I. Introduction
Maxillofacial surgical procedures require special attention to patient airways, especially because the airway space must be shared by the surgeons and the anesthetist throughout the procedure. General anesthesia (GA) with endotracheal intubation is the most common technique in maxillofacial surgeries. However, this technique exposes patients to the stress of being awake during airway manipulation, as well as to potential postoperative complications from GA. All the risks associated with a difficult intubation and GA are avoidable if surgery is performed under regional anesthesia.
Previously, regional anesthesia has been successfully used for various minor oral surgical procedures; currently it has gained popularity for use among patients with inherent risks for GA. Reports have described successful temporomandibular joint (TMJ) surgeries being carried out under regional anesthesia
1. The aim of this article is to assess the effectiveness of managing isolated mandibular fracture patients under regional anesthesia on an outpatient basis.
The mandible is the most commonly fractured bone in the facial skeleton
2 and mandible fractures are twice as common as mid-face fractures
3. Proper functioning of the mandible is essential for speech and mastication. Mandibular fractures can sometimes also result in facial contour defects. Because of action by the supra-hyoid and masticatory muscles, fracture fragments are often displaced. Mandibular fracture patients also present with acute trismus due to pain, muscle spasm, or mechanical obstruction of the overriding fracture segments.
Because of the complex anatomy and multifarious complications
4 associated with mandibular fractures ranging from hematoma, irreversible nerve injury, non-union, mal-union, and TMJ disorders, to life threatening complications like infection and osteomyelitis, it is imperative that surgeons intervene early.
Currently, open reduction and internal fixation (ORIF) using mini-plates via a transoral approach is the most frequently performed treatment modality
5 for mandibular fractures because it allows early restoration of jaw function and obviates the need for extended periods of maxillomandibular fixation (MMF), which is troublesome for patients.
II. Materials and Methods
Herein, we review 23 patients who had isolated mandibular fractures reporting to the Department of Oral and Maxillofacial Surgery, Government Dental College and Hospital (Mumbai, India) from January 2, 2016 to November 24, 2016. The objectives were to evaluate: 1) the versatility of regional anesthesia for managing isolated fractures; 2) various intraoral and extraoral surgical approaches that can be carried out under regional anesthesia; 3) ease of surgical site exposure and internal fixation with minimal patient discomfort; and 4) postoperative stability and functional restoration and various complications encountered.
Inclusion criteria:
Exclusion criteria:
Patients with condylar fractures requiring ORIF
Fractures that were more than 2 weeks old
Malunion fractures
Patients with uncontrolled systemic diseases
Patients not willing to consent to the procedure
1. Preoperative procedures
Routine blood examinations, including complete blood count, bleeding time, clotting time, and blood sugar levels were performed for all patients, and complete histories were taken to rule out any active communicable infectious diseases.
We used an orthopantomograph (OPG; Planmeca, Helsinki, Finland) for all radiographs, irrespective of mandibular fracture type. For some individual cases, additional radiographs were taken using cone-beam computed tomography (Planmeca Romexis; Planmeca) of the following views: mandibular occlusal view, mandibular lateral oblique view, and mandibular posteroanterior view.
Tetanus toxoid 0.5 mL (Tetanus Toxoid [adsorbed]; Serum Institute of India, Pune, India) was administered intramuscularly for patients who had not received a vaccination within the past year. Oral prophylaxis was administered to all patients. Upper and lower Erich arch bars were secured preoperatively to aid peri-surgical occlusion after reducing the fracture fragments until the fixation. Afterward, patients were not routinely placed in MMF, except for those with condylar fractures who were placed in intermaxillary fixation (IMF) for 1 week.
A 20-gauge intravenous (IV) catheter was placed in all patients just before procedure initiation and dextrose normal saline infusion was started at a rate of 150 mL/h and was continued throughout the surgical procedure. Oxygen saturation and heart rate were monitored with a pulse oximeter throughout the procedure.
All patients were preoperatively given IV Augmentin 1.2 g (GlaxoSmithKline, Mumbai, India), IV metronidazole 100 mL, IV diclofenac 75 mg, and IV dexamethasone 8 mg.
2. Operative procedure
All patients were prepared, scrubbed, and draped according to standard aseptic surgical protocols.
A bilateral conventional inferior alveolar nerve block was given with a 1:1 mixture of 2% lignocaine with 1:200,000 adrenalines and 0.5% bupivacaine. In patients with severe trismus and restricted mouth opening, a closed-mouth Akinosi-Vazirani technique was used to achieve bilateral mandibular nerve block.
