Abstract
Objectives
Menopause is associated with adverse metabolic changes in plasma lipoprotein and inflammation markers. Estrogens have beneficial effects on lipid metabolism and inflammation. Isoflavones (ISO) have structurally similar to estradiol. Our objective was analize the effect of soy-ISO on serum lipid and inflammatory markers (sP-selectin and sCD40L) in postmenopausal women.
Methods
A 12-week randomized, double-blind, placebo-controlled intervention with soy-ISO (50 mg, twice daily) was conducted in 35 healthy postmenopausal women (55–72 years old). The women were divided in 2 groups: 20 were allocated to soy-ISO, and 15 to a placebo group.
Results
The changes of total cholesterol (TC), triglycerides, low-density lipoproteins-cholesterol (LDL-C), high-density lipoprotein-cholesterol, Apo-A1, sP-selectin and sCD40L in 2 groups before and after 12-week treatment showed no statistical significance. In subgroup analysis, soy-ISO supplementation significantly decreased the levels of TC, LDL-C and sCD40L in women under 65 years old, and with null effects on serum lipid and inflammation markers in women over 65 years old.
Conclusions
Soy-ISO did not significantly favorable effects on the lipid profile and inflammatory markers in postmenopausal women. However, in women under 65 years of age, soy-ISO significantly decreased the TC, LDL-C and sCD40L, whereas, no effects on lipid profile and inflammation markers in women over 65 years old were observed.
In postmenopausal women, the incidence and prevalence of cardiovascular disease (CVD) are increased,1 a pathological process possibly related to the decrease in estrogen levels after the cessation of ovarian function.23 Dyslipidemia is one the most important risk factor for CVD, which can be corrected and prevented. In prospective randomized clinical trials conducted mostly in older women, menopause hormone therapy (MHT) showed that not only they do not offer protection against CVD, but they can even increase the risk of this disease.45 However, more recent studies suggest that MHT is associated with beneficial effects with regard to CVD when the therapy is initiated close to menopause but not when it is initiated later.4 Estrogen administrations is still the most effective treatment for the symptoms of menopausal and to prevent osteoporosis, in concordance to increase the health and quality of postmenopausal women's life.5 Balancing the risk versus beneficial factors of MTH, some women opt for natural forms of treatment. Phytoestrogens are a diverse group of non-steroidal substances of plant origin that are structurally similar to estradiol and have an affinity for estrogens receptors (ERs),6 ERα, and ERβ, producing estrogenic and antiestrogenic effects.7 Many foods contain phytoestrogens, but soybeans are particularly rich in isoflavones (ISO), one of the common classes of phytoestrogens.8 The ISO with the most powerful estrogenic action are genistein, daidzein, and glycitein.9 Evidences from epidemiological studies have indicated that soy-ISO consumption is associated with a lower risk of CVD, which seems to have a favorable effect on the lipid profile.10 Favorable impact of soybean ISO on plasma lipids in postmenopausal women has been reported, but the results are controversial due to the discordant nature of the data,1112 a controversy that can probably be given due to age and years from the onset of menopause in women who participated in the different trial.
Activated platelets express P-selectin as operative membrane glycoprotein, but a shorter soluble isoform has been recognized. In human, this sP-selectin occurs as the consequence of the selective splicing of the exon containing the transmembrane domain.13 Different studies have detected a relevant participation of sP-selectin in thrombus generation and triggering a pro-thrombotic state.1415 CD40L produced by stimulated platelets increases the production of adhesion molecules and inflammatory markers. The soluble structure of CD40L, which is a cleaved fragment form of surface-expressed sCD40L, is considered a platelet activation marker.16 Soluble CD40L is pro-inflammatory in endothelial cells and promotes aggregation by activation in the expression of tissue factor on monocytes and endothelial cells.17
The objective of this double-blinded, placebo-controlled study performed in postmenopausal women (age 55–73 years) was to investigate the effects of 3 months oral treatment of 50 mg of soy-ISO, twice daily, on the lipid profile and plasma level of sP-selectin and sCD40L.
