Abstract
Ramsay Hunt syndrome is a type of acute herpes zoster, which occurs by reactivation of the varicella-zoster virus at the geniculate ganglion. Clinical presentation of Ramsay Hunt syndrome includes a vesicular rash on the ear (herpes zoster oticus) or in the oral mucosa accompanied by acute peripheral facial nerve paralysis. Other cranial nerves such as V, IX, XI, and XII are often involved. Additional variability of the clinical picture of Ramsay Hunt syndrome is produced by varying patterns of skin involvement explained by individual anastomoses between cranial and cervical nerves. Combination treatment containing anti-viral agents and steroids is recommended for the treatment of Ramsay Hunt syndrome. Additionally, early diagnosis of Ramsay Hunt syndrome is a crucial factor to improve damaged nerves in Ramsay Hunt syndrome, which initiates treatment as soon as possible.
After primary exposure to chicken pox, varicella-zoster virus remains for life in the sensory ganglion of the spinal and cranial nerves. The reactivation and replication of varicella-zoster virus leads to herpetic inflammatory lesions from the ganglion to dermatomes associated with the involved ganglion. Therefore, the characteristic symptom of herpes zoster (shingles) is pain and rash in the involved dermatome [12]. In the few cases of herpes zoster, the extension of inflammation from the sensory ganglion to the anterior horn and ventral root results in motor impairment [34].
In 1907, James Ramsay Hunt reported several cases of an erythematous vesicular rash on the auricular area or oral mucosa by reactivation of the varicella-zoster virus in the geniculate ganglion or facial nerve, which is sometimes combined with various neurological disturbances of the cranial nerves [5].
Herpes zoster most frequently involves the thoracic segment in 59.2% of cases. Head and neck occurrence of herpes zoster is reported as accounting for up to 35% of cases [67]. Ramsay Hunt syndrome is one of the most common cases of atraumatic facial paralysis. In a retrospective review of 1507 patients with unilateral facial palsy, 12% (185) of the patients were diagnosed with Ramsay Hunt syndrome based on the clinical presentations such as facial paralysis, ear pain, and herpetic lesions with any cranial dermatome [8]. A retrospective review of 2076 patients with unilateral facial palsy demonstrated that there was no significant difference in terms of the incidence of Ramsay Hunt syndrome between adults and children aged older than 6 years. In this study, Ramsay Hunt syndrome was diagnosed in 16.7% of children and 18.1% of adults with facial palsy [9]. The incidence of Ramsay Hunt syndrome significantly increases in children aged older than 6 years (24.3%), compared to children aged younger than 6 years (10.5%) [8]. However, other studies showed that involvement of the cranial nerve in Ramsay Hunt syndrome increases with age [710]. In a previous study by Robillard et al., it was found that among 185 patients with peripheral facial nerve paresis in herpes zoster oticus, women (18%) were more significantly affected than men (8%) [8]. However, other studies have shown that gender-specific predilection is less clear [1011].
Typical Ramsay Hunt syndrome includes zoster oticus in connection with lower motor neuron facial palsy. Herpes zoster oticus can involve the eardrum, external auditory canal and conchae, antihelix, fossa of the antihelix, incisura intertragica, and lobule, which is called Hunt's zone [1213]. In a review of 91 patients with herpes zoster oticus, 40.6% of patients had an isolated lesion and 25.3% of patients had multiple lesions in both the external ear and external auditory canal [14]. Therefore, due to the variability in erythematous vesicles in Ramsay Hunt syndrome, the external parts of the external auditory canal and eardrum should be examined.
There are complicated anastomoses between cranial nerves including facial, trigeminal, glossopharyngeal, vagal, or cervical nerves, which enable herpetic lesions to progress further. While skin lesions lead to the diagnosis of herpes zoster oticus, various neurological disturbances can occur such as tinnitus, hearing loss, nausea and vomiting, vertigo, and nystagmus [515]. Acute herpetic neuralgia within Hunt's zone may radiate to the face, ear, head, and neck. This neuralgia has a relationship with the sympathetic nervous system. Therefore, pain sometimes induces lacrimation, nasal congestion, and salivation [16].
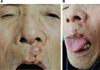
