Journal List > Asian Oncol Nurs > v.18(4) > 1111246
The purpose of this study was to compare the differences in the performance of life-sustaining treatment after signing a do-not-resuscitate (DNR) order between terminal cancer patients who died in the cancer unit and hospice unit.
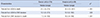
We performed a retrospective analysis of 174 patients who died in the cancer unit (CU) and 68 patients who died in the hospice unit (HU) from January 1, 2016 to December 31, 2016 at a hospital specializing in cancer treatment.
The rate of life-sustaining treatment administration was lower for patients who died in the HU than that of those who died in the CU. The period until death after signing a DNR order was 7 days for CU patients and 19.5 days for the HU patients. The period from admission to death was also significantly longer in HU patients (32.5 days) than that in CU patients (21.5 days, p<.001). Of the patients who died in the CU, 54% were referred to the HU but did not use the service. Most of the people who signed DNR informed consents were spouses and offspring; only 4.6% of patients signed DNRs.
It is hard to say that life-sustaining treatment increases the survival period, but it can improve symptom control and quality of life in hospices. Activation of consultation-based hospice is necessary for patients who cannot use the hospice unit. To increase patient's active participation in the life-sustaining treatment decision of terminal cancer patients, it is necessary that an advanced practice nurse specialized in counseling and education is involved in the decision.
1. National Cancer Information Center (KR). Mortality of major cancer in 2016 [Internet]. Accessed October 16, 2017. Available from: https://www.cancer.go.kr.
2. Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000; 132:825–832.

3. Oh DY, Kim JE, Lee CH, Lim JS, Jung KH, Heo DS, et al. Discrepancies among patients, family members, and physicians in Korea in terms of values regarding the withholding of treatment from patients with terminal malignancies. Cancer. 2004; 100:1961–1966.

4. Yoon HM, Choi YS, Hyun JJ. Current situation on signing advance medical directives and actual life-sustaining treatment given at a university hospital. Korean J Hosp Palliat Care. 2011; 14:91–100.

5. Koh Y, Heo DS, Yun YH, Moon JL, Park HW, Choung JT, et al. Charactersitics and issues of guideline to withdrawal of a life-sustaining therapy. J Korean Med Assoc. 2011; 54:747–757.

6. Chiu TY, Hu WY, Chuang RB, Chen CY. Nutrition and hydration for terminal cancer patients in Taiwan. Support Care Cancer. 2002; 10:630–636.

7. Bruera E, Hui D, Dalal S, Torres-Vigil I, Trumble J, Roosth J, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013; 31:111–118.

8. Morita T, Shima Y, Miyashita M, Kimura R, Adachi I;. Physician- and nurse-reported effects of intravenous hydration therapy on symptoms of terminally ill patients with cancer. J Palliat Med. 2004; 7:683–693.

9. Chen LK, Chou YC, Hsu PS, Tsai ST, Hwang SJ, Wu BY, et al. Antibiotic prescription for fever episodes in hospice patients. Support Care Cancer. 2002; 10:538–541.

10. Jeong HS, Kim DY, Song KP, Suh SY, Group KF, Group KF. Antibiotics use in infected patients with terminal stage of cancer: based on Seminar of Korean Family Medicine Palliative Medicine Research Group. Korean J Hosp Palliat Care. 2007; 10:43–47.
11. Oh DY, Kim JH, Kim DW, Im SA, Kim TY, Heo DS, et al. Antibiotic use during the last days of life in cancer patients. Eur J Cancer Care (Engl). 2006; 15:74–79.

12. Helde-Frankling M, Bergqvist J, Bergman P, Björkhem-Bergman L. Antibiotic treatment in end-of-life cancer patients-a retrospective observational study at a palliative care center in Sweden. Cancers (Basel). 2016; 8:pii: E84.

13. Kim MJ, Noh SM, Ryu EJ, Shin SM. Research trend analysis of do-not-resuscitate decision: based on text network analysis. Asian Oncol Nurs. 2014; 14:254–264.

14. Kim HA, Park JY. Changes in life-sustaining treatment in terminally ill cancer patients after signing a do-not-resuscitate order. Korean J Hosp Palliat Care. 2017; 20:93–99.

15. Baker JN, Kane JR, Rai S, Howard SC, Hinds PS. PCS Research Working Group. Changes in medical care at a pediatric oncology referral center after placement of a do-not-resuscitate order. J Palliat Med. 2010; 13:1349–1352.

16. McGorty EK, Bornstein BH. Barriers to physicians' decisions to discuss hospice: insights gained from the United States hospice model. J Eval Clin Pract. 2003; 9:363–372.

17. Ro YJ, Han SS, Yong JS, Song MS, Hong JU. A comparison of nursing Interventions with terminal cancer patients in a hospice unit and general units. J Korean Acad Adult Nurs. 2002; 14:543–553.
18. Baek SK, Chang HJ, Byun JM, Han JJ, Heo DS. The association between end-of-life care and the time interval between provision of a do-not-resuscitate consent and death in cancer patients in Korea. Cancer Res Treat. 2017; 49:502–508.

19. Higashiguchi T, Ikegaki J, Sobue K, Tamura Y, Nakajima N, Futamura A, et al. Guidelines for parenteral fluid management for terminal cancer patients. Jpn J Clin Oncol. 2016; 46:986–992.

20. Yamaguchi T, Morita T, Shinjo T, Inoue S, Takigawa C, Aruga E, et al. Effect of parenteral hydration therapy based on the Japanese national clinical guideline on quality of life, discomfort, and symptom intensity in patients with advanced cancer. J Pain Symptom Manage. 2012; 43:1001–1012.

21. Celso BG, Meenrajan S. The triad that matters: palliative medicine, code status, and health care costs. Am J Hosp Palliat Care. 2010; 27:398–401.

22. Becker G, Sarhatlic R, Olschewski M, Xander C, Momm F, Blum HE. End-of-life care in hospital: current practice and potentials for improvement. J Pain Symptom Manage. 2007; 33:711–719.

23. Seo IS, Shin MH, Hong SH. Needs of hospice care and quality of life for cancer patients. Korean J Hosp Palliat Care. 2010; 13:89–97.

24. Ambroggi M, Biasini C, Toscani I, Orlandi E, Berte R, Mazzari M, et al. Can early palliative care with anticancer treatment improve overall survival and patient-related outcomes in advanced lung cancer patients? A review of the literature. Support Care Cancer. 2018; 26:2945–2953.

25. Brickner L, Scannell K, Marquet S, Ackerson L. Barriers to hospice care and referrals: survey of physicians’ knowledge, attitudes, and perceptions in a health maintenance organization. J Palliat Med. 2004; 7:411–418.

26. Lee JR, Lee JK, Hwang S, Kim JE, Chung JI, Kim SY. Doctor's perception and referral barriers toward palliative care for advanced cancer patients. Korean J Hosp Palliat Care. 2012; 15:10–17.

27. Ciemins EL, Blum L, Nunley M, Lasher A, Newman JM. The economic and clinical impact of an inpatient palliative care consultation service: a multifaceted approach. J Palliat Med. 2007; 10:1347–1355.

28. Hanson LC, Usher B, Spragens L, Bernard S. Clinical and economic impact of palliative care consultation. J Pain Symptom Manage. 2008; 35:340–346.

- TOOLS
- ORCID iDs
-
Eun Jeong Nam

https://orcid.org/0000-0001-5481-2336Se-Na Lee

https://orcid.org/0000-0003-4873-1913 - Similar articles




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download