This article has been
cited by other articles in ScienceCentral.
Abstract
Endotracheal intubation is commonly associated with laryngeal injury that often resolves spontaneously without any complication. However, stenosis or granulomatous lesions are generally found on the tracheal wall or vocal process at the tube cuff level, caused by excessive cuff pressure. We present a case of fatal vocal cord granuloma leading to dyspnea following orthognathic surgery and sustained intubation for 14 hours.
Keywords: Granuloma, Intubation, Trauma, Vocal Cord
INTRODUCTION
Laryngeal granuloma is a common late complication of tracheal intubation in adults. Intubation related subglottic granulomas could cause hoarseness of voice, sore throat, lump sensation, and dyspnea [
1]. Vocal process granulomas may arise due to gastroesophageal reflux, vocal abuse, and mechanical trauma such as endotracheal intubation or feeding tube inserted in the throat [
2]. Laryngeal granulomas may be encountered even if the endotracheal tube is maintained for < 24 hours. Pressure necrosis results from trauma by endotracheal tube cuff on the arytenoid cartilage due to high positive pressure [
3]. Granulomas associated with gastroesophageal reflux are usually found in adult males, while 75 to 90% of intubation-related vocal process granulomas are reported in females [
4] because of a narrow glottis, lower glottic proportion, and thinner arytenoid mucochondrium. Granulomas typically affect the posterior aspect of the vocal cords, especially the vocal process of the arytenoids, and the posterior cricoid plate in the subglottic larynx. The treatment of granuloma is excision by microlaryngeal surgery under general anesthesia [
56].
In this report, we describe a case of intubation-related fatal vocal cord granuloma after orthognathic surgery.
CASE
A healthy 29-year-old woman visited the otolaryngology clinic with sore throat and hoarseness that started three months ago, with a history of Le Fort I osteotomy and bilateral sagittal split osteotomy performed three months back in a dental hospital. During induction of general anesthesia for the orthognathic surgery, propofol 80 mg and rocuronium 30 mg were administered, and 10 mg of rocuronium was injected every hour for maintenance. Intubation was done using a cuffed nasotracheal tube (NTT) of 6.5 mm internal diameter in a single attempt with grade 1 Cormack-Lehane view in direct laryngoscopy. Duration of general anesthesia was approximately 4 hours 15 minutes. The NTT was retained postoperatively to avoid the risk of airway swelling and difficulties of airway management. The patient was able to breathe through the NTT and was transferred to the recovery room. The oxygen saturation was 100% and other vital signs were stable. The NTT was removed after a 9-hour postoperative period. During the week of admission, there was a swelling in the left jaw and throat pain without any hoarseness or lump sensation.
The hoarseness developed two weeks after discharge, and three months later, she visited the outpatient clinic with sustained hoarseness and sore throat, and right vocal cord mass was observed in laryngoscopy (
Fig. 1). On the next outpatient clinic visit two months later, the mass became larger and blocked more than half of the airway at the vocal cord level (
Fig. 2). The previous symptoms persisted but there was no dyspnea. The patient was discharged with the expectation that the symptoms would improve; however, she visited the emergency room with throat pain, voice loss, and dyspnea after one week. On arrival at the emergency room, the oxygen saturation was 98%. Atrovent inhalation was administered and the vital signs of the patient were stable. A 1.3 × 1.1 cm sized, well-defined nodular lesion was observed on computed tomography performed in the emergency room, and most of the laryngeal airway was blocked by the vocal cord mass as observed in laryngoscopy (
Fig. 3). Two days after admission, there was no improvement in the symptoms and emergency laryngeal microsurgery was performed.
Under general anesthesia, the patient was placed in the Boyce position, the suspension laryngoscope was placed, and vocal cords were exposed. Hemorrhagic granuloma was observed in the right vocal cord process and the mass was removed using a laser.
The next day, she was discharged without complications. Three months after the granuloma removal, laryngoscopic examination showed no abnormality (
Fig. 4). Additional botox injection was administered to improve the hoarseness.
DISCUSSION
Laryngeal trauma due to an endotracheal tube or NTT could be due to an extremely large-sized tube, abnormal position of the patient's head and larynx, mislocation or overpressure of tube cuff, and extubation trauma, further contributing to granuloma development [
4]. These factors can be prevented by paying precise attention during airway manipulation.
A previous study has reported that female sex, short neck, obesity, and hereditary airway abnormality to be predisposing factors of laryngeal granuloma formation [
7]. The female sex was the only factor in this case report. Additionally, the movements of the vocal cord and trachea are equally important. During spontaneous ventilation, the vocal cords open and close and passively constrict and shorten with each inspiration and expiration. However, with controlled respiration, the tube moves along its longitudinal axis. These movements cause the endotracheal tube to rub against the tracheal surface, and this is observed even with bucking, coughing, swallowing [
7]. Therefore, patients who maintain intubation after orthognathic surgery should be provided adequate sedation to reduce airway irritation.
In another case, it was reported that the cause of laryngeal granuloma is traumatic intubation, related to the trauma and ischemia in the tracheal wall due to high pressure of a large-diameter tube or cuff [
8]. It has been reported that granuloma formation prevalence is as high as 76% in patients intubated for > three days [
9]. On the other hand, another case reported that the granuloma developed even though the intubation lasted only for 105 minutes [
10]. Although our patient was intubated for 13.5 hours, it is not considered a long period. Therefore, granulomatous formation in this case could be related to the cuff pressure rather than the intubation duration. The oral anatomy of the patient was normal, and intubation was performed easily. The cause of vocal cord granuloma in this case was attributed to the traumatic pressure of the cuff or damage to the vocal process by gag reflex in a state of intubation after surgery, because the patient did not have any underlying medical conditions, smoking habits, or anatomic variations. Furthermore, a 6.5-mm internal diameter NTT was used as per the usual size for Korean women.
The chances of intubation related granuloma can be reduced by monitoring the cuff pressure via a manometer, using the smallest possible diameter tube, avoiding extreme flexion or extension of the neck, and providing adequate muscle relaxation or adequate depth of anesthesia to minimize the patient's movement around the tube. Treatment of intubation related granulomas includes corticosteroids, antibiotics, antacids, strict voice rest, and surgical removal. However, some granulomas are refractory to usual therapies. For these recurrent granulomas, repeated excision may provide resolution [
11]. Many anesthesiologists postulate that hoarseness is a common post-intubation complication; however, hoarseness may be the sign of a growing granuloma. Therefore, patients should be informed of the risk of intubation related granulomas and its symptoms. If patients experience post-intubation hoarseness for > one week, they should be told to visit an outpatient clinic.
Figures and Tables
Fig. 1
Three months postoperatively, the right vocal cord granuloma is observed in outpatient laryngoscopy.