The facial nerve mainly provides motor innervation of facial muscles with a few sensory nerve fibers for conveyance of taste sensation from the anterior two-thirds of the tongue. In patients with Ramsay Hunt syndrome, facial nerve palsy is characterized by facial weakness on the affected side, such as decreased forehead wrinkling, inability to close eye, and drooping corner of the mouth (Fig. 1A). When patients with Ramsay Hunt syndrome are asked to wrinkle their forehead, they cannot form wrinkles on the affected side. If asked to smile or show their teeth, these actions are impossible on the affected side and the upper axis is shifted to the healthy side. In addition, loss of motor control of facial muscles leads to a reduction in the flow of tears and saliva on the affected side. Inability to close the eye leads to excessive dryness of the eye, which can produce ulcerations of cataracts [1517]. The stapedius muscle reduces the vibrations of the stirrup by pulling on the neck of that bone. This muscle is innervated by the nerve to the stapedius, a branch of the facial nerve. Paralysis of the stapedius muscles cannot prevent wider vibration of the stapes, resulting in heightened reaction of the auditory ossicles to sound vibrations. This phenomenon is referred to as hyperacusis: increased sensitivity to noise [15]. Patients with Ramsay Hunt syndrome sometimes show erythematous rashes on the ipsilateral anterior two-thirds of the tongue or on the palate (Fig. 1B). The chorda tympani is a sensory branch of the facial nerve that is involved in taste on the anterior two-thirds of the tongue. This nerve anastomoses with the lingual and maxillary nerves, which contributes to the distribution of herpes zoster oticus lesions. Damage to the chorda tympani leads to taste disturbances in the anterior two-thirds of the affected half of the tongue as well as a reduction of tear, nasal, and saliva secretions. Patients with oral mouth lesions report a burning or numb sensation in the involved mucosal areas [15]. Approximately 50% of patients are expected to be associated with an injury of the vestibulocochlear nerve, cranial nerve XIII. Injury of the vestibular nucleus produces nausea and/or vomiting [14]. Therefore, the herpetic lesion of the vestibular nerve is associated with several side effects including gait insecurity with a tendency to fall to the affected side, vertigo, and spontaneous nystagmus [1819]. Damage of the cochlear component leads to tinnitus and hearing loss [19].
Involvement of the abducens, glossopharyngeal, or vagus nerves rarely occurs in Ramsay Hunt syndrome. Paralysis of the abducens nerve leads to double vision and involvement of the glossopharyngeal nerve, and the vagus nerve is associated with swallowing difficulty or vasovagal reactions, such as cardiac arrhythmia [2021].
Zoster sine herpete is a relatively rare condition with radicular pain in the absence of skin lesions [22]. It can only be diagnosed using serological or polymerase chain reaction assays. Immunoglobulin antibodies specific for acute varicella-zoster virus infection include immunoglobulin A and M. However, these antibodies are detected in approximately 50%–60% of the patients with zoster sine herpete [23]. It was found that Bell's palsy can be associated with varicella-zoster virus. Herpes zoster virus DNA may be detected in patients with Bell's palsy using polymerase chain reaction assays [24]. In addition, it was reported that combined treatment with acyclovir and prednisolone hastened the recovery of Bell's palsy [25].
The diagnosis of Ramsay Hunt syndrome is mainly based on the history, clinical findings, and neurological examination [18]. Analysis of cerebrospinal fluid and brain magnetic resonance imaging has limited value for the diagnosis and prognosis of Ramsay Hunt syndrome. Polymerase chain reaction assays may be useful to detect herpes zoster virus DNA in exudates from ear scrapings, tears, saliva, blood mononuclear cells, or cerebrospinal fluid [23].
Early treatment with a combination of acyclovir and prednisone is reported to be effective to treat Ramsay Hunt syndrome [2526]. Antiviral agents such as acyclovir and famciclovir improve acute pain and recovery of lesions from herpes zoster and prevent the occurrence of postherpetic neuralgia [127]. Steroids have a strong anti-inflammatory action, which reduces inflammation and edema in the nerves involved in herpes zoster, which can lead to accelerated recovery of the affected nerves [4]. The effects of acyclovir–prednisone treatment were investigated in 80 patients with Ramsay Hunt syndrome [12]. In 21 (75%) patients treated within the first 3 days of the onset, complete resolution occurred. However, in 14 (48%) patients treated at 4–7 days and 7 (30%) treated after 7 days of the onset, complete recovery was observed. Additionally, early treatment can improve hearing loss. Acyclovir–prednisone was found to prevent degeneration of nerves with nerve excitability testing and enhance the recovery rate of facial nerve palsy [2526]. There is no statistical difference in the treatment with oral or intravenous acyclovir [18].
Ramsay Hunt syndrome occurs by reactivation of the varicella-zoster virus in the geniculate or facial nerves. Due to anatomical associations with other cranial or cervical spinal nerves, various clinical features can present, such as tinnitus, hearing loss, nausea and vomiting, vertigo, and nystagmus. Combination treatment with anti-viral agents and steroids is recommended for the treatment of Ramsay Hunt syndrome. Additionally, early diagnosis of Ramsay Hunt syndrome is a crucial factor to improve damaged nerves in Ramsay Hunt syndrome, which initiates treatment as soon as possible.
Figures and Tables
References
1. Jeon YH. Herpes Zoster and Postherpetic Neuralgia: Practical Consideration for Prevention and Treatment. Korean J Pain. 2015; 28:177–184.