In addition to nerve blocks, the surgical site was infiltrated with anesthetic solution and extraoral infiltrations were also made at the lower border of the mandible to reduce pain when handling muscular structures for adequate exposure.
3. Reduction and fixation
Among the 23 patients, 21 patients had their fracture site exposed through a standard mandibular vestibular approach. Two patients had extraoral lacerations that allowed exposure of the fracture. No difficulty was encountered in reducing the fracture segments due muscle spasm.
As per AO principle, the dentate segment was fixed first. Twelve patients had a single fracture (5 angle fractures, 7 parasymphysis fractures) and 11 patients had more than one fracture (8 angle+parasymphysis fractures, 1 parasymphysis+sub-condylar fracture; 1 parasymphysis+subcondylar+coronoid fracture, and 1 comminuted angle+body fracture).
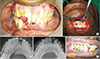
Among the 17 parasymphysis fracture sites, two patients received 2-mm profile, 4-hole titanium mini-plates (Ortho Max mandible plating system; Ortho Max Manufacturing Company, Vadodara, India) with gaps in 15 sites. One patient had a comminuted right parasymphysis fracture that was fixed using a 2-mm profile, 7-hole continuous titanium mini-plate (Ortho Max mandible plating system) at the lower border and a 2-mm profile, 5-hole continuous titanium mini-plate placed 4 to 5 mm above the lower plate.(
Fig. 1) The triangular segment was fixed with a 12-mm long, 2-mm profile titanium screw. In another patient, a single lag screw that was 20-mm long with a 2.5-mm profile was used at the lower border and a 2-mm profile, 4-hole titanium mini-plate with a gap was placed above the lag screw.(
Fig. 2)
Of the 14 angle fracture sites, 13 were fixed with a single upper border plate with a 2-mm profile and 4-hole titanium mini-plate (Ortho Max mandible plating system) with a gap. One angle fracture site was comminuted and was fixed using a 2-mm profile, 2-hole titanium mini-plate with a gap at the upper border and a 2.5-mm profile and 4-hole titanium plate on the lateral surface.(
Fig. 3) While fixing the angle fracture, the most proximal screws were fixed after the release of the MMF for ease of access, as suggested by Ellis and Walker
6. Of 14 angle fracture sites, 4 required removal of the third molar while 3 had a missing third molar, and the remaining 7 third molars were retained.
The surgical sites were closed in layers according to site characteristics and patients were discharged after being observed for 1 hour. Patients were not placed in MMF, except for those with condylar fractures who were placed in IMF for 1 week. Patients were administered Augmentin 625 mg (twice a day), metronidazole 400 mg tab. (three times a day), and diclofenac 50 mg (three times a day) for 5 days with nutrition supplements for 1 month and were advised to maintain strict oral hygiene. All patients had follow-up visits at regular intervals: on the 1st postoperative day, 1st week, 4th week, and 6th week. After 6 weeks, the arch bars were removed and patients were seen 3 months, 6 months, and 1 year after surgery.
III. Results
A total of 23 patients with 32 fracture sites were included in this review; 20 patients were male and 3 were female. Patient ages ranged from 19 to 49 years.
Among the 23 patients, 1 had a left angle and right parasymphysis fracture that was intolerant to the procedure. This patient was given 10 mg of IV Valium (Cipla, Mumbai, India), which did not help to calm the patient. It was then decided to limit treatment to a single mini-plate at the superior border of the angle and a single mini-plate at the parasymphysis.
In general, the reductions and fixations obtained were stable. Recovery was uneventful in all 23 patients with stable reproducible occlusion even after 6 months; this included patients with condylar fractures who were managed with conservative closed reduction. Two patients developed an extraoral draining sinus. One patient was managed with incision and drainage, while the other required hardware removal after 3 months. One alcoholic patient came back with deranged occlusion 1 week after surgery, because the patient fell while intoxicated and was managed with MMF for 6 weeks.
IV. Discussion
All patients in this review underwent ORIF for their mandibular fractures, while condylar fractures were managed conservatively with closed reduction. A simple straightforward method should always be chosen over a tedious complicated one, provided it offers a similar outcome. With respect to fixation methods, rigid fixation was employed in all cases except two parasymphysis and body fractures fixed with 2 mini-plates and an Erich arch bar. All the angle fractures were managed with semi-rigid fixation employing a single upper border mini-plate. Internal fixation methods for multiple mandibular fractures are controversial. Champy et al.
