2. Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009; 180(1):59–99.

3. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007; 120(5):Suppl. S94–S138.
4. Cloutier MM, Schatz M, Castro M, Clark N, Kelly HW, Mangione-Smith R, et al. Asthma outcomes: composite scores of asthma control. J Allergy Clin Immunol. 2012; 129(3):Suppl. S24–S33.

6. Kim HS, Kim YH, Lee HS, Han YK, Park YA, Kim KW, et al. Utility of tools for the assessment of asthma control in childhood asthma. Allergy Asthma Respir Dis. 2015; 3(4):261–266.

7. Juniper EF, Gruffydd-Jones K, Ward S, Svensson K. Asthma Control Questionnaire in children: validation, measurement properties, interpretation. Eur Respir J. 2010; 36(6):1410–1416.


8. Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007; 119(4):817–825.


9. Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006; 117(3):549–556.


10. Vollmer WM, Markson LE, O'Connor E, Sanocki LL, Fitterman L, Berger M, et al. Association of asthma control with health care utilization and quality of life. Am J Respir Crit Care Med. 1999; 160(5 Pt 1):1647–1652.


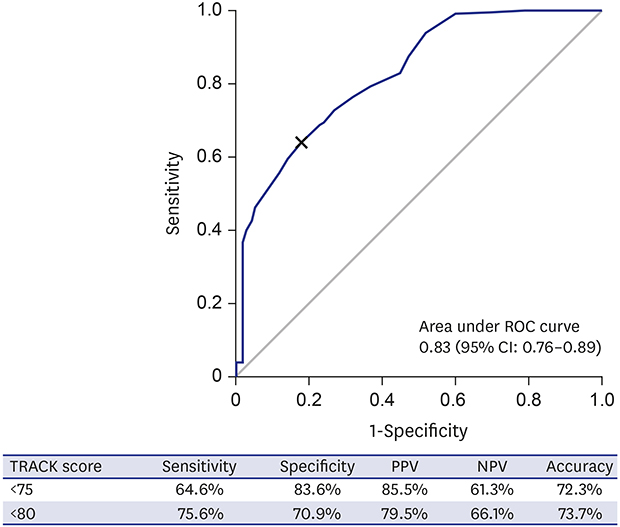
11. Murphy KR, Zeiger RS, Kosinski M, Chipps B, Mellon M, Schatz M, et al. Test for Respiratory and Asthma Control in Kids (TRACK): a caregiver-completed questionnaire for preschool-aged children. J Allergy Clin Immunol. 2009; 123(4):833–839.e9.


12. Chipps B, Zeiger RS, Murphy K, Mellon M, Schatz M, Kosinski M, et al. Longitudinal validation of the Test for Respiratory and Asthma Control in Kids in pediatric practices. Pediatrics. 2011; 127(3):e737–e747.

14. Buyuktiryaki B, Sahiner UM, Yavuz ST, Cavkaytar O, Arik Yilmaz E, Soyer OU, et al. Validation of the Turkish version of “Test for Respiratory and Asthma Control in Kids (TRACK)” questionnaire. J Asthma. 2013; 50(10):1096–1101.


15. Zeiger RS, Mellon M, Chipps B, Murphy KR, Schatz M, Kosinski M, et al. Test for Respiratory and Asthma Control in Kids (TRACK): clinically meaningful changes in score. J Allergy Clin Immunol. 2011; 128(5):983–988.


16. Oh HL, Koh YY, Suh DI, Kang BC, Kim BS, Kim WK, et al. Translation and linguistic validation of Korean version of the Test for Respiratory and Asthma Control in Kids instrument. Allergy Asthma Respir Dis. 2016; 4(1):22–30.

17. Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005; 19(1):231–240.


18. Davidson M. Known-groups validity. In : Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer;2014. p. 3481–3482. DOI:
10.1007/978-94-007-0753-5_1581.
19. Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York, NY: McGraw-Hill;1994.
21. Suh DI, Yang HJ, Kim BS, Shin YH, Lee SY, Park G, et al. Asthma severity and the controller prescription in children at 12 tertiary hospitals. Allergy Asthma Immunol Res. 2017; 9(1):52–60.


22. Sato K, Sato Y, Nagao M, Shimojo N, Yoshihara S, Adachi Y, et al. Development and validation of asthma questionnaire for assessing and achieving best control in preschool-age children. Pediatr Allergy Immunol. 2016; 27(3):307–312.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download