3. Chernev I, Dado D. Segmental zoster abdominal paresis (zoster pseudohernia): a review of the literature. PM R. 2013; 5:786–790.

4. Kim S, Jeon Y. Treatment of Abdominal Segmental Hernia, Constipation, and Pain Following Herpes Zoster with Paravertebral Block. Pain Physician. 2015; 18:E927–E929.
5. Hunt JR. On herpetic inflammations of the geniculate ganglion: a new syndrome and its complications. J Nerv Ment Dis. 1907; 34:73–96.

7. Nahm FS, Kim SH, Kim HS, Shin JW, Yoo SH, Yoon MH, et al. Survey on the treatment of postherpetic neuralgia in Korea; multicenter study of 1,414 patients. Korean J Pain. 2013; 26:21–26.

8. Robillard RB, Hilsinger RL Jr, Adour KK. Ramsay Hunt facial paralysis: clinical analyses of 185 patients. Otolaryngol Head Neck Surg. 1986; 95:292–297.

9. Hato N, Kisaki H, Honda N, Gyo K, Murakami S, Yanagihara N. Ramsay Hunt syndrome in children. Ann Neurol. 2000; 48:254–256.

10. Ragozzino MW, Meltan LJ, Kurland LT, Chu CP, Perry HO. Population based study of herpes zoster and its sequelae. Medicine (Baltimore). 1982; 61:310–316.
11. Devriese PP, Moesker WH. The natural history of facial paralysis in herpes zoster. Clin Otolaryngol Allied Sci. 1988; 13:289–298.

12. Murakami S, Hato N, Horiuchi J, Honda N, Gyo K, Yanagihara N. Treatment of Ramsay Hunt syndrome with acyclovir-prednisone: Significance of early diagnosis and treatment. Ann Neurol. 1997; 41:353–357.

13. Sweeney CJ, Gilden DH. Ramsay Hunt syndrome. J Neurol Neurosurg Psychiatry. 2001; 71:149–154.
14. Walther LE, Prosowsky K, Walther A, Gudziol H. Untersuchungen zum Zoster oticus. Laryngorhinootologie. 2004; 83:355–362.

16. Nanda A, Khan IS. Nervus intermedius and geniculate neuralgia. World Neurosurg. 2013; 79:651–652.

18. Murakami S, Hato N, Horiuchi J, Honda N, Gyo K, Yanagihara N. Treatment of Ramsay Hunt syndrome with acyclovir-prednisone: significance of early diagnosis and treatment. Ann Neurol. 1997; 41:353–357.

19. Xanthopoulos J, Noussios G, Papaioannides D, Exarchakos G, Assimakopoulos D. Ramsay Hunt syndrome presenting as a cranial polyneuropathy. Acta Otorhinolaryngol Belg. 2002; 56:319–323.
20. Asnis DS, Micic L, Giaccio D. Ramsay Hunt syndrome presenting as a cranial polyneuropathy. Cutis. 1996; 57:421–424.
21. Cheung MY, Viney M. A unique case of recurrent asystole secondary to paroxysmal pain of acute herpetic ophthalmicus. Anesth Analg. 2007; 105:1127–1129.

22. Dayan RR, Peleg R. Herpes zoster - typical and atypical presentations. Postgrad Med. 2017; 129:567–571.

23. Sauerbrei A, Eichhorn U, Schacke M, Wutzler P. Laboratory diagnosis of herpes zoster. J Clin Virol. 1999; 14:31–36.

24. Terada K, Niizuma T, Kawano S, Kataoka N, Akisada T, Orita Y. Detection of varicellazoster virus DNA in peripheral mononuclear cells from patients with Ramsay Hunt syndrome or zoster sine herpete. J Med Virol. 1998; 56:359–363.

25. Furuta Y, Ohtani F, Mesuda Y, Takasu T, Inuyama Y, Nagashima K. Early diagnosis of zoster sine herpete and antiviral therapy for the treatment of facial palsy. Neurology. 2000; 55:708–710.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download