DISCUSSION
In this study, the proportion of patients with LN metastasis was 20.0% for early AEG and 76.1% for advanced AEG. The observed incidence of LN metastasis has been reported to be much higher in patients with AEG than in patients with non-junctional cancer [
8]. Therefore, complete dissection of the LNs is necessary in order to improve the survival outcomes of patients with both early and advanced AEG.
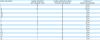
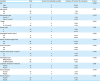
In this study, LN metastasis in stations number 1, 2, 3, and 7 was frequent in both patients with Siewert types II and III AEG. On the other hand, no cases of LN metastasis in station number 4d, 5, or 6 were detected.
In previous studies, the incidence of LN metastasis and the index of estimated benefit from LN dissection (IEBLD) were reported to be higher for LN stations number 1, 2, 3, and 7, and lower (or zero) for LN stations number 4d, 5, and 6, both in patients with Siewert types II and III AEG [
891011]. However, LN metastasis in stations number 4d, 5, and 6 has been reportedly detected in some patients with Siewert type III [
811]. Therefore, caution must be exercised while evaluating patients with AEG showing invasion up to the middle-third of the stomach, because the lower perigastric LNs could be involved, even if the primary tumor epicenter is located within the upper-third of the stomach.
We further investigated the significance of metastasis in LN stations number 3a and 3b separately. The incidence of metastasis in LN station number 3a was higher in both Siewert types II and III AEG. Therefore, radical dissection of the LNs in stations number 1, 2, 3a, and 7 is important in patients with AEG.
On the other hand, the frequency of metastasis in LN station number 3b was relatively low, although not zero, in patients with AEG. Number 3b is the most important LN station while discussing the indications of PG for AEG. However, the LN status of number 3b station in AEG has not yet been investigated in detail.
Four patients in this study had metastasis in number 3b LNs. All patients with number 3b LN metastasis had a gastric invasion length of more than 40 mm, including 1 patient with Siewert type II AEG and a gastric invasion length of 55 mm. The proportion of patients with number 3b LN metastasis in patients with AEG and a gastric invasion length of more than 40 mm was 16.7%, and 1 of 4 patients with number 3b LN metastasis died within 1 year. The prognosis of patients with AEG and number 3b LN metastasis is expected to be worse even after complete LN dissection. However, the number of patients examined in this study was too small to discuss the therapeutic efficacy of number 3b LN dissection. Based on the results of this study, we suppose that the main prognostic factor related to number 3b LN metastasis is not the location of the tumor epicenter, but the lowest level of the tumor.
Although both number 3a and 3b LNs belong to number 3 region along the lesser curvature, number 3a station represents the area along the LGA and number 3b station represents the area along the RGA [
12]. These two arteries are different in terms of embryological origin, with LGA and RGA deriving from the dorsal and ventral mesogastrium, respectively [
13]. Considering the direction of the lymphatic flow, the lymphatics from AEG with a gastric invasion length of less than 40 mm will drain into the proximal lesser curvature nodes (number 3a station), and then to the nodes alongside the root of the LGA (number 7 station) and the celiac trunk (number 9 station), rather than to the nodes along the RGA (number 3b station). This is why number 3b LN metastasis is rare in AEG, despite the high incidence of number 3a and 7 LN metastasis.
Function-preserving gastric cancer surgery, such as PG or pylorus-preserving gastrectomy, is widely practiced for stage I disease [
61415]. Many retrospective studies have shown the functional benefit and oncological safety of function-preserving gastrectomy, which is associated with a lower complication rate and improved postoperative quality of life [
161718]. PG is now regarded as one of the standard procedures for early gastric cancer located in the upper-third of the stomach [
4]. In practice, PG is performed for advanced AEG [
5]. However, the incidence of LN metastasis is higher in AEG than in non-junctional cancer. Therefore, the oncological safety of PG for AEG still remains unclear.
