Abstract
Purpose
Methods
Results
Conclusions
Figures and Tables
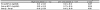
 | Figure 1Comparison of preoperative and postoperative K-MMSE score in unilateral cataract patients. ‘high score patients’ means ‘K-MMSE score more than 24, including 24’, and ‘Low score patients’ means ‘K-MMSE score less than 23, including 23’. K-MMSE = Korean mini-mental state examination; Pre-op = preoperative; Post-op = postoperative. |
Table 2
Comparison of preoperative and postoperative BCVA and K-MMSE score of study patients (87 patients)

Table 3
Comparison of preoperative and postoperative BCVA between high K-MMSE score patients and low K-MMSE score patients in unilateral cataract patients

Values are presented as mean ± standard deviation. ‘High score patients’ means ‘K-MMSE score more than 24, including 24’, and ‘Low score patients’ means ‘K-MMSE score less than 23, including 23’.
BCVA = best corrected visual acuity; K-MMSE = Korean mini-mental state examination; Pre-op BCVA = preoperative BCVA; Post-op = postoperative BCVA; Post-op - Pre-op = score difference between preoperative and postoperative.
*Measured using independent t-test.
Table 4
Comparison of preoperative and postoperative BCVA between high K-MMSE score patients and low K-MMSE score patients in bilateral cataract patients
Values are presented as mean ± standard deviation or number. ‘High score patients’ means ‘K-MMSE score more than 24, including 24’, and ‘Low score patients’ means ‘K-MMSE score less than 23, including 23’.
BCVA = best corrected visual acuity; K-MMSE = Korean mini-mental state examination; Pre-op BCVA = preoperative BCVA; Post-op = postoperative BCVA; Post-op - Pre-op = score difference between preoperative and postoperative BCVA.
*Measured using independent t-test.
Table 5
Comparison of preoperative and postoperative K-MMSE score between unilateral cataract patients and bilateral cataract patients

Values are presented as mean ± standard deviation or number.
K-MMSE = Korean mini-mental state examination; Pre-op = preoperative K-MMSE score; Post-op = postoperative K-MMSE score; Post-op - Pre-op = score difference between preoperative and postoperative K-MMSE.
*Measured using independent t-test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download