Abstract
Objectives
The purpose of this study was to compare antibiotic resistance patterns between first urinary tract infection (UTI) and recurrent UTI groups and to obtain information regarding empirical antibiotic selection for treating recurrent UTI.
Methods
We retrospectively reviewed 148 children treated for UTIs from January 2009 to June 2016. The patients were divided into two groups: first UTI (N = 148) and recurrent UTI (17 patients and 20 episodes).
Results
In both groups, Escherichia coli was the most frequent causative organism, accounting for 89.9% and 75.0% in the first and recurrent UTI groups, respectively. When E. coli or Klebsiella pneumoniae was the causative organism, extended-spectrum β-lactamase (ESBL)-producing organisms were more frequent in the recurrent UTI group (17.6%) than in the first UTI group (14.0%); however, this difference was not statistically significant (P = 0.684). Cefotaxime was the most frequently used first-line empirical antibiotic in both groups. In the first UTI and recurrent UTI groups, 7.4% and 15.0% of patients were treated with intravenous antibiotics as definitive therapy, respectively (P = 0.250). Fifteen out of 17 patients having a second UTI had different causative organisms or antibiotic susceptibility patterns compared to their previous episode.
Conclusions
Escherichia coli was the most frequent causative organism in the recurrent UTI group. There were no differences in the proportion of ESBL-producing organisms between the first UTI and recurrent UTI groups. Therefore, when a UTI recurs in children, the antibiotics effective on the most common causative organism might be administered as empirical antibiotics.
Urinary tract infection is a common bacterial infection disease in children and is known to occur in 1% of boys and 1–3% of girls.1 It is important for UTI patients to make early diagnoses and to use appropriate antibiotics, as a UTI may lead to renal scarring, hypertension and end-stage renal diseases if contracted in infancy and not properly treated.2 The most frequent causative organism in children is Escherichia coli.3 For children with a UTI, Cefotaxime, Ceftriaxone or Ampicillin and Aminoglycoside combination are used as a first-line drug.1
According to a study, the incidence of UTI recurrence within 3 years in infants aged less than 1 year who suffered from a UTI was 35% in boys and 32% in girls.4 Recurrence of a UTI can be divided into recurrence by the same bacteria and reinfection by other bacteria.5 When choosing empirical antibiotics in cases of reinfection, one of the main concerns is whether to use the first-line drugs used in treating the first UTI or to use drugs susceptible to the bacteria that previously caused the UTI; however, there have been few studies on the selection of appropriate antibiotics for a recurrent UTI. In addition, if a UTI recurs in patients with a previous history of being treated with antibiotics for UTI, it raises the question of whether the possibility that bacteria resistant to the previously used antibiotics caused the recurrence should be considered; however, there have also been few studies on this issue.
The aim of this study was to identify the types of causative organisms, their antibiotic susceptibility and clinical characteristics in the cases of recurrent UTI patients and to compare them with those observed in the cases of first UTI patients in order to obtain base data that can aid in the selection of empirical antibiotics for patients who come to hospitals with a recurrent UTI.
The study retrospectively investigated 168 cases of UTI occurring in 148 pediatric patients who were admitted to the Department of Pediatrics of Kosin University Gospel Hospital from January 1, 2009 to June 30, 2016. 148 cases of first UTI, 17 cases of second UTI and 3 cases of third UTI were included in the study. The patients who had no previous history of UTI and were first diagnosed with UTI were defined as the first UTI group; while the patients admitted with a second and third UTI were defined as the recurrent UTI group. Then the 20 cases of infection that occurred in the 17 patients in the recurrent UTI group were analyzed. All the patients in this group had been diagnosed and treated in this hospital, which enabled the review of their medical records.
This study was reviewed and approved (2016-06-047) by the Institutional Review Board (IRB) of Kosin University Gospel Hospital.
