Abstract
Tracheobronchopathia osteoplastica (TO) is a rare benign disease in which the anterior inner wall of the tracheobronchus changes because of abnormal chondrogenesis or ossification, while the posterior wall of the trachea is spared. The etiology is not clearly understood, but may relate with chronic infection, inflammation, and trauma. In some case studies, it has also been reported to be accompanied by other chronic diseases such as atrophic rhinitis and amyloidosis. However, Coexistence of TO and tuberculosis has rarely been reported, and has never been reported in Korea. Here, we report a case of a 70-year-old male patient who complained of hemoptysis and whose case was diagnosed as TO and pulmonary tuberculosis through bronchoscopy with bronchial washing and biopsy.
Tracheobronchopathia osteochodroplastica is a rare benign disease in which multiple osteochondral submucous noduli protrude in the internal tracheal bronchus.
Since tracheobronchopathia osteochodroplastica is mostly symptomless, the disease was previously found mostly during autopsy prior to the introduction of bronchial endoscopy. Due to the recent developments in, and the introduction of, radiological tests, the disease is often an incidental finding and confirmed through bronchial endoscopy.
Although the pathogenic mechanisms of tracheobronchopathia osteochodroplastica and its correlation with smoking are not clearly known, some chronic diseases such as infection, inflammation, trauma, atrophic rhinitis, and amyloidosis are expected to be correlated with tracheobronchopathia osteochodroplastica. However, patients with both tracheobronchopathia osteochodroplastica and tuberculosis are a rare phenomenon that has not yet been reported in Korea.
The authors herein report a case of a 70-year-old patient who visited our institution with the chief complaint of hemoptysis and who was diagnosed with tracheobronchopathia osteochodroplastica and accompanying pulmonary tuberculosis via bronchial washing and bronchial endoscopy performed in addition to biopsy.
A 70-year-old male patient visited the emergency room at our institution with the chief complaint of hemoptysis accompanied by coughing, which had started earlier that morning. The patient had been diagnosed with tuberculosis 10 years earlier, and his doctor informed him that he had completely recovered following administration of an antituberculosis drug for 6 months. The patient complained of recurrence of his intermittent and relatively long-lasting cough from 5 years ago. The patient visited the emergency room because the routine and intermittent cough was suddenly exacerbated at about 8 o'clock that morning, and one instance of hemoptysis of about 400 mL also occurred.
The patient had been diagnosed with tuberculosis, hypertension, and diabetes about 5 years ago, and he was taking an antihypertensive drug and an oral hypoglycemic agent from a nearby medical clinic. The patient is not a smoker, but had consumed two bottles of Soju (Korean distilled spirit) daily for about 30 years.
Pulmonary sound auscultation was performed during the physical examination; weak wheezing and rales were heard from the right upper lobe of the lung. No specific sounds were heard during heart sound auscultation. At the time the patient visited our institution, his blood pressure was 130/80 mmHg, his heart rate was 110 beats/min, and his respiratory rate was 20 breaths/min. No particularly worrisome findings were shown during examinations of the patient's head, abdomen, or upper and lower limbs, and the patient's neurologic examination was unremarkable.
The blood test results were as follows: white blood cell count, 8,850/mm3; hemoglobin, 15.3 g/dL; and platelets, 254,000/mm3, all of which were within normal range. The arterial blood gas analysis results were as follows: oxygen saturation, 98%; arterial oxygen partial pressure, 96 mmHg; arterial carbon dioxide partial pressure, 30 mmHg; and arterial blood pH, 7.44 with no particularly notable findings. The biochemical test showed no remarkable findings except for a mild increase in C-reactive protein to 0.78 mg/dL.
The plain chest X-ray radiography performed at the time the patient visited our institution showed a local shadow increase of 40×15 mm2 in the middle of the right lung with multiple nodular shadow increases in the right upper lobe of the lung (Fig. 1).
Contrast-enhanced chest CT showed multiple centrilobular noduli and ground-glass opacity in the superior segment of the right upper lobe and the right lower lobe (Fig. 2A), as well as an endotracheal nodule on the right wall at the lower two-thirds of the trachea (Fig. 2B).
On the basis of the patient's clinical pattern and the radiographic findings, pulmonary tuberculosis at the right upper lobe and endotracheal tuberculosis were initially suspected. Bronchoscopy was performed to verify the lesions and to determine the hemorrhagic regions in the trachea and bronchus. As a result, multiple white-colored nodular spots were observed above the tracheal bifurcation point, at the lower two-thirds of the lower trachea (Fig. 3A); and two polyp-shaped lesions were found in the right middle lobe bronchus (Fig. 3B).
After performing bronchial washing in the right upper lobe, a biopsy of the lesions was performed. The biopsy showed ossified cartilage tissue, which is associated with tracheobronchopathia osteochodroplastica, but there were no findings of chronic granulomatous inflammation, suggestive of tuberculosis (Fig. 4, 5).