The study protocol was reviewed and approved by the Institute of Nutrition and Food Technology, University of Chile Review Board Human Subjects Committee. Thirty-five women, aged 55 to 72 years, were recruited from Santiago Metropolitan area, and gave written informed consent to participate in this study. To be eligible for this study, women had to be in menopause at least 6 months, have follicle-stimulating hormone levels over 20 IU/L, without any type of hormonal treatment during previous 6 months, and not currently using lipid-lowering drugs, soybean-derived products, or herbal supplements diets. Exclusion criteria included: cigarette smoking within the last 5 years, diabetes, heavy alcohol consumption (more than 30 g/day), hypertension, abnormal uterine bleeding, and coexistent major illnesses. Volunteers were randomly assigned to receive 2 daily capsules of a soy-ISO extract (50 mg ISO capsule) or identical placebo during 12 consecutive weeks. ISO extract correspond to a NovaSoy® 400 (Archer Daniels Midland Company, Decatur, IL, USA), and have a ratio of 1.3:1:0.2 for genistein: daidzein: glycitein. The placebo capsules were identical in size and colors and contained starch. The study coordinator and investigative team performing the blood collection, and assays were blinded to the group assignment.
Total plasma cholesterol (TC), High-density lipoprotein-cholesterol (HDL-C), and total triacylglycerols (TG) were quantified by commercially available kits (Sigma Diagnostics, St Louis, MO, USA). Low-density lipoproteins-cholesterol (LDL-C) was calculated by using the Friedewald equation.18 Morning fasting blood samples were collected from all subjects on an assigned date. Serum P-selectin and sCD40L were quantified using an ELISA kit (R&D System, In Minneapolis reactive, MN, USA). Assay was carried out on diluted samples following manufacturer's instructions.
Measurement soluble CD40L was determined according to the methodology described by Allanore et al.19. Blood samples (10 mL) were collected in tubes containing EDTA, and plasma was separated by centrifugation within 30 minutes of collection. After separation, plasma was stored at −80℃ until use. Plasma sCD40L was measured by Human sCD40-Ligand Quantikine kit (R&D System).
Results are expressed as means ± standard deviation. A P-value of less than 0.05 was considered significant. Difference between the groups at baseline was evaluated by the Wilcoxon signed-rank test. Data analysis was performed using Software STATA SE version 12 (StataCorp., College Station, TX, USA).
Of the 65 postmenopausal screened, 38 were randomized, 18 placebo and 20 ISO. Thirty-five participants of the 38 enrolled concluded the study and 3 women from the placebo group left the study due to personal reasons.
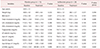
The baseline characteristics between women randomized to placebo (n = 15) and ISO (n = 20) were similar; treatment groups did not differ with respect to age, cholesterol, lipoprotein, sP-selectin and sCD40L. Compliance with the protocol of supplement intake in the groups was assessed by package and capsules count and found to be >85% among both the placebo-treated and ISO-treated participants. The result of the serum biochemical parameters, shown in Table 1, indicate that there was no difference in the levels of total cholesterol, LDL-C, HDL-C, triglycerides, Apo-A1, sP-selectin and sCD40L within-group comparisons of baseline (P > 0.05) and 3 months values (P > 0.05) and between the 2 groups after treatment (P > 0.05). However, the data obtained within-group comparison of baseline and 3 months value, demonstrated a significant increase in Apo-B in the placebo group (P = 0.028) and a significant decrease in the ISO-group (P = 0.044). This decrease in Apo-B levels was also significant between groups (P = 0.047).
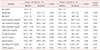
In the case of women who received ISO, we tested the hypothesis that ISO-supplement on cardiovascular risk factors in the postmenopause may be associated with the age of the woman. The effect of ISO on lipoprotein profiles and inflammation markers among subgroups (women <65 years old, and women >65 years old) is shown in Table 2. Within sub-group <65 years, ISO-supplement caused a significant decrease in TC (P = 0.007), LDL-C (P = 0.013) and sCD40L (P = 0.016). However, within sub-group >65 years, ISO-supplement has no effect on plasma lipid levels, but was observed a significant decrease in Apo-B (P = 0.028).
The aim of the present double-blind, randomized placebo-controlled study was to analyze the effect of supplementation of soy-ISO over 12 weeks on the lipid profile, apolipoprotein and inflammation markers in postmenopausal women (55–72 years old). We found that the effect of oral supplementation at a dose of 100 mg/day for 12 weeks did not change plasma lipid, sCD40L and sP-selectin. This study revealed a moderate (~13%) but statistically significant increase in serum Apo B. In subgroup analysis, ISO supplementation significantly decreased the serum levels of TC, LDL-C and sCD40l in women under 65 years old, and with no effects on serum plasma lipid and inflammation markers in women over 65 years old.