5, in their landmark 1978 article, outlined the ideal approach for osteosynthesis. Many authors, including Ellis and Walker
6, supported the use of a single mini-plate at the upper border for angle fractures
67. Champy et al.
5 stated that placement of a single mini-plate at the upper border in an angle fracture was sufficient for attaining functional stability, irrespective of whether the patient had a single or multiple mandibular fracture. In 2013, Ellis
8 advocated that at least one rigid fixation should be required in multiple fracture cases to reduce complications. Ellis
8 stated that placement of two mini-plates along with an arch bar provided rigid fixation to the fracture segments because it allowed no movement of the fracture site.
All fractures in this study were either single or multiple, except for those with condylar fractures, and all were managed with patients under regional anesthesia.
Although various techniques for inferior alveolar nerve block have been described in the literature
9, a conventional inferior nerve block technique was used for patients in this study, because the operator was fluent with the technique. For patients with severe trismus, a closed-mouth Akinosi-Vazirani technique for mandibular nerve block was employed. Local infiltration over the surgical site and the lower border of the mandible was performed to minimize oozing because the anesthetic contained adrenaline to aid in painless handling of muscular structures. No difficulty was encountered with regard to fracture reduction from muscle spasm.
All patients were successfully managed under regional anesthesia without any intraoperative uncontrolled events, with one exception, which arose from a judgment error in patient selection, who was very apprehensive about the surgical procedure and who had a decreased pain threshold, which prompted us to place a single mini-plate at the upper border of the left angle and a single mini-plate in the parasymphysis region.
Because the majority of mandibular fracture patients present with trismus, which makes preoperative anesthetic assessment difficult
10, the anesthetist must proceed under the assumption that the mouth opening will increase after induction, but this assumption could lead to serious consequences if the anticipated mouth opening is not achieved. To avoid this, the anesthetist may resort to performing awake fiberoptic intubation, which is very unpleasant for patients and also introduces serious complications
11. Associated mid-face fractures can sometimes preclude naso-tracheal intubation.
Following mandibular fracture treatment, mandibular nerve blocks have been frequently used for postoperative analgesia
12. To eliminate the inherent risks associated with GA, regional anesthesia has been successfully used in traumatic maxillofacial cases
13.
The advantage of regional over GA is that the patient is conscious and has control over the musculature that maintains the airway, controls gastric secretions, and aids in condylar positioning. Although condylar sag has not been reported in the literature as a main cause of deranged occlusion following mandibular fracture treatment, it is nevertheless an established causative factor for postoperative malocclusion. Previous studies suggested that patients under GA should be awakened intraoperatively to check the condyle position within the fossa
14. Occlusion is a dynamic relationship that depends on dentoalveolar architecture, TMJ articulation, and masticatory muscles. Thus, it is important to emphasize the role of muscle tone, muscular activity, and proprioception to maintain condylar position, which is not affected by regional anesthesia, and to prevent postoperative malocclusion.
Additionally, regional anesthesia has a clear advantage over GA in that the patient is conscious during the procedure, which can warn the surgeon of impending complications. Under regional anesthesia, patients require less postoperative nursing care and have a shorter recovery time. All our patients were discharged 1 hour after the procedure. Regional anesthesia negates other GA complications, like atelectasis, pulmonary edema, nausea, and vomiting and it provided better pain postoperative relief. Also, regional anesthetic procedures are cheaper, which is particularly important in lower-middle income countries, like India, where the majority of people with maxillofacial trauma are of lower economic status.
Complications are very common when managing mandibular fractures and can occur during any phase of treatment
415. Surprisingly, only two of our 23 patients, accounting for 32 fracture sites, developed infection. The lower infection incidence was due to our emphasis on strict aseptic surgical protocol and because we placed patients on IV antibiotics during their surgery. Of the two patients who experienced infections, one had very poor oral hygiene, which contributed to infection of surgical site, and the other had a contaminated extraoral laceration, which was responsible for the infection.
No incidence of non-union or mal-union was observed in our patients. One patient returned a week later with deranged occlusion due to a fall while intoxicated. Alcohol and maxillofacial trauma have a well-established relationship in the literature
16.
All our patients were prescribed protein and vitamin supplements. By default, oral intake by mandibular fracture patients was reduced, despite the fact that trauma patients have elevated metabolic demands
17, which must be supplemented.
We infer that regional anesthesia is an excellent intraoperative alternative to GA for ORIF for mandibular fractures in selected cases following stringent perioperative protocols.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download