1. Salvi GE, Cosgarea R, Sculean A. Prevalence and mechanisms of peri-implant diseases. J Dent Res. 2017; 96:31–37.

2. Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015; 42:Suppl 16. S158–S171.

3. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008; 35:Suppl. 286–291.

4. Albrektsson T, Buser D, Chen ST, Cochran D, DeBruyn H, Jemt T, et al. Statements from the Estepona consensus meeting on peri-implantitis, February 2–4, 2012. Clin Implant Dent Relat Res. 2012; 14:781–782.

5. Wade WG. The oral microbiome in health and disease. Pharmacol Res. 2013; 69:137–143.

6. Seymour GJ, Ford PJ, Cullinan MP, Leishman S, Yamazaki K. Relationship between periodontal infections and systemic disease. Clin Microbiol Infect. 2007; 13:Suppl 4. 3–10.

7. Pitts NB, Zero DT, Marsh PD, Ekstrand K, Weintraub JA, Ramos-Gomez F, et al. Dental caries. Nat Rev Dis Primers. 2017; 3:17030.

8. Chenicheri S, R U, Ramachandran R, Thomas V, Wood A. Insight into oral biofilm: primary, secondary and residual caries and phyto-challenged solutions. Open Dent J. 2017; 11:312–333.

9. Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015; 42:Suppl 16. S152–S157.

10. Salvi GE, Ramseier CA. Efficacy of patient-administered mechanical and/or chemical plaque control protocols in the management of peri-implant mucositis. A systematic review. J Clin Periodontol. 2015; 42:Suppl 16. S187–S201.

11. Larsen T, Fiehn NE. Dental biofilm infections - an update. APMIS. 2017; 125:376–384.

12. Lin NJ. Biofilm over teeth and restorations: what do we need to know? Dent Mater. 2017; 33:667–680.

13. Subramani K, Jung RE, Molenberg A, Hammerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009; 24:616–626.
14. Busscher HJ, Rinastiti M, Siswomihardjo W, van der Mei HC. Biofilm formation on dental restorative and implant materials. J Dent Res. 2010; 89:657–665.

15. Song F, Koo H, Ren D. Effects of material properties on bacterial adhesion and biofilm formation. J Dent Res. 2015; 94:1027–1034.

16. Suárez-López Del Amo F, Yu SH, Wang HL. Non-surgical therapy for peri-implant diseases: a systematic review. J Oral Maxillofac Res. 2016; 7:e13.

17. Ferraris S, Spriano S. Antibacterial titanium surfaces for medical implants. Mater Sci Eng C. 2016; 61:965–978.

18. Kreisler M, Kohnen W, Christoffers AB, Götz H, Jansen B, Duschner H, et al.
In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er: YAG laser and an air powder system. Clin Oral Implants Res. 2005; 16:36–43.

19. Schwarz F, Ferrari D, Popovski K, Hartig B, Becker J. Influence of different air-abrasive powders on cell viability at biologically contaminated titanium dental implants surfaces. J Biomed Mater Res B Appl Biomater. 2009; 88:83–91.

20. Sahm N, Becker J, Santel T, Schwarz F. Non-surgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine: a prospective, randomized, controlled clinical study. J Clin Periodontol. 2011; 38:872–878.

21. Albertini M, López-Cerero L, O'Sullivan MG, Chereguini CF, Ballesta S, Ríos V, et al. Assessment of periodontal and opportunistic flora in patients with peri-implantitis. Clin Oral Implants Res. 2015; 26:937–941.

22. Canullo L, Rossetti PH, Penarrocha D. Identification of
Enterococcus faecalis and
Pseudomonas aeruginosa on and in implants in individuals with peri-implant disease: a cross-sectional study. Int J Oral Maxillofac Implants. 2015; 30:583–587.

23. Harris LG, Mead L, Müller-Oberländer E, Richards RG. Bacteria and cell cytocompatibility studies on coated medical grade titanium surfaces. J Biomed Mater Res A. 2006; 78:50–58.

24. Renvert S, Lindahl C, Renvert H, Persson GR. Clinical and microbiological analysis of subjects treated with Brånemark or AstraTech implants: a 7-year follow-up study. Clin Oral Implants Res. 2008; 19:342–347.

25. Mehl C, Kern M, Zimmermann A, Harder S, Huth S, Selhuber-Unkel C. Impact of cleaning procedures on adhesion of living cells to three abutment materials. Int J Oral Maxillofac Implants. 2017; 32:976–984.