In addition, the liquid taken from the bronchial washing during bronchoscopy yielded positive results in both the acid-fast bacterium smear test and the nucleic acid amplification test. Therefore, under the diagnosis of tuberculosis, a four-drug regimen including isoniazid, rifampin, ethambutol, and pyrazinamide was started. After 10 days of the antituberculosis drug administration, the patient did not show any more symptoms of hemoptysis, and the sputum smear test yielded a negative result. Therefore, following the discontinuation of isolation, the patient was discharged without any complications and is currently being monitored by outpatient's consulting.
Tracheobronchopathia osteochodroplastica, first reported as “ossific deposits in the larynx, trachea and bronchi” by Wilkis in 1857,1 is a rare benign disease where abnormal cartilaginification and ossification on anterior lateral wall of the internal tracheal bronchus replace the normal tissue.2
The prevalence of tracheobronchopathia osteochodroplastica is not exactly known, but the disease has been reported in 1 of 400 autopsy cases, and it has also been observed in 2–7 individuals out of a total of 1,000 bronchial endoscopy cases.3 Patients diagnosed with tracheobronchopathia osteochodroplastica are usually in their 60s or 70s, but it has also been reported in a 12-year-old boy. The prevalence of the disease is slightly higher in males than in females.4
The cause of tracheobronchopathia osteochodroplastica is not clear, but it has been reported that the disease may be caused by chronic infection, inflammation, trauma, amyloidosis, and silicosis. There is also a report of a case in which tracheobronchopathia osteochodroplastica was accompanied by atrophic rhinitis.56 There are currently no reports on the direct correlation between tuberculosis and tracheobronchopathia osteochodroplastica, but there are a few cases in which patients were diagnosed with both diseases, indicating that the two diseases may be correlated.7
The pathological mechanism of tracheobronchopathia osteochodroplastica is still controversial, but two well-known hypotheses have been developed. The first hypothesis, proposed by Virchow, is that tracheobronchopathia osteochodroplastica is caused by exostosis.8 The second hypothesis, proposed by Aschoff, is that tracheobronchopathia osteochodroplastica is caused by ossification of the tracheal elastic connective tissues.9
Tracheobronchopathia osteochodroplastica does not have a characteristic symptom that facilitates its clinical diagnosis; it is also symptomless in most cases.10 Expressed symptoms are usually caused by airway obstruction, causing cough, dyspnea, sputum, wheezing, and hemoptysis, and are sometimes accompanied by repeated infection in the respiratory system.11 In the present case, the patient visited our institution with the chief complaint of hemoptysis, which was found to be accompanied by tuberculosis. Bronchial endoscopy showed hemoptysis at the right upper lobe.
During the diagnosis of tracheobronchopathia osteochodroplastica, plain chest X-ray radiography usually yields a normal result, and thus does not aid in the diagnosis, as in the present case. The chest CT of tracheobronchopathia osteochodroplastica shows multiple calcareous submucous nodules, each of which has a diameter of 1–3 mm and protrudes to the internal trachea or bronchus.12 The lesions are usually found on the anterior side wall of the trachea, and thus the disease is differentiated from amyloidosis, in which the posterior wall is invaded; it is also distinct from relapsing polychondritis, endobronchial sarcoidosis, papillomatosis, and tracheobronchomalacia. Bronchial endoscopy and biopsy may aid in the differential diagnosis.13
Bronchial endoscopic findings of tracheobronchopathia osteochodroplastica include protrusion of while-colored and solid nodules into the trachea. The posterior wall is not usually invaded, but the larynx and the main bronchus are rarely invaded.14 In the present case, the posterior wall was not invaded, and the nodules were found starting at the top-third of the lower trachea to the bifurcation point of the trachea, as well as in the bronchus of the right pulmonary middle lobe.
The necessity of biopsy may still be controversial, but a biopsy was performed in the present case to exclude endotracheal tuberculosis for differential diagnosis. The biopsy of tracheobronchopathia osteochodroplastica may show squamous metaplasia, submucous cartilaginification, and submucous ossification, as well as calcification and hemopoietic marrow cells in the ossified regions.7 In the present case, pathological examination of the specimen taken from the submucous lesions also showed hemopoietic marrow cells in the ossified tissues, as well as hyaline cartilage tissues without chronic granulomatous inflammation, suggesting tuberculosis.
The pulmonary function test shows fixed obstruction of the upper airway,15 which was not found in the present case; as such, a pulmonary function test could not be performed due to tuberculosis.
There is no particular therapy for the disease, and thus symptomatic treatment may be conducted. If there is no response to the symptomatic treatment, a surgical therapy or an endoscopic interventional procedure may be considered.
In conclusion, a case of a tracheobronchopathia osteochodroplastica patient with tuberculosis is a rare phenomenon globally, and has not yet been reported in Korea. Although the correlation between tracheobronchopathia osteochodroplastica and tuberculosis is not well known, the present report is significant, as it is the first reported case of a tracheobronchopathia osteochodroplastica patient with tuberculosis.
More studies may need to be conducted on tracheobronchopathia osteochodroplastica, particularly pertaining to the etiology and pathophysiology of this condition, as well as to investigate its correlation with other diseases.
Figures and Tables
Fig. 1
Chest X-ray reveals multiple nodular opacities in the right upper lung field (arrows) with a 40 × 15 mm2 focal opacity in the right middle lung field (arrowhead).