The study looked into the sex, age, and imaging examination findings of the patients in the first and recurrent UTI groups. The medical agents used as empirical antibiotics before the identification of the causative organisms and their antibiotic susceptibility were also investigated, and then the antibiotics selected as definitive therapy were identified. Afterwards, the study compared the types of causative organisms, their antibiotic susceptibility and the production of extended-spectrum β-lactamase (ESBL) that degrades third-generation Cephalosporin antimicrobials in the cases of both the first and recurrent UTI groups.
Among patients who visited the hospital with fever as their major complaint, those who were found to have pyuria and more than 50,000 CFU/mL of a single type of bacterium in their urine through urinalysis tests and urine culture tests respectively were included in the study subjects.6 To obtain the samples for the urine cultures, mid-stream urine was collected from patients who could control their bladders and catheterization was carried out for the patients who could not control their bladders. Cases that were clinically suspected as UTI but for which no bacterium was identified in the urine cultures or the sizes of bacterial colonies were smaller than the diagnostic criteria were excluded from the study. Of the recurrent UTI group, even patients who had come to the hospital due to a second or third UTI, if the relapses were suspected to have been caused by the same bacteria as in the previous UTI within two weeks of the completion of antibiotic treatment, were also excluded from the study.
As automation equipment to identify causative organisms and their antibiotic susceptibility, the research institution used the Phoenix 100 system (BD Diagnostics, Sparks, USA) as main equipment and the Vitek 1 system (bioMérieux, Marcy l'Etoile, France) as supplementary equipment from 1999 to 2012, and since 2012, the Phoenix 100 system has been mainly used and the Vitek 2 system (bioMérieux, Marcy l'Etoile, France) has been used as a supplement.
The research institution has selected Cefotaxime or Ampicillin or Aminoglycoside combination as an empirical antibiotic when patients with UTI were hospitalized.1 When the results of tests on the causative organisms' susceptibility to antibiotics were identified, the antibiotic was replaced by the drug to which the organisms were found to be susceptible.6 If the organisms were susceptible to oral antibiotics, the patients were discharged with oral medications. When the organisms were those producing ESBL and were resistant to all oral antibiotics, injections to which the organisms were susceptible were used during the hospitalization periods. The total duration of treatment was 7 to 14 days, including the duration of both oral and intravenous antibiotic treatments.6 Of patients who were admitted to the hospital with a UTI, for those who had a UTI before, the causative organisms and their antibiotic susceptibility in the previous infections were checked to select appropriate antibiotics according to the conditions, and the one mainly used was Cefotaxime.
According to the American Academy of Pediatrics guidelines, renal urinary tract ultrasonography was performed for first UTI patients. Voiding cystourethrography was conducted on patients with a UTI who showed abnormal findings suggesting a high-grade vesicoureteral reflux or recurrence in the ultrasonography.6 Tc-99m-dimercaptosuccinic acid (DMSA) scans were performed on all first UTI patients until February 2013 in accordance with the American Academy of Pediatrics guidelines7; since, they have been carried out only when patients had vesicoureteral reflux.8 Tc-99m-mercaptoacetyltriglycine (MAG3) scans were carried out when patients had no vesicoureteral reflux but hydronephrosis and when obstruction was suspected in the ultrasonography (the anteroposterior diameter of the renal pelvis > 10 mm).9 The diagnoses of hydronephrosis by ultrasonography were based on Index 10 of the Society of Fetal Urology's grading system10 and an anteroposterior diameter of the renal pelvis greater than 7 mm was defined as a significant abnormal finding.11 Vesicoureteral reflux was classified into grades I-V in the patients who underwent voiding cystourethrography.12 The patients who received DMSA scans were examined to find whether they had renal cortical defects. Using MAG3 scans, whether the patients had had ureteropelvic junction obstructions or renal hypofunction was investigated.
