Abstract
Purpose
Proliferation marker Ki-67 is widely used in cancer prognosis prediction. We tried to investigate the role of Ki-67 as a prognostic factor in stomach cancer after surgery in this study.
Methods
We retrospectively evaluated 251 patients who underwent curative resection for gastric cancer from 2010 to 2015. In pathologic examination, Ki-67 labeling index was defined as the percentage of Ki-67 antigen positive cells. Prognostic significance of Ki-67 for gastric cancer was evaluated. Disease-free survival (DFS) was assessed as a primary end-point.
Results
The median follow-up period was 28.0 months. Thirty-one patients (12.4%) showed Ki-67 labeling index (LI) lower than 25%. Sixty-eight patients (26.6%) showed recurrence during follow-up period. Recurrence was associated with Ki-67 LI level (≤25%, P = 0.016), and lymph node metastasis status (P = 0.002). High Ki-67 LI level (>25%) was also related to p53 positivity (P < 0.001) and poorly cohesive type (P = 0.002). The 3-year DFS was 69.4%. Low Ki-67 LI level (≤25%) was related with low DFS (47.6% vs. 72.6%, P = 0.016). T stage (P < 0.001), N stage (P = 0.006), lymphovascular invasion (P = 0.010), and neuronal invasion (P = 0.001) also affected the DFS. In addition, T stage (P = 0.03) and Ki-67 LI (P = 0.035) were independent prognostic factors for DFS. In patients treated with adjuvant chemotherapy (n = 239, 93.4%), low Ki-67 (≤25%) was a poor prognostic factor for DFS (P = 0.013).
Ki-67, as a proliferation marker, is used to predict the prognosis of cancer [1] and estimate the response to treatment. Recently, various researches have focused on Ki-67 labeling index (LI) and its role in cancer [1]. Ki-67 LI is defined as the percentage of Ki-67 antigen positive cells. Nuclear protein Ki-67, known as a marker of cellular proliferation, seems to be correlated with cancer survival. The cell cycle is known to affect the status of Ki-67; Ki-67 is present in the G1, G2, S, and M phase, but not in the G0 phase [2]. A previous study by Lazăr et al. [3] has shown that pathologic differentiation and p53 positivity are associated with the Ki-67 LI.
Although stomach cancer incidence has decreased compared to before, it is still considered a major cause of cancer death in East Asia [456]. In stomach cancer, p53 and Ki-67 have been reported to be useful in predicting prognosis [78]. For instance, according to a recent Korean study by Lee et al. [9], high Ki-67 level may be associated with good prognosis. However, this is controversial because several studies [10111213] have shown that high Ki-67 LI is associated with poor prognosis. Wu et al. [10] also reported that low Ki-67 LI was closely related to favorable survival after combined chemotherapy and surgery of gastric cancer. An Italian study additionally showed that high Ki-67 index is correlated with poor prognosis in elderly gastric cancer patients. Huang et al. [13] also showed that high Ki67 expression was associated with shorter survival and high relapse rate. On the one hand, Boger et al. [14] reported that Ki-67 expression did not have any prognostic value in gastric cancer.
The purpose of this study was to determine the significance of Ki-67 LI obtained from postoperative tissue specimens as a predictive marker to estimate the prognosis of stomach cancer. We also tried to find out other clinical/pathologic factors that might affect prognosis and factors related to Ki-67 LI.
We evaluated 251 patients who underwent surgery for locally advanced gastric cancer in Inje University Busan Paik Hospital from February 2010 to August 2015. This study was approved by the Institutional Review Board (IRB) of Busan Paik Hospital (approval number: 17-0070). The IRB waived the requirement for obtaining informed consent. All patients underwent radical surgery for gastric cancer and D2 dissection. Patients were excluded from the study if they had early gastric cancer or distant metastasis at diagnosis. Patients with resection margin involvement were also excluded from this evaluation. Locally advanced gastric cancer, which is considered for postoperative chemotherapy, was the subject of this study. Moreover, if they were followed up for less than 3 months after surgery, or they did not undergo Ki-67 LI examination, they were excluded from the analysis.
In this study, we evaluated the predictive marker for gastric cancer prognosis in the pathologic examination after radical surgery. The primary antibodies used for this evaluation were as follows: Ki-67 (1:280; Dako, Glostrup, Denmark) and p53 (1:150; Dako, Carpinteria, USA). World Health Organization (WHO) classification and American Joint Committee on Cancer 8th staging system were used for tumor classification. Additional examination to investigate the status of p53 or Ki-67 LI was performed for each specimen. Using the monoclonal antibody Ki-67, cellular proliferation rate was quantitatively investigated. In particular, Ki-67 LI was defined as the percentage of immunopositive cells among the counted 100 tumor cells. In the immunohistochemical study, Ki-67 LI was divided into 4 classes:≤25%, 25%–50%, 50–75%, and >75%. Postoperative chemotherapy was administered to most patients.
We assessed disease-free survival (DFS) as a primary end-point. DFS was defined as the time interval between the date of surgery and recurrence. Analyses for failure pattern and prognostic factor were also performed.