Fig. 2
Chest computed tomography shows clustered centrilobular nodules (arrows with solid line) and ground glass attenuation (arrows with dashed line) in the right upper lobe and the superior segment of the right lower lobe (A), with endotracheal nodules on the right wall of the interior two-thirds of the trachea (arrowhead) (B).

Fig. 3
Bronchoscopy reveals multiple whitish nodules and patches in the lower trachea above carina (A) and two nodules (arrows) in the bronchus of the right middle lobe (B).

Fig. 4
Biopsy sample with lamellar structures which are similar to cortical bone. Polarized light makes the lamellar structures more visible. (polarized light, hematoxylin and eosin, ×200).
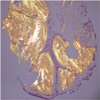
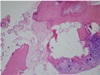
Fig. 5
Osseous tissue with marrow spaces is found just beneath the pseudostratified respiratory epithelium. The marrow cavity is filled with some erythropoietic cells and mature adipose tissue. At the periphery, a focal remnant of hyaline cartilage is seen. Collectively, these histological findings indicate tracheobronchopathia osteoplastica (hematoxylin and eosin, ×200).
References
1. Wilks S. Ossific deposits on larynx, trachea, and bronchi. Rans Pathol Soc London. 1857; 8:88.
2. Zhu Y, Wu N, Huang HD, Dong YC, Sun QY, Zhang W, et al. A clinical study of tracheobronchopathia osteochondroplastica: findings from a large Chinese cohort. PLoS One. 2014; 9:e102068.

3. Hussain K, Gilbert S. Tracheopathia osteochondro plastica. Clin Med Res. 2003; 1:239–242.
4. Prakash UB. Tracheobronchopathia osteochondro plastica. Semin Respir Crit Care Med. 2002; 23:167–175.
5. Chroneou A, Zias N, Gonzalez AV, Beamis JF Jr. Tracheobronchopathia osteochondroplastica. An underrecognized entity? Monaldi Arch Chest Dis. 2008; 69:65–69.

6. Magro P, Garand G, Cattier B, Renjard L, Marquette CH, Diot P. Association of tracheobronchopathia osteochondroplastica and ozène. Rev Mal Respir. 2007; 24:883–887.
7. Leske V, Lazor R, Coetmeur D, Crestani B, Chatté G, Cordier JF. Groupe d'Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM“O”P).Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine (Baltimore). 2001; 80:378–390.
8. Virchow R. Die krankhaften Geschwülste. 1st ed. Berlin Hirschwald 1863;442p.
9. Aschoff-Freiburg L. Ueber Tracheopathia Osteoplastica. Verh Dtsch Gesch Pathol. 1910; 14:125–127.
10. Clee MD, Anderson JM, Johnston RN. Clinical aspects of tracheobronchopathia osteochondroplastica. Br J Dis Chest. 1983; 77:308–314.

11. Nienhuis DM, Prakash UB, Edell ES. Tracheobronchopathia osteochondroplastica. Ann Otol Rhinol Laryngol. 1990; 99:689–694.

12. White BD, Kong A, Khoo E, Southcott AM. Computed tomography diagnosis of tracheobronchopathia osteochondroplastica. Australas Radiol. 2005; 49:319–321.

13. Manning JE, Goldin JG, Shpiner RB, Aberle DR. Case report: tracheobronchopathia osteochon droplastica. Clin Radiol. 1998; 53:302–309.
14. Magnusson P, Rotemark G. Tracheobronchopathia osteochondroplastica. Three case reports. J Laryngol Otol. 1974; 88:159–164.
15. Tukiainen H, Torkko M, Terho EO. Lung function in patients with tracheobronchopathia osteochondroplastica. Eur Respir J. 1988; 1:632–635.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download