Dyslipidemia is a well-studied cardiovascular risk factor and the onset of menopause increase blood level of TC, TG and LDL-C, and increased as well LDL-C/HDL-C ratio and TC/HDL-C ratio.2021 Reports demonstrate that the estrogen action on lipid variations would be dependent on aging. In fact, several studies suggest that estrogen therapy is related to favorable effect cardiovascular risk factor when the treatment is initiated close to the time of menopause.2223
ISO are natural substances that are found in a wide range of plants kingdom species, and that weakly bind to ERs. There are 2 types of ERs: ERα and ERβ. ISO can bind to either ERα or ERβ; however, ISO appears to have a higher affinity for ERβ.24 The activation of ERs by ISO is selective, that means that in some tissues act like estrogen and in others, as anti-estrogens.25 Therefore, studies in postmenopausal women have shown that soy protein and ISO reduces serum TC and LDL-C, and increase HDL-C concentration. However, given the inconsistency of these results, the action of soy-ISO on lipid profile is controversial.26 The results of our study may explain, in part, this inconsistency since ISO did not have a favorable impact on the profile of serum lipids in postmenopausal women of 55 to 72 years, although the effects were observed in the subgroup of younger postmenopausal women. In recent years, soy or ISO intervention studies2728 have found little or no benefit on serum lipid profiles. Our results are consistent with that of others; neither soy protein nor ISO alone demonstrated meaningful effects on serum lipids or inflammatory markers in older, postmenopausal women.
Inflammation is a central process to CVD, and in this aspect platelets play crucial roles. The CD40-CD40L is as considered as a pro-inflammatory marker and has been identified on several cells, however the majority of the circulating levels (~95%) comes from platelets.29 Platelets express CD40L on their cell membrane upon activation, and CD40L is then cleaved and circulates as sCD40L. When expressed on the cell membrane of platelets and exposed to CD40-bearing vascular cells, platelet-associated CD40L is capable to activate diverse inflammatory responses.30 In the present study, ISO supplementation decreases serum sCD40L levels in women <65 years old.
In different physiological and pathological situations, the stimulation of platelets is depending upon the interaction between von Willebrand factor and glycoprotein Ib/IX/V.31 Interestingly, Enomoto et al.32 reported that ristocetin, an activator of glycoprotein Ib/IX/V, induce the release of sCD40L in human platelets via thromboxane A2 (TxA2) production. Several studies, including ours, have demonstrated that inhibition of specific flavonoid in in vitro platelet aggregation induced by collagen, arachidonic acid and TxA2 agonist, seems to be largely related to their ability to compete for the binding to TxA2 receptor.3334 On the other hand, ours in vitro studies showed that ristocetin-stimulated sCD40L release from platelets from postmenopause women was significantly inhibited with equol, a metabolite of daidzein.35
The results obtained in the present investigation are relevant, although the study design present some limitations. In fact, it was not considered analyzing the effect of soy-ISO in early and late postmenopausal women. Thus, the number of individuals in the subgroups is low and the years of menopause in each volunteer are not known. On the other hand, it is necessary to measure other pro-inflammatory molecules.
In summary, our results may further contribute to the understanding of the physiological impact of the epidemiological finding that soy-ISO decreases the risk of CVD. The results of this investigation show that the effect of supplementation of ISO, at the dose of 100 mg/day, did no significantly exert a favorable effect on the lipid profile and CD40-CD40L system in postmenopausal women. However, a subgroup analysis suggests that effect of supplementation of ISO on lipid variable and inflammatory marker is age dependent, and is observed only in postmenopause women younger than 64 years.
Figures and Tables
Table 1
Lipoprotein profiles and inflammation markers in women treated with isoflavone or placebo for 3 months
Acknowledgement
This study was funded by Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT) 1100299 and Enlace Project ENL007 University of Chile.
References
1. Mendelsohn ME, Karas RH. Molecular and cellular basis of cardiovascular gender differences. Science. 2005; 308:1583–1587.