To perform PG for AEG, at least 2 conditions should be satisfied. First, more than one half of the distal stomach should be preserved with an oncological safety margin of at least 2 cm for T1 tumors, 3 cm for T2 or deeper tumors with an expansive growth pattern (types 1 and 2), and 5 cm for those with an infiltrative growth pattern (types 3 and 4) [
4]. Second, no LN metastasis in number 3b station should be detected. In this study, none of the patients with AEG and a gastric invasion length of less than 40 mm had any LN metastases in the number 3b station. Thus, PG may be indicated for patients with AEG with a gastric invasion length of less than 40 mm, if a sufficient distal margin can be obtained while preserving more than half of the stomach. AEG with a gastric invasion length of more than 40 mm would preclude preservation of half of the stomach after PG; therefore, from the viewpoint of function preservation, PG should not be indicated for such cases.
In JGCG 2018 (ver.5), LN dissection of stations number 1, 2, 3, and 7 is recommended for AEGs measuring less than 40 mm in diameter with the lesion center located within 20 mm of the EGJ [
4]. This type of AEG was included in AEG with a gastric invasion length of less than 40 mm and was not associated with number 3b LN metastasis in this study. Thus, the recommended extent of LN dissection might be changed to “Number 1, 2, 3a, and 7 stations” and PG might be indicated for both early and advanced AEGs measuring less than 40 mm in diameter with the lesion center located within 20 mm of the EGJ.
Mine et al. investigated whether gastric invasion length of tumor was related to the distribution of involved abdominal lymph nodes in Siewert type II AEG [
19]. They used Youden Index and determined the cut-off value of gastric invasion length with regard to nodal involvement and found that the length of 43 mm had the largest sum of sensitivity and specificity. Thus, they divided the patients into three groups according to the gastric invasion length (<30, 30–50, and >50 mm). They found that the distribution of involved abdominal LNs in Siewert type II AEG was significantly related to the gastric invasion length of tumor and concluded that PG can be indicated when the gastric invasion length is ≤30 mm. On the other hand, TG should be considered when the gastric invasion length is >50 mm. PG or TG indication was controversial when gastric invasion length was 30–50 mm.
In our study, the cut-off value of gastric invasion length was 40 mm for the following 2 reasons: first, half of the stomach cannot be preserved with sufficient oncological safety margin after PG for AEG with a gastric invasion length of more than 40 mm; second, JGCG prescribes a tumor measuring less than 40 mm in diameter with the lesion center located within 20 mm of the EGJ as junctional cancer. All these AEG types are included in AEG with a gastric invasion length of less than 40 mm. We considered that 40 mm was the most optimal cut-off value to determine the indications of PG for AEG. Therefore, a new cut-off value of gastric invasion length for PG in AEG might be established.
The present retrospective study had some limitations. First, this study was based on the data of a small number of patients. Although the number of patients with AEG is increasing in Japan, LN stations number 3a and 3b began to be investigated separately after the subclassification of number 3 station into these two substations in March 2010 by the JGCG. The number of patients in this study was too small to examine the IEBLD, a concept proposed by Sasako et al. [
20] to assess the efficacy of LN dissection of each LN station. Further large-scale analysis should address this issue. Second, the specimens' size and length were examined after formalin fixation, which may not exactly match clinical measurements. Moreover, these parameters differ among cases and their accurate measurement was difficult because we had no reliable method to evaluate gastric invasion length pre- or intra-operatively. Tumor size and esophageal or gastric invasion length are generally measured by endoscopy with or without endoscopic measurement. Accurate measurement of these parameters is difficult because it is endoscopist-dependent and EGJ is sometimes difficult to detect in large tumors. Therefore, differences between clinical and surgical diagnoses generally arise. However, these parameters can be of help in detecting PG candidates.
In conclusion, radical PG may be indicated for patients with AEG with a gastric invasion length of less than 40 mm who do not require number 3b lymphadenectomy.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download