For this study, the SPSS software package (version 23.0; SPSS Inc., Chicago, IL, USA) was used as the statistical analysis program. The Chi-square test was used to compare sexes, ESBL-producing intestinal bacterial ratios, antibiotic resistance rates and oral antibiotic use rates in the first and recurrent UTI groups. Fisher's exact test was used when the expected frequencies were less than 5. P < 0.05 was defined as the significant level.
There were more males than females in both the first UTI group (71.6%, 106/148) and the recurrent UTI group (80.0%, 16/20). The average age was 0.8 in the first UTI group (minimum: 21 days, maximum: 12.8 years), and 1.0 in the recurrent UTI group (minimum: 52 days, maximum: 6.2 years). UTI recurred for 11.5% (17/148) of the patients who were diagnosed with the first UTI in this hospital.
Renal and urinary tract ultrasonography was performed in 95.2% (141/148) of the first UTI group and in 75.0% (15/20) of the recurrent UTI group. Malfunctions such as hydronephrosis, ureterocele and polycystic kidney diseases were detected in 8.5 % (12/141) of the first UTI group and in 26.7% (4/15) of the recurrent UTI group. DMSA scans were carried out in 45.3% (67/148) and 20.0% (4/20) of the first UTI and the recurrent UTI groups, respectively, and renal cortical defects were found in 23.9% (16/67) and 75.0% (3/4), respectively. Voiding cystourethrography was performed in 25.7% (38/148) and 75.0% (15/20) of the first UTI and recurrent UTI groups, respectively, and vesicoureteral reflux was identified in 26.3% (10/38) and 40.0% (6/15), respectively. MAG3 scans were performed and malfunctions were detected in 85.7% (6/7) and 0.0% (0/2) of the first UTI and recurrent UTI groups, respectively.
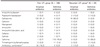
In both the groups, E. coli was the most frequent causative organism, accounting for 89.9% (133/148) and 75.0% (15/20) in the first and recurrent UTI groups, respectively (Table 1). The second most frequent causative organism was Klebsiella pneumoniae in the first UTI group, K. pneumoniae and Enterococcus faecalis in the recurrent UTI group. When both groups are combined, E. coli was the most frequent causative organism, accounting for 88.1% (148/168) and K. pneumoniae 7.1% (12/168) was the second most frequent causative organism; the two organisms accounted for 95.2% of the entire causative organisms of UTI.
For the 17 patients who had a UTI two or more times, identified causative organisms and the occurrence interval are specified in Table 2. Among the 17 patients hospitalized for a second UTI, 3 patients (17.6%) showed a difference in causative organisms between the first and second infections. Twelve patients (85.7%) out of the 14 who had the same causative organisms in the first and second infections were confirmed to show different antibiotic susceptibility patterns even though the names of the organisms were identical. Two out of the three patients hospitalized for a third UTI had causative organisms different from the previous ones, and the remaining one patient who had the same causative organisms showed a different antibiotic susceptibility pattern.
The interval period between the first and second infections fell between the 11th and 414th days after the first antibiotic treatment was terminated, while the interval period between the second and third infections fell between the 20th and 77th days after the second antibiotic treatment was terminated. The patients who had a second occurrence of UTI on the 11th day after the first antibiotics treatment was terminated were found to have different causative organisms in the first (E. coli) and the second (faecalis).
When E. coli or Klebsiella pneumoniae was the causative organism, ESBL-producing organisms accounted for 17.6% (3/17) and 14.0% (20/143) in the first and recurrent UTI groups, respectively; however, this difference was not statistically significant (P = 0.684) (Table 3). In terms of each causative organism, ESBL-producing organisms were produced by 14.2% (21/148) of the total E. coli and by 16.7% (2/12) of the total K. pneumoniae. And in the first and recurrent UTI groups, 45.0% (9/20) and 33.3% (1/3) were confirmed to have the ESBL-producing organisms resistant to trimethoprim/sulfamethoxazole.