2. Cui J, Shen Y, Li R. Estrogen synthesis and signaling pathways during aging: from periphery to brain. Trends Mol Med. 2013; 19:197–209.

4. Manson JE, Hsia J, Johnson KC, Rossouw JE, Assaf AR, Lasser NL, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003; 349:523–534.

5. Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA. 1998; 280:605–613.
6. Cano A, García-Pérez MA, Tarín JJ. Isoflavones and cardiovascular disease. Maturitas. 2010; 67:219–226.

7. Bertonazzi A, Nelson B, Salvador J, Umland E. The smallest available estradiol transdermal patch: a new treatment option for the prevention of postmenopausal osteoporosis. Womens Health (Lond). 2015; 11:815–824.

8. Munro IC, Harwood M, Hlywka JJ, Stephen AM, Doull J, Flamm WG, et al. Soy isoflavones: a safety review. Nutr Rev. 2003; 61:1–33.

9. Vitale DC, Piazza C, Melilli B, Drago F, Salomone S. Isoflavones: estrogenic activity, biological effect and bioavailability. Eur J Drug Metab Pharmacokinet. 2013; 38:15–25.

10. An J, Tzagarakis-Foster C, Scharschmidt TC, Lomri N, Leitman DC. Estrogen receptor beta-selective transcriptional activity and recruitment of coregulators by phytoestrogens. J Biol Chem. 2001; 276:17808–17814.
11. Messina M. Soy and health update: Evaluation of the clinical and epidemiologic literature. Nutrients. 2016; 8:E754.

12. Taku K, Umegaki K, Sato Y, Taki Y, Endoh K, Watanabe S. Soy isoflavones lower serum total and LDL cholesterol in humans: a meta-analysis of 11 randomized controlled trials. Am J Clin Nutr. 2007; 85:1148–1156.

13. Fujimoto TT, Noda M, Takafuta T, Shimomura T, Fujimura K, Kuramoto A. Expression and functional characterization of the P-selectin glycoprotein ligand-1 in various cells. Int J Hematol. 1996; 64:231–239.
14. Myers DD, Hawley AE, Farris DM, Wrobleski SK, Thanaporn P, Schaub RG, et al. P-selectin and leukocyte microparticles are associated with venous thrombogenesis. J Vasc Surg. 2003; 38:1075–1089.

15. André P, Hartwell D, Hrachovinová I, Saffaripour S, Wagner DD. Pro-coagulant state resulting from high levels of soluble P-selectin in blood. Proc Natl Acad Sci U S A. 2000; 97:13835–13840.
16. Mach F, Schönbeck U, Bonnefoy JY, Pober JS, Libby P. Activation of monocyte/macrophage functions related to acute atheroma complication by ligation of CD40: induction of collagenase, stromelysin, and tissue factor. Circulation. 1997; 96:396–399.
17. Lindmark E, Tenno T, Siegbahn A. Role of platelet P-selectin and CD40 ligand in the induction of monocytic tissue factor expression. Arterioscler Thromb Vasc Biol. 2000; 20:2322–2328.

18. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502.

19. Allanore Y, Borderie D, Meune C, Lemarechal H, Weber S, Ekindjian OG, et al. Increased plasma soluble CD40 ligand concentrations in systemic sclerosis and association with pulmonary arterial hypertension and digital ulcers. Ann Rheum Dis. 2005; 64:481–483.