For the statistical analysis, IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA) was used. A chi-square test or a Fisher exact test was used for variable comparisons. For survival analysis, Kaplan-Meier and log-rank tests were used. The Cox regression hazard model was used for finding independent prognostic factors for DFS.
The median follow-up period was 28.0 months (range, 3.9–74.6 months). Table 1 summarizes the patient characteristics. The median age of patients was 63 years (range, 26–82 years). Patients aged over 65 accounted for 39.0% (n = 98). According to T stage, T3 was the most common tumor stage observed (n = 113, 45.0%). More than two-thirds of patients (n = 167, 66.5%) had regional lymph node metastases at the time of diagnosis. Moreover, most patients were histologically diagnosed with adenocarcinoma (n = 239, 95.2%). The distribution of Ki-67 LI on pathologic reports was as follows: Ki-67 LI ≤25% in 12.4% of patients, Ki-67 LI 25%–50% in 25.9% of patients, Ki-67 LI 50%–75% in 35.1% of patients, and Ki-67 LI >75% in 26.7% of patients (Table 1). One hundred fifty-one patients (60.2%) were classified as having poorly cohesive carcinoma by the WHO classification. In addition, 168 patients (66.9%) had p53-positive tumors.
For the perioperative treatment, most patients (n = 241, 96.0%) received chemotherapy after surgical resection. Postoperative chemotherapy regimens were mainly 5-fluorouracil (5-FU; n = 44, 17.5%), doxifluridine (n = 124, 49.4%), and S-1 (oral fluoropyrimidine, n = 82, 32.7%), while some patients received multiple types of chemotherapy. No patient underwent neoadjuvant chemotherapy or adjuvant radiotherapy.
Table 2 shows the distribution of clinical/pathologic factors according to Ki-67 value difference. Higher than 25% of Ki-67 LI was associated with poorly cohesive type (P = 0.003) according to WHO classification and p53 positivity (P < 0.001). When the Ki-67 LI value was lower than 25%, there was a tendency of a more diffuse subtype according to the Lauren's classification (P = 0.078).
Regarding the failure pattern, 68 patients (27.1%) showed recurrence. During the follow-up period, 11 patients (4.4%) experienced loco-regional relapse and 59 patients experienced distant relapse (among them, 2 patients showed both loco-regional and distant relapse). Ki-67 LI was related with recurrence (Ki-67 LI ≤25% vs.>25%, P = 0.016) (Table 3). Recurrence was also associated with T stage (P < 0.001) and lymph node metastases at diagnosis (P = 0.002) (Table 3). In addition, lymphovascular invasion (P = 0.008) and neuronal invasion (P < 0.001) were also related with high risk of recurrence (Table 3).
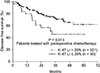
During the follow-up period, 23 patients died. Among them, 20 died because of the progression of gastric cancer, while the others died because of intercurrent disease. According to the survival analyses, the 3-year DFS and overall survival (OS) were calculated as 69.4% and 89.1%, respectively (Fig. 1). The 5-year DFS and OS were estimated as 61.0% and 85.9%, respectively.
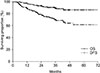
Table 3 shows the results of the univariate analysis for survival. T stage (P < 0.001), N stage (P = 0.006), lymphovascular invasion (P = 0.010), neuronal invasion (P = 0.001), and Ki-67 LI value (≤25% vs. >25%, P = 0.016) affected the DFS. To be specific, Fig. 2 shows that a low Ki-67 value (Ki-67 LI ≤25%) was correlated with low DFS (P = 0.033). Meanwhile, OS was correlated with T stage (P = 0.008), N stage (P = 0.002), and lymphovascular invasion (P = 0.042) (Table 4).
Table 4 demonstrates the results of the multivariate analysis for DFS. T stage (T1–2 vs. T3–4, P = 0.003) and Ki-67 LI (Ki-67 LI ≤25% vs.>25%, P = 0.035) were independent prognostic factors for DFS (Table 5). Additionally, there were no independent prognostic factors for OS.
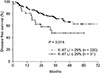
The optimum Ki-67 LI cutoff point, which was obtained to divide the patients according to their prognosis (DFS), was 25% in this study (Fig. 2) (P = 0.033). The other 50% (P = 0.178) or 75% (P = 0.098) cutoff points were inadequate as the relevant Ki-67 LI cutoff values did not produce significant differences. Importantly, among the subgroup who underwent adjuvant chemotherapy (n = 241) after surgery, low Ki-67 LI was related to low DFS (P = 0.013) (Fig. 3).
Subgroup analyses were performed according to p53 positivity and WHO classification, which showed difference of patient distribution by Ki-67 LI (Table 2). In the group without p53 expression, lower Ki-67 LI (≤25%) was correlated with lower DFS (P = 0.031). However, there was no significant DFS difference according to Ki-67 LI in the patient subgroup with p53 positive expression (P = 0.343). In regard to the WHO classification, there were no differences in DFS by Ki-67 LI, though they approached borderline statistical significance (well differentiated P = 0.050 vs. poorly cohesive P = 0.077, respectively).
On the other hand, the further analysis for patient subgroup without lymph nodal metastases (N0) did not show the prognostic effect of Ki-67 expression on DFS (P = 0.312). Even in the analysis for the patients with lymph nodal metastases (N+), the effect of Ki-67 on DFS did not reach the statistical significance (P = 0.072).
