Abstract
Early suspicion is essential in diagnosing pyriform sinus cysts. We report two neonatal cases of pyriform sinus cysts presented as neck masses. The first case presented as a right neck mass, which made it more difficult to suspect a pyriform sinus cyst considering the prevalence of left sided cysts. Surgical resection was done in both cases and anatomical investigation suggested both to originate from the fourth branchial pouch. Detection of air bubble containing mass on imaging studies can aid early diagnosis and early use of gastric tube feeding can facilitate treatment by preventing milk contamination which may result in infection of the sinus cyst.
Pyriform sinus cyst is a rare congenital anomaly, which may present as a neck mass. In cases of failure of obliteration of the third or fourth branchial pouch, cysts usually present on the left side. Here, we introduce two cases presented in neonates.
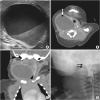
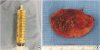
An otherwise healthy girl born at gestation age of 37+6 weeks, birth weight of 3.74 kg, delivered by Cesarean section was referred to our neonatal intensive care unit (NICU) 4 days after birth with swelling and redness of right neck. At birth, skin tag of the right chin was noted. Swelling and redness of the right neck started 2 days after birth. She was fed with normal formula, about 40 mL two to three times per day. She presented with high fever of 39°C and slight inspiratory distress during feeding. Physical examination showed a firm round mass of 4 cm diameter at the anterolateral aspect of right neck. Initial lab results showed nonspecific findings except increased C-reactive protein levels. Initial ultrasound (US) revealed a 3.6×6.5 cm sized elongated cystic mass, medial to carotid space, lateral to trachea, and extending to the retrothyroidal region, containing fluid level and surrounded by an irregular thick wall with minimal soft tissue infiltrates (Fig. 1A). Computed tomography (CT) showed air-bubbles in the nondependent portion of the mass with anterior displacement of trachea and right thyroid gland (Fig. 1B and C). Based on these findings, the mass was suspected to be a complicated anaerobe infected cystic hygroma. Antibiotics therapy were started and needle aspiration was done. Aspirated cystic fluid was yellowish and turbid. Streptococcus viridans was cultured from the fluid (Fig. 2A). Analysis of the fluid showed white blood cell count of 172,800 and low levels of total cholesterol and triglyceride. Feeding was initiated from postoperative 1 day, and size of the cyst started to increase rapidly after needle aspiration, returning to its previous size within two days. Excision of the cyst was done on the 7th day of hospitalization (Fig. 2B). Feeding was reinitiated on postoperative day 1. Pus discharge drained from the neck wound on postoperative 4th day and it contained milk-like substance right after feeding. Esophagography was performed on postoperative day 8, revealing a hairline fistulous communication from the right pyriform sinus to the cyst, suggesting a pyriform sinus fistula due to 4th branchial cleft anomaly (Fig. 1D). Once gastric tube feeding was initiated, size and drainage from the cyst started to decrease. A follow-up esophagography after 15 days demonstrated obliteration of the fistula tract and bottle feeding was started. She was discharged from the hospital after 1 week of bottle feeding, showing no signs of recurrence.
A newborn female infant, gestational age of 39+2 weeks, and 3.46 kg at birth was referred to our NICU due to a 7 cm sized left neck mass presented at birth. No significant medical history during antenatal care was noted. The baby arrived at our NICU 3 hours after birth and physical examination revealed a soft, tense, movable 7 cm long mass without signs of inflammation. Initial neck X-ray showed a 4.7×3.9 cm sized soft tissue density mass at left side of the neck containing round air density (Fig. 3A). With experience of patients with pyriform sinus cysts, gastric tube feeding was initiated from day 1. A sonographic study of the neck mass revealed findings consistent with pyriform sinus cyst, located at the medial side of the left carotid artery and extending to the posterior aspect of the left thyroid gland. The cyst was unilocular and contained isoechogenic debris. Esophagography showed a small tubular opacity from the left pyriform sinus adjacent to the air-filled cyst, suggesting a fistula (Fig. 3B). On neck magnetic resonance imaging (MRI), the fistula was not visualized but a cyst of homogeneous signal intensity without wall thickening or enhancement was visualized with air-fluid level, suggesting communication with the esophagus (Fig. 3C and D). On the 6th day of admission, pyriform sinus cyst resection and fistula ligation was done (Fig. 4). The size of the cyst was 7.0×3.5 cm on operation findings. Histological results of the dissected cyst were negative for malignancy and showed many benign squamous epithelial cells with some multinucleated histiocytes and mixed inflammatory cells. There was no intra-operative complication and the patient recovered uneventfully. Bottle feeding was initiated on postoperative day 7 and the patient was discharged 10 days after surgery.
Pyriform sinus tracts are generally thought to be anomalies arising from remnants of the third or fourth branchial pouch [1]. Third branchial cleft anomalies are proposed to originate from the cranial end of the pyriform sinus, above the superior laryngeal nerve, looping around the hypoglossal nerve, and traveling inferiorly to exit on the lateral aspect of the neck [2]. On the other hand, fourth branchial cleft anomalies are thought to begin at the apex of the pyriform sinus, traveling inferiorly in the tracheoesophageal groove, posterior to the thyroid gland, continuing its inferior course into the thorax and looping around the aorta, then coursing superiorly and looping again around the hypoglossal nerve, exiting at the lateral aspect of the neck [2]. Distinguishing the origin of pyriform sinus tract is difficult both clinically and through imaging studies [3]. The origin can be distinguished only through surgical exploration to determine whether it rises from the third or fourth branchial pouch [3]. Both cases in our study were pyriform sinus cysts originating from the fourth branchial pouch.