20. Miller VT, LaRosa J, Barnabei V, Kessler C, Levin G, Smith-Roth A, et al. Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA. 1995; 273:199–208.
21. Alwers R, Urdinola J, Onatra W, Sánchez F, Posso H. Changes in normal lipid profile of menopausal women with combined hormone replacement therapy. Comparative clinical trial of two hormonal combinations (conjugated estrogens/medroxyprogesterone acetate versus estradiol valerate/cyproterone acetate). Maturitas. 1999; 32:41–50.
22. Harman SM, Vittinghoff E, Brinton EA, Budoff MJ, Cedars MI, Lobo RA, et al. Timing and duration of menopausal hormone treatment may affect cardiovascular outcomes. Am J Med. 2011; 124:199–205.

23. Hodis HN, Mack WJ, Shoupe D, Azen SP, Stanczyk FZ, Hwang-Levine J, et al. Methods and baseline cardiovascular data from the Early versus Late Intervention Trial with Estradiol testing the menopausal hormone timing hypothesis. Menopause. 2015; 22:391–401.

24. Kuiper GG, Lemmen JG, Carlsson B, Corton JC, Safe SH, van der Saag PT, et al. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology. 1998; 139:4252–4263.
25. Oseni T, Patel R, Pyle J, Jordan VC. Selective estrogen receptor modulators and phytoestrogens. Planta Med. 2008; 74:1656–1665.

26. Li J, Liu Y, Wang T, Zhao L, Feng W. Does genistein lower plasma lipids and homocysteine levels in postmenopausal women? A meta-analysis. Climacteric. 2016; 19:440–447.

27. Mangano KM, Hutchins-Wiese HL, Kenny AM, Walsh SJ, Abourizk RH, Bruno RS, et al. Soy proteins and isoflavones reduce interleukin-6 but not serum lipids in older women: a randomized controlled trial. Nutr Res. 2013; 33:1026–1033.

28. Simental-Mendia LE, Gotto AM Jr, Atkin SL, Banach M, Pirro M, Sahebkar A. Effect of soy isoflavone supplementation on plasma lipoprotein(a) concentrations: A meta-analysis. J Clin Lipidol. 2018; 12:16–24.
29. Nagasawa M, Zhu Y, Isoda T, Tomizawa D, Itoh S, Kajiwara M, et al. Analysis of serum soluble CD40 ligand (sCD40L) in the patients undergoing allogeneic stem cell transplantation: platelet is a major source of serum sCD40L. Eur J Haematol. 2005; 74:54–60.

30. Gerdes N, Seijkens T, Lievens D, Kuijpers MJ, Winkels H, Projahn D, et al. Platelet CD40 exacerbates atherosclerosis by transcellular activation of endothelial cells and leukocytes. Arterioscler Thromb Vasc Biol. 2016; 36:482–490.

31. Gresele P, Momi S. Inhibitors of the interaction between von Willebrand factor and platelet GPIb/IX/V. Handb Exp Pharmacol. 2012; 287–309.

32. Enomoto Y, Adachi S, Matsushima-Nishiwaki R, Doi T, Niwa M, Akamatsu S, et al. Thromboxane A(2) promotes soluble CD40 ligand release from human platelets. Atherosclerosis. 2010; 209:415–421.

33. Guerrero JA, Lozano ML, Castillo J, Benavente-García O, Vicente V, Rivera J. Flavonoids inhibit platelet function through binding to the thromboxane A2 receptor. J Thromb Haemost. 2005; 3:369–376.

34. Muñoz Y, Garrido A, Valladares L. Equol is more active than soy isoflavone itself to compete for binding to thromboxane A(2) receptor in human platelets. Thromb Res. 2009; 123:740–744.

35. Gonzalez N, Garrido A, Acevedo I, Valladares L. In vitro effect of soy isoflavone and equol on soluble CD40L release stimulated by ristocetin in platelets from postmenopause women. JBiSE. 2015; 8:24–30.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download