When E. coli was the causative organism, the resistance rates to piperacillin/tazobactam in both the first and recurrent UTI groups were 5.3% (7/132) and 6.7% (1/15), respectively (P = 0.825) (Table 4). There were no patients with resistance to Carbapenem in either the first or the recurrent UTI groups of E. coli and K. pneumoniae.
The antibiotic that was selected in most cases was Cefotaxime: 81.1% (120/148) and 80.0% (16/20) in the first and recurrent UTI groups, respectively (Table 5).
After confirming the antibiotic susceptibility results, the third-generation Cephalosporin, Cefixime, was the most commonly used antibiotic, so 78.4% (116/148) of the first group and 65.0% (13/20) of the recurrent group were discharged with this antibiotic prescribed. The second most commonly used definitive antibiotics were oral trimethoprim/sulfamethoxazole in the first group and trimethoprim/ sulfamethoxazole and piperacillin/tazobactam in the recurrent group. Patients who were treated with intravenous antibiotics for the entire treatment period as there was no susceptible oral medication accounted for 7.4% (11/148) in the first UTI group and 15.0% (3/20) in the recurrent UTI group. So the rate of such patients was higher than in the latter group, but the difference was not statistically significant (P = 0.250). In the cases in which definitive oral antibiotics were available, Cefixime was used the most in both the groups: 84.6% (116/137) in the first and 76.5% (13/17) in the recurrent groups. Trimethoprim/sulfamethoxazole was the second most used antibiotic: 8.0% (11/137) and 11.8% (2/17) in the first and recurrent groups, respectively.
Nine patients took prophylactic antibiotics after the reflux was confirmed in the first UTI group, and three of them experienced recurrence. Eight of nine patients took Trimethoprim/Sulfamethoxazole as prophylactic antibiotics, and one took Cefaclor.
There were 23 ESBL-producing organisms throughout both the first and recurrent UTI groups. In these cases, Trimethoprim/Sulfamethoxazole was used by 39.1% (9/23), and Piperacillin/Tazobactam by 21.7% (5/23) and Carbapenem by 17.4% (4/23).
To choose adequate empirical antibiotics at the early stage in the event of a UTI recurrence, it is necessary to consider the distribution of causative organisms and the antibiotic susceptibility of the organisms. This study compared the causative organisms, antibiotics used, and the antibiotic susceptibility of the causative organisms in the group of patients with the first UTI and the group of patients with the recurrent UTI, selected from the patients who were hospitalized with a UTI. Among the patients admitted to this institution due to a UTI during the study period, 11.5% (17/148) were readmitted for the recurrence of a UTI, which is similar to the recurrence rate of 13.6% (83/611), reported in the study by Conway et al.13
In this study, UTIs occurred more frequently in boys than in girls in both the first UTI group and the recurrent UTI group. When it comes to the occurrence frequency of UTI in infants under one year, the ratio of boys to girls was 2.8–5.4:1, which shows that boys are more affected by UTIs than girls.1 In this study, infants younger than one year were 89.9% (133/148) in the first UTI group and 80.0% (16/20) in the recurrent UTI group, and the ratio of boys to girls was 3.3:1, meaning that this is consistent with the above-stated study. In particular, UTIs occurred more often in male infants who were not circumcised.1 In this study, however, whether male infants were circumcised or not was not investigated.
E. coli was the most common causative organism of UTIs in both the first and recurrent UTI groups. K. pneumoniae and E. faecalis were the second most common in the recurrent UTI group, but when the two groups were combined, the second most common causative organism was K. pneumoniae. Nuutinen et al. and Kang et al. also reported that E. coli was the most common and K. pneumoniae was the second most common causative organism in their studies, which corresponds to the results of the present study.414
Of the 17 patients in the recurrent UTI group, three (17.6%) had causative organisms different from those of the previous infections. And 12 of the 14 (85.7%) had the same causative organisms in both the first and second infections, but their antibiotic susceptibility patterns were found to have been changed. Therefore, the cases in which the names of the causative organisms and antibiotic susceptibility patterns were identical in both the recurrent and first infections were identified in the remaining two patients (11.8%). In the cases of these two patients, their second infection occurred on the 32nd and 258th day after the termination of the antibiotic treatment for the first infection, respectively, so their cases were considered to have been caused by reinfection.