Pyriform sinus tracts may be identified at various stages in life with diverse clinical presentations. In a meta-analysis review of fourth branchial arch anomalies by Nicoucar et al. [4], age of onset ranged from neonates to 68 years old and initial presentations included acute suppurative thyroiditis (46%), neck abscess (42%), neck mass, and cutaneous discharging fistula. In the same study, approximately 8.7% (35 cases out of 518 cases), occurred in neonates; and among these cases, 64% had clinical symptoms of respiratory distress [4]. Our first case demonstrated respiratory distress during feeding. CT finding of anterior displacement of trachea by the neck mass may have contributed to the development of such symptom. This demonstrates the need to carefully assess respiratory support needs in neonates who present with pyriform sinus tracts.
We introduced two neonatal cases of pyriform sinus tracts initially presented as neck masses. Neck masses presented since birth or during the neonatal period are usually benign and developmental [5]. Differential diagnoses to consider in such cases include thyroglossal duct cysts, branchial cleft cysts, dermoid cysts, cystic hygroma, vascular malformations and hemangiomas [5]. When inflammation is combined, neck abscess, infected cystic hygroma, reactive lymphadenopathy, and infectious lymphadenitis should be considered.
Imaging studies are essential in differentiating neck masses. Imaging studies such as US, CT, and MRI are useful in delineating the characteristics of the mass and the extent of the inflammatory process [6]. However, since pyriform sinus tracts may not be apparent on such imaging modalities, the diagnosis can easily be overlooked without suspicion of pyriform sinus tracts. Barium study or direct laryngoscopy should be performed for evaluation of pyriform sinus tracts. Barium study is recommended after the inflammation has subsided [1]. Yet, negative finding on barium swallowing test does not completely rule out the possibility of a tract [1].
Air bubbles in the inflammatory cavity of pyriform sinus tract may be due to production of air-forming bacilli or inhaled air from opening of pyriform sinus tracts [6]. These air bubbles may be noted on US, CT or MRI findings, and also on close observation of initial plain X-rays. In our first case, air bubble was not found on US but was visualized on the neck CT. At first, we assumed it to be air-fluid level within an abscess formed by anaerobic bacterial infection and treatment was targeted toward infection based on the assumption of complicated infected cystic hygroma. Earlier acknowledgement of the possibility of air inflow from an open sinus tract would have accelerated the process of correct diagnosis.
Right sided pyriform sinus tracts are very rare, composing only 6% of cases of fourth branchial arch anomalies [4]. Two studies in Korea reported the incidences of pyriform sinus fistula in single institutions; a 9-year-review of 30 patients with pyriform sinus fistula included only one right sided pyriform sinus case [7] and a 13-year-review of 15 patients with pyriform sinus fistula reported two right sided cases [8]. This scarcity makes it even more difficult to correctly diagnose right sided pyriform sinus tracts, as presented in our first case. High levels of suspicion in part of the pediatrician or surgeon is necessary to diagnose and treat pyriform sinus tracts.
Regarding management of fourth branchial arch anomalies, complete excision with open neck surgery or endoscopic cauterization of internal opening is suggested [4]. For cystic anomalies, surgical resection is the treatment of choice and an alternative less invasive method of endoscopic cauterization can be considered. With ongoing inflammation, there is a substantial risk of recurrent laryngeal nerve injury and treatment should be postponed until the inflammation is resolved by adequate incision and drainage and use of antibiotics [4]. For pediatric patients, suggestions are made that complete excision of the entire fistula with a partial thyroidectomy should be delayed until after 8 years of age due to higher risk of complications (e.g., salivary fistula, vocal cord paralysis) in younger children [4]. Endoscopic cauterization requires no open excision and may be performed on an outpatient basis [9]. A study of 10 patients treated with endoscopic cauterization showed no recurrence of a neck mass among the 7 patients who have been followed up for 3 years [9]. However, since cauterization is a relatively novel method, data regarding long-term follow-up and complications need to be assessed.
Regarding chemocauterization, an article published by Yanagisawa et al. [10] in 2017 reviewed 7 studies which used trichloroacetic acid chemocauterization or silver nitrate chemocauterization. Success rate after the initial procedure varied from 0 to 100 percent. Considering studies with more than 10 cases, the initial success rate was 67%–82% and the percentage of cases requiring subsequent chemocauterization was 8%–25%, with 9% eventually requiring surgical treatment. Also, the youngest age reported for chemocauterization was 2 years old with no reported cases of neonatal chemocauterization. Thus, more data and experience are needed to generalize the use of chemocauterization in neonates.
Due to the common recurrence of pyriform sinus cysts, complete excision is essential. However, a few cases of spontaneous closure of pyriform sinus tracts have been reported. In a study of 43 patients with piriform sinus fistula by Miyauchi et al. [11], 62% of patients who refused fistulectomy did not have recurrence during the follow-up period of the study, suggesting that some cases may possibly be treated with conservative care. A study by Wasniewska et al. [12] also demonstrated three cases of spontaneous and definitive closure of pyriform sinus fistulas. In our first case, it is noteworthy how gastric tube feeding facilitated the closure of the pyriform sinus tract which recurred after surgery. Because orally fed formula leaked through the fistula tract and caused repeated infection, gastric tube feeding helped in acquiring the time necessary to treat the inflammation process and facilitated spontaneous closure of the sinus tract.
The scarcity of pyriform sinus tracts, especially presented on the right side, makes it difficult to recognize and misdiagnosis may lead to recurrent episodes of infection as presented in our first case. When neonates present cystic neck masses with air bubble, the possibility of pyriform sinus tract should always be taken into consideration as a differential diagnosis.
ACKNOWLEDGMENTS
We are grateful to Dr. Jooyoung Lee for her valuable insights in editing these cases.
Notes
References
1. Pereira KD, Davies JN. Piriform sinus tracts in children. Arch Otolaryngol Head Neck Surg. 2006; 132:1119–1121.