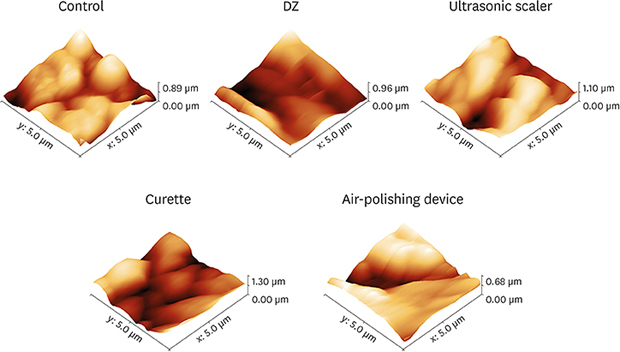
26. Cafiero C, Aglietta M, Iorio-Siciliano V, Salvi GE, Blasi A, Matarasso S. Implant surface roughness alterations induced by different prophylactic procedures: an in vitro study. Clin Oral Implants Res. 2017; 28:e16–20.
27. Chen CJ, Ding SJ, Chen CC. Effects of surface conditions of titanium dental implants on bacterial adhesion. Photomed Laser Surg. 2016; 34:379–388.

28. Ametrano G, D’Antò V, Di Caprio MP, Simeone M, Rengo S, Spagnuolo G. Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on rotary nickel-titanium instruments evaluated using atomic force microscopy. Int Endod J. 2011; 44:203–209.

29. Spagnuolo G, Ametrano G, D’Antò V, Rengo C, Simeone M, Riccitiello F, et al. Effect of autoclaving on the surfaces of TiN-coated and conventional nickel-titanium rotary instruments. Int Endod J. 2012; 45:1148–1155.

30. D'Antò V, Rongo R, Ametrano G, Spagnuolo G, Manzo P, Martina R, et al. Evaluation of surface roughness of orthodontic wires by means of atomic force microscopy. Angle Orthod. 2012; 82:922–928.
31. Rongo R, Ametrano G, Gloria A, Spagnuolo G, Galeotti A, Paduano S, et al. Effects of intraoral aging on surface properties of coated nickel-titanium archwires. Angle Orthod. 2014; 84:665–672.

32. Mandrich L, Cerreta M, Manco G. An engineered version of human PON2 opens the way to understand the role of its post-translational modifications in modulating catalytic activity. PLoS One. 2015; 10:e0144579.

33. Guillemot F, Prima F, Tokarev VN, Belin C, Porté-Durrieu MC, Gloriant T, et al. Ultraviolet laser surface treatment for biomedical applications of β titanium alloys: morphological and structural characterization. Appl Phys, A Mater Sci Process. 2003; 77:899–904.

34. Gallardo-Moreno AM, Pacha-Olivenza MA, Fernández-Calderón MC, Pérez-Giraldo C, Bruque JM, González-Martín ML. Bactericidal behaviour of Ti6Al4V surfaces after exposure to UV-C light. Biomaterials. 2010; 31:5159–5168.

35. Fox SC, Moriarty JD, Kusy RP. The effects of scaling a titanium implant surface with metal and plastic instruments: an
in vitro study. J Periodontol. 1990; 61:485–490.

36. Mengel R, Buns CE, Mengel C, Flores-de-Jacoby L. An in vitro study of the treatment of implant surfaces with different instruments. Int J Oral Maxillofac Implants. 1998; 13:91–96.
37. Hallmon WW, Waldrop TC, Meffert RM, Wade BW. A comparative study of the effects of metallic, nonmetallic, and sonic instrumentation on titanium abutment surfaces. Int J Oral Maxillofac Implants. 1996; 11:96–100.

38. Quirynen M, Bollen CM, Papaioannou W, Van Eldere J, van Steenberghe D. The influence of titanium abutment surface roughness on plaque accumulation and gingivitis: short-term observations. Int J Oral Maxillofac Implants. 1996; 11:169–178.
39. Louropoulou A, Slot DE, Van der Weijden FA. Titanium surface alterations following the use of different mechanical instruments: a systematic review. Clin Oral Implants Res. 2012; 23:643–658.

40. Bennani V, Hwang L, Tawse-Smith A, Dias GJ, Cannon RD. Effect of air-polishing on titanium surfaces, biofilm removal, and biocompatibility: a pilot study. BioMed Res Int. 2015; 2015:491047.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download