The rates of ESBL-producing organisms were 14.2% (21/148) in E. coli and 16.7% (2/12) in K. pneumoniae. Among related studies in Korea, the study of Lee et al.15 conducted on E. coli 429 and K. pneumoniae 49 reported that the ESBL-producing organism rates were 6.1% in both organisms, which is lower than the rates confirmed in this study. In addition, the study of Li et al.,16 although it was not conducted on children, found that 12.6% of E. coli and 26.2% of K. pneumoniae were ESBL-producing organisms, similar to the results of this study. The ESBL-producing organisms are generally resistant to antibiotics such as third-generation Cephalosporins that are selected as first-line antibiotic agents for UTIs. Thus, when ESBL-producing organisms are identified, Non-Beta Lactam antibiotics or Carbapenem should be used.17 In this study, the antibiotics that were finally selected as therapeutic antibiotics when ESBL-producing organisms were identified included oral Trimethoprim/Sulfamethoxazole, which were used the most, and injectable Piperacillin/Tazobactam. Piperacillin/Tazobactam is a Beta-Lactam/Beta-Lactam inhibitor, which is known to be effective against UTIs caused by E. coli and K. pneumoniae when susceptible despite the production of ESBLs by organisms.18192021
In the research institution, it has been a treatment principle that patients are discharged early with oral antibiotics prescribed for them when the causative organisms are confirmed to be susceptible to the oral antibiotics and the patients are in good condition as their fever has subsided. There were cases in which the patients were required to be hospitalized for the whole treatment period to enable the use of injectable antibiotics as no susceptible oral antibiotics were found. Such cases were more frequent in the recurrent UTI group, but this increased frequency was not statistically significant. The incidence of ESBL-producing organisms in E. coli and K. pneumoniae was also higher in the recurrent UTI group than in the first UTI group, but the difference was not statistically significant. Park et al.22 reported that although the priorities of the causative organisms were slightly different in the first UTI and recurrent UTI groups, the results were not statistically significant. As a result, they saw that the treatment for a recurrent UTI can be started with the empirical antibiotics used for the first UTI, which corresponds to the results of this study.
This study was a retrospective medical record study conducted in a single institution. There are several limitations to this study. First, the number of cases in the recurrent group was smaller than that of the first group. Also, cases in which the recurrent patients moved to other regions or visited other hospitals were not considered in this study. In addition, the age range of patients is wide and as urine collection methods were not included in medical records for all cases, they were excluded from the analysis. Moreover, when a patient has clinical symptoms, even though more than 10,000 CFU/mL of bacteria were cultured in urine culture test, he or she can be diagnosed with a UTI1; however, in this study, only the patients with more than 50,000 CFU/mL of cultured bacteria were diagnosed with a UTI, which means that there might be patients excluded from the selection of subjects. This was also a limitation of the present study. However, the significance of this study lies in the fact that it confirmed the rates of resistant organisms in children with recurrent UTI, obtaining basic data that can be useful in the selection of appropriate drugs as empirical antibiotics. E. coli was the most common of the causative organisms in children admitted with a recurrent UTI. There was no difference in the rates of ESBL-producing organisms between recurrent UTI patients and first UTI patients. Therefore, when selecting empirical antibiotics for children hospitalized due to recurrent UTI, it is considered as appropriate that the drugs generally target E. coli, which is the most common causative organism.
Figures and Tables
Table 2
Causative organisms and interval since previous infection episode of recurrent UTI group patients

