Abstract
Background
Methods
Results
Figures and Tables
Table 1
The nursing practices for controlling healthcare-associated infections in intensive care units nurses (N=210)

Table 2
Individual and organizational characteristics related with nursing practices for control of healthcare-associated infections in participants (N=210)

Table 3
Knowledge of the nursing practices for controlling healthcare-associated infections in intensive care units nurses as individual characteristics

Table 4
Recognition of the nursing practices for controlling healthcare-associated infections in intensive care units nurses as individual characteristics (N=210)

Table 5
Attitude of the nursing practices for controlling healthcare-associated infections in intensive care units nurses as individual characteristics (N=210)

Table 6
Nursing culture of the nursing practices for controlling healthcare-associated infections in intensive care units nurses as organizational characteristics (N=210)

Table 7
Workload burden regarding the nursing practices for controlling healthcare-associated infections in intensive care units nurses as organizational characteristics (N=210)

Table 8
Differences in the nursing practices for controlling healthcare-associated infections in intensive care units nurses (N=210)
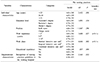
Table 9
Correlation of the nursing practices for controlling healthcare-associated infections in intensive care units nurses as individual and organizational characteristics

*The nursing practices for controlling healthcare-associated infections. †Workload burden due to the nursing practices for controlling healthcare-associated infections. ‡Nursing culture for the nursing practices for controlling healthcare-associated infections. §Attitude of the nursing practices for controlling healthcare-associated infections. ∥Recognition of the nursing practices for controlling healthcare-associated infections. ¶Knowledge of the nursing practices for controlling healthcare-associated infections.
Table 10
Influencing factors on nursing practices associated with the controlling healthcare-associated infections among the nurses working in intensive care units (N=210)

*Knowledge of the nursing practices for controlling healthcare-associated infections. †Recognition of the nursing practices for controlling healthcare-associated infections. ‡Attitude of the nursing practices for controlling healthcare-associated infections. §Nursing culture for the nursing practices for controlling healthcare-associated infections.
Model I: Adjusted R2=.103 (F=5.854, P<.001).
Model II: Adjusted R2=.498 (F=28.663, P<.001).
Model III: Adjusted R2=.561 (F=28.351, P<.001).
References group: Work experience: more than 10 years, Work place: combined intensive care unit.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download