Fig. 2
Granuloma has become larger and blocked more than half of the vocal cord, five months postoperatively.

Fig. 3
On arrival at the emergency room, most of the vocal cord seems to be blocked by the mass (a), with bleeding tendency (b).
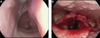
Fig. 4
Laryngeal examination does not reveal any heteroplasia in the vocal cords, three months after granuloma removal surgery.

ACKNOWLEDGEMENTS
This study was supported by 2017 Clinical Research Grant, Pusan National University Dental Hospital.
References
1. Yilmazer C, Sener M, Yilmaz I. Bilateral giant posterior laryngeal granulomas with dyspnea: a rare complication of endotracheal intubation. Anesth Analg. 2005; 101:1881–1882.

2. Yun KI, Lee JA, Park JU. Intubation granuloma: report of a case. J Oral Maxillofac Surg. 2008; 66:1263–1265.

3. Barton RT. Observation on the pathogenesis of laryngeal granuloma due to endotracheal anesthesia. N Engl J Med. 1953; 248:1097–1099.

4. Drosnes DL, Zwillenberg DA. Laryngeal granulomatous polyp after short-term intubation of a child. Ann Otol Rhinol Laryngol. 1990; 99:183–186.

5. Dubick MN, Wright BD. Comparison of laryngeal pathology following long-term oral and nasal endotracheal intubations. Anesth Analg. 1978; 57:663–668.

6. de Lima Pontes PA, De Biase NG, Gadelha EC. Clinical evolution of laryngeal granulomas: treatment and prognosis. Laryngoscope. 1999; 109:289–294.

7. Blanc VF, Tremblay NA. The complications of tracheal intubation: a new classification with a review of the literature. Anesth Analg. 1974; 53:202–213.
8. Barton RT. Medicolegal aspects of intubation granuloma. J Am Med Assoc. 1958; 166:1821–1823.

9. Santos PM, Afrassiabi A, Weymuller EA Jr. Risk factors associated with prolonged intubation and laryngeal injury. Otolaryngol Head Neck Surg. 1994; 111:453–459.

10. Altun D, Yilmaz E, Basaran B, Camci E. Surgical Excision of Postintubation Granuloma Under Jet Ventilation. Turk J Anaesthesiol Reanim. 2014; 42:220–222.

11. Harari PM, Blatchford SJ, Coulthard SW, Cassady JR. Intubation granuloma of the larynx: successful eradication with low-dose radiotherapy. Head Neck. 1991; 13:230–233.