Taken together, p53 positivity and the poorly cohesive type were associated with the Ki-67 LI level. In addition, Ki-67 LI affected recurrence and DFS of gastric cancer. In the case of high level of Ki-67 LI with higher proliferation rates, aggressive features, and intratumor heterogeneity, better results were obtained because of the possibility of early detection. That is, high Ki-67 LI tumors may have been easily detected due to mass-forming symptoms [3], because of a relatively less tumor invasiveness and extensive stomach involvement.
The effect of Ki-67 on prognosis may be different according to treatment methods, such as degree of operation or administration of chemotherapy. Our results showed that high Ki-67 level tended to be associated with good prognosis. This result is in contradiction with the findings of previous Western studies, which showed high Ki-67 had detrimental outcomes [111213]. It could be related with the fact that most of the patients of our study received postoperative chemotherapy, whereas most of the European patients did not undergo this adjuvant treatment.
Ki-67 seems to be a useful predictor of chemotherapy response according to the results of our study. In patients treated with chemotherapy, a low Ki-67 level was correlated to a poor DFS in our study. Chemotherapy has been frequently performed as adjuvant therapy after surgery to improve the treatment outcome of gastric cancer in East Asia [151617]. Similarly, in the cases of breast cancer, a high Ki-67 LI value is associated with higher response rate to chemotherapy, as seen in the neoadjuvant treatment arm [1819]. Moreover, Li et al. [20] recently reported that gastroesophageal cancer showed good response to chemotherapy in cases with elevated Ki-67 expression.
As for chemotherapy, 5-FU, which is widely used in adjuvant therapy for gastric cancer, is a proliferation-dependent drug, mainly acting in the G1 and S phases of the cell cycle. Doxifluridine, a fluoropyrimidine derivative of 5-FU, is also widely used as a chemotherapeutic agent in stomach cancer. Biologically, 5-FU is known to inhibit DNA replication by blocking thymidine synthesis [21] which makes it a better anticancer agent for proliferating tumors with high Ki-67 LI. On the other hand, Ki-67 LI levels were associated with radiosensitivity in brain tumors [22] and head and neck cancer [23]. Taken together, Ki-67 LI seems to be associated with chemosensitivity in gastric cancer.
Regional differences may cause different cancer outcomes. Compared to the prognosis in other countries, the prognosis of stomach cancer in Korea seems to be better even with a high Ki-67 LI [24]. According to a previous study [24], Asian patients with stomach cancer have better prognosis than Western patients do, which is thought to be related to differences in biological characteristics and treatment methods. The gastric cancer epidemiology in East Asian countries might be different from that in other countries. In East Asia, stomach cancer occurrence seems to be largely associated with dietary factors, such as salted foods or pickled vegetables [25]. In addition, excessive salt intake can interact with other carcinogens (i.e., Helicobacter pylori) and produce synergic effects.
Our study suggested the cutoff of Ki-67 LI as 25% for DFS. A recent meta-analysis study by Pyo and Kim [26] also shows that Ki-67 LI ≤25% was correlated with worse survival in gastric cancer. However, the optimal cutoff value is still unclear in this field. Therefore, further studies for the optimal cutoff value for Ki-67 LI are still warranted.
As for the limitations, this study was conducted in a limited population of Koreans, by retrospective design. Therefore, selection bias might influence the outcome. The finding that Ki-67 LI showed no effect on OS may be associated with the short-term follow-up period of this study. Moreover, patients were treated with various kinds of chemotherapy drugs. Further studies are needed to establish the direct action mechanism between chemosensitivity and Ki-67 LI. In addition, when we divided the patients using Ki-67 LI, there might be a bias because there was a difference of distribution in p53 positivity or differentiation according to the WHO classification (Table 2) between the 2 groups. Therefore, attention should be paid to the interpretation of the results in that other factors may have affected the outcomes of this study. On the other hand, N stage was not a significant independent prognostic factor for DFS in this study. This indicates that the effect of the N stage on the prognosis might be limited if the lymph node dissection is sufficiently performed and postoperative chemotherapy is given in most cases.
In conclusion, low Ki-67 LI was associated with poor prognosis after gastric cancer surgery. Ki-67 LI seems to be a predictive biomarker of resected stomach cancer treated with adjuvant chemotherapy and can be used for the estimation of adjuvant chemosensitivity. However, further studies should be conducted to determine the exact Ki-67 cutoff value for prognostic prediction in gastric cancer. New predictive biomarkers are still needed to predict therapeutic efficacy and prognosis. Importantly, the identification of the gastric tumor characteristics may be used in the development and selection of effective anticancer drugs.
Figures and Tables
 | Fig. 3Disease-free survival in patients treated with adjuvant chemotherapy according to Ki-67 labeling index (LI). |
ACKNOWLEDGEMENTS
This work was supported by 2016 Inje University Busan Paik Hospital research grant.
References
1. Li LT, Jiang G, Chen Q, Zheng JN. Ki67 is a promising molecular target in the diagnosis of cancer (review). Mol Med Rep. 2015; 11:1566–1572.


2. Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown. J Cell Physiol. 2000; 182:311–322.

3. Lazar D, Taban S, Sporea I, Dema A, Cornianu M, Lazar E, et al. Ki-67 expression in gastric cancer. Results from a prospective study with long-term follow-up. Rom J Morphol Embryol. 2010; 51:655–661.

4. Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017; 49:292–305.



5. Katanoda K, Kamo K, Saika K, Matsuda T, Shibata A, Matsuda A, et al. Short-term projection of cancer incidence in Japan using an age-period interaction model with spline smoothing. Jpn J Clin Oncol. 2014; 44:36–41.


6. Rahman R, Asombang AW, Ibdah JA. Characteristics of gastric cancer in Asia. World J Gastroenterol. 2014; 20:4483–4490.



7. Al-Moundhri MS, Nirmala V, Al-Hadabi I, Al-Mawaly K, Burney I, Al-Nabhani M, et al. The prognostic significance of p53, p27 kip1, p21 waf1, HER-2/neu, and Ki67 proteins expression in gastric cancer: a clinicopathological and immunohistochemical study of 121 Arab patients. J Surg Oncol. 2005; 91:243–252.

8. Tzanakis NE, Peros G, Karakitsos P, Giannopoulos GA, Efstathiou SP, Rallis G, et al. Prognostic significance of p53 and Ki67 proteins expression in Greek gastric cancer patients. Acta Chir Belg. 2009; 109:606–611.


9. Lee HE, Kim MA, Lee BL, Kim WH. Low Ki-67 proliferation index is an indicator of poor prognosis in gastric cancer. J Surg Oncol. 2010; 102:201–206.

10. Wu A, Jia Y, Dong B, Tang L, Liu Y, Du H, et al. Apoptosis and KI 67 index correlate with preoperative chemotherapy efficacy and better predict the survival of gastric cancer patients with combined therapy. Cancer Chemother Pharmacol. 2014; 73:885–893.


11. de Manzoni G, Verlato G, Tomezzoli A, Guglielmi A, Pelosi G, Ricci