E. coli, Escherichia coli ; E. cloacae, Enterobacter cloacae; K. pneumoniae, Klebsiella pneumoniae; E. faecalis, Enterococcus faecalis ; mo, months; yr, years
*Age refers to the age when we diagnosed first UTI.
†Second and third episode refer to the interval between the last day of treatment of previous infection episode and the first day of present infection episode.
‡Extended-spectrum β-lactamase (ESBL)-producing organism
§Antibiotic resistance pattern changed compared to previous infection episode.
References
1. Elder JS. Urinary tract infections. In : Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier Health Sciences;2015. p. 2556–2562.
2. Roberts KB, Akintemi OB. The epidemiology and clinical presentation of urinary tract infections in children younger than 2 years of age. Pediatr Ann. 1999; 28:644–649.

3. Edlin RS, Shapiro DJ, Hersh AL, Copp HL. Antibiotic resistance patterns of outpatient pediatric urinary tract infections. J Urol. 2013; 190:222–227.

4. Nuutinen M, Uhari M. Recurrence and follow-up after urinary tract infection under the age of 1 year. Pediatr Nephrol. 2001; 16:69–72.

5. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002; 113:5S–13S.

6. Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management. Roberts KB. Urinary tract infection : clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011; 128:595–610.

7. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Urinary Tract Infection. Pediatrics. 1999; 103:843–852.
8. Temiz Y, Tarcan T, Onol FF, Alpay H, Simşek F. The Efficacy of Tc99m dimercaptosuccinic acid (Tc-DMSA) scintigraphy and ultrasonography in detecting renal scars in children with primary vesicoureteral reflux (VUR). Int Urol Nephrol. 2006; 38:149–152.

9. Dudley JA, Haworth JM, McGraw ME, Frank JD, Tizard EJ. Clinical relevance and implications of antenatal hydronephrosis. Arch Dis Child Fetal Neonatal Ed. 1997; 76:F31–F34.

10. Fernbach SK, Maizels M, Conway JJ. Ultrasound grading of hydronephrosis: Introduction to the system used by the society for fetal urology. Pediatr Radiol. 1993; 23:478–480.

11. Lidefelt KJ, Ek S, Mihocsa L. Is screening for vesicoureteral reflux mandatory in infants with antenatal renal pelvis dilatation. Acta Paediatr. 2006; 95:1653–1656.

12. Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol. 1985; 15:105–109.

13. Conway PH, Cnaan A, Zaoutis T, Henry BV, Grundmeier RW, Keren R. Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. JAMA. 2007; 298:179–186.
14. Kang YD, Kim NS, Oh SH. Causative organisms of urinary tract infection in children, and their antibiotic susceptibility. Korean J Pediatr. 2004; 47:1065–1071.
15. Lee YK, Lee H, Kim JM, Kang JM, Lee ST, Lee NY, et al. The antibiotic resistance pattern of gram-negative bacteria in children younger than 24 months with a urinary tract infection : a retrospective single-center study over 15 consecutive years. Child Kidney Dis. 2015; 19:148–153.

16. Li XM, Jang SJ, Bae IK, Park G, Kim YS, Shin JH, et al. [Frequency of extended-spectrum β-lactamase (ESBL) and AmpC β-lactamase genes in Escherichia coli and Klebsiella pneumoniae over a three-year period in a university hospital in Korea]. Korean J Lab Med. 2010; 30:616–623.

17. Megged O. Extended-spectrum β-lactamase-producing bacteria causing community-acquired urinary tract infections in children. Pediatr Nephrol. 2014; 29:1583–1587.

18. Gavin PJ, Suseno MT, Thomson RB Jr, Gaydos JM, Pierson CL, Halstead DC, et al. Clinical correlation of the CLSI susceptibility breakpoint for piperacillin-tazobactam against extended-spectrum-β-lactamase-producing Escherichia coli and Klebsiella species. Antimicrob Agents Chemother. 2006; 50:2244–2247.

19. Peterson LR. Antibiotic policy and prescribing strategies for therapy of extended- spectrum β-lactamase-producing Enterobacteriaceae: the role of piperacillin-tazobactam. Clin Microbiol Infect. 2008; 14:181–184.

20. Rodríguez-Baño J, Navarro MD, Retamar P, Picón E, Pascual Á. Extended-Spectrum Beta-Lactamases–Red Española de Investigación en Patología Infecciosa/Grupo de Estudio de Infección Hospitalaria Group. β-Lactam/β-lactam inhibitor combinations for the treatment of bacteremia due to extended-spectrum β-lactamase-producing Escherichia coli: a post hoc analysis of prospective cohorts. Clin Infect Dis. 2012; 54:167–174.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download