years; SD, 7.6) included 32 (68.1%) parents and 13 (27.7%) spouses. Forty-five bereaved family members (25 men, 55.6%; mean age, 42.8 years; SD, 7.0) included 28 (70.0%) parents and 11 (27.5%) spouses of the deceased.
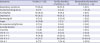
The frequency of psychological responses among victims and family members including the bereaved is described in
Table 1. It was revealed that 65.4% of victims had respiratory symptoms. Anxiety/fear and depression were the most frequently observed psychological symptoms in victims, significantly higher than in the bereaved group (38.5% and 6.7%,
P = 0.001; 35.5% and 8.9%,
P = 0.003, respectively). Also, the level of anger felt by victims (30.8%) was significantly higher than other groups (2.1% and 6.7%,
P < 0.001).
Table 1
The frequency of physical and psychological responses among humidifier disinfectant disaster victims and family members
|
Symptoms |
Victims (n = 26) |
Family members of victims (n = 47) |
Bereaved family members of victims (n = 45) |
|
Respiratory symptoms |
17 (65.4) |
10 (21.3) |
5 (11.1) |
|
Alcohol/smoking abuse |
2 (7.7) |
2 (4.3) |
7 (15.6) |
|
Anxiety/fear |
10 (38.5) |
9 (19.1) |
3 (6.7) |
|
Depression |
10 (38.5) |
10 (21.3) |
4 (8.9) |
|
Sadness/grief |
3 (11.5) |
5 (10.6) |
1 (2.2) |
|
Anger |
8 (30.8) |
1 (2.1) |
3 (6.7) |
|
Re-experience/nightmare |
3 (11.5) |
3 (6.4) |
2 (4.4) |
|
Suicidal ideation |
1 (3.8) |
0 (0.0) |
1 (2.2) |
|
Insomnia |
1 (3.8) |
2 (4.3) |
5 (11.1) |
|
CGI-S: ≥ 6 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
CGI-S: 4–5 |
9 (34.6) |
12 (25.5) |
8 (17.8) |
|
CGI-S: 2–3 |
15 (57.7) |
28 (59.6) |
29 (64.4) |
|
CGI-S: 1 |
2 (7.7) |
7 (14.9) |
8 (17.8) |

With respect to the clinical severity of psychological distress demonstrated by the CGI-S, only 7.7% of victims were classified into the “normal” group, whereas scores of 34.6% of victims were 4–5 (“slightly bad” group, possible medical treatment). Moreover, 1.2% of victims scored higher than 6 (“very bad” group, possible hospitalization). Additionally, during the interviews, victims expressed distrust and anxiety regarding chemical substances and concerns about the respiratory aftereffects of HD use, as well as chronic depression including helplessness and decline of self-confidence.
Anxiety/fear and depression were the most common symptoms among family members of victims (19.1% and 21.3%, respectively). Although family members of victims had not suffered damage to the respiratory system, they, along with the bereaved, had also experienced respiratory symptoms (21.3% and 11.1%).
However, the bereaved showed a relatively higher rate of alcohol/smoking abuse and insomnia than other psychological responses.
DISCUSSION
The findings from this study demonstrated that HD disaster victims and their family members including the bereaved still experienced psychological distress even 7 years after the event. However, the characteristics of psychological symptoms among subject groups were slightly different; victims frequently showed anxiety and fear, whereas the bereaved showed alcohol/smoking abuse and insomnia, which indicates chronic psychological distress.
With regard to the severity of psychological distress using the CGI-S, 34.6% of victims were classified into the “slightly bad” group that needed to consider psychiatric treatment. In several studies, the prevalence of PTSD in the first year after human-made/technological disasters has been documented to range between approximately 25 and 75 percent, which is generally higher than that documented in studies after natural disasters.
16 Especially in terms of the aftermath of toxic chemical substance disasters, it has been reported that prolonged psychological symptoms such as anxiety last regardless of the elapse of time. For example, among the 474 people who were exposed to methyl isocyanate gas in India, the frequency of anxiety was 65% and depression 25% even 9 years after the disaster.
13 Similarly, 32% of the Tokyo subway disaster victims exposed to sarin gas experienced PTSD symptoms even after 5 years.
12 The reasons for psychological responses lasting for such long periods after disasters could include hidden exposure and prolonged potential complications including cancer and genetic disorders.
1718
Compared to the grief and anger of family members of those who succumbed to Middle East Respiratory Syndrome and received similar psychological support from the NCMH in 2015 (81.3% and 51.6%, respectively), the grief and anger of bereaved family members of HD victims were lower. This implies that the psychological responses of the bereaved might be relieved by mourning victims' deaths. The relatively high rates of alcohol/smoking abuse and insomnia among bereaved family members of HD disaster victims imply that the bereaved might be suffering from chronic psychological distress.
It was revealed that family members of victims experienced not only anxiety and fear but also respiratory symptoms, even though their respiratory systems might not have been damaged. This result would be understandable considering previous findings, as follows: 1) toxic chemical substance disasters trigger high anxiety because it can be difficult to identify prolonged complications
18 and 2) somatization symptoms observed in toxic chemical substance disaster victims need to be regarded from both the organic and psychogenic perspectives because physical symptoms can be related to psychiatric symptoms such as anxiety, depression, and anger as well as the degree of exposure to toxic chemical substances.
17
Prolonged psychological distress among victims and their family members (including the bereaved) might be caused by the absence of adequate psychological support such as psychological first aid immediately after the event. According to Ponsford et al.,
19 patients in the non-intervention group reported more symptoms and were significantly more stressed than those in the early intervention group, which implies that psychological intervention immediately after a traumatic event mitigates psychological distress. Also, Brewin et al.
20 reported that outreach with screening, linked to the provision of evidence-based treatment, significantly mitigated posttraumatic symptoms among London bombing victims. In addition to the absence of psychological support, there can be several stressors such as monetary compensation and legal suits that arouse prolonged psychological distress. In fact, there is an outpouring of blame and anger from victims and their families toward the administration in terms of neglecting their duties in managing HD products as well as manufacturers and sellers.
Limitations of this study may be derived from analyzing the initial counseling records via telephone, which might hinder detailed examination of mental health of HDs victims. However, considering that psychological aftereffects of HD disaster have been disregarded due to the legal problems related to judgement and compensation, it is valuable to reveal the need of psychological intervention as well as financial compensation for the HDs victims. Further research is needed to elucidate the predictors of psychological responses and which way of intervention will be as effective when toxic chemical disasters occur.
In conclusion, the findings from this study imply that the psychological aftereffects of HD disasters continue despite the time elapsed. Also, victims of HD disasters mainly experience anxiety/fear, depression, and anger while bereaved family members show relatively high rates of alcohol/smoking abuse and insomnia. Hence, it is important to provide psychological support to victims and their families, focusing on the characteristic symptoms of each group as well as monetary compensation for the damage caused.