2. Franciosi JP, Sell LL, Conley SF, Bolender DL. Pyriform sinus malformations: a cadaveric representation. J Pediatr Surg. 2002; 37:533–538.

3. Bar-Ziv J, Slasky BS, Sichel JY, Lieberman A, Katz R. Branchial pouch sinus tract from the piriform fossa causing acute suppurative thyroiditis, neck abscess, or both: CT appearance and the use of air as a contrast agent. AJR Am J Roentgenol. 1996; 167:1569–1572.

4. Nicoucar K, Giger R, Pope HG Jr, Jaecklin T, Dulguerov P. Management of congenital fourth branchial arch anomalies: a review and analysis of published cases. J Pediatr Surg. 2009; 44:1432–1439.

5. Meier JD, Grimmer JF. Evaluation and management of neck masses in children. Am Fam Physician. 2014; 89:353–358.
6. Wang HK, Tiu CM, Chou YH, Chang CY. Imaging studies of pyriform sinus fistula. Pediatr Radiol. 2003; 33:328–333.

7. Kim KH, Sung MW, Lee KJ, Roh JL, Kwon TK, Kim IS, et al. Management of pyriform sinus fistula with chemocauterization. Korean J Otolaryngol-Head Neck Surg. 2002; 45:906–910.
8. Seok JH, Ahn D, Sohn JH, Choi JH, Jung YY, Kong JS. Pyriform sinus fistula: a single center experience. Korean J Otorhinolaryngol-Head Neck Surg. 2013; 56:154–158.

9. Verret DJ, McClay J, Murray A, Biavati M, Brown O. Endoscopic cauterization of fourth branchial cleft sinus tracts. Arch Otolaryngol Head Neck Surg. 2004; 130:465–468.

10. Yanagisawa S, Oshio T, Kato M, Kano M, Tsuji Y, Morikawa Y. Endoscopic chemocauterization for pyriform sinus fistula in children. Pediatr Int. 2017; 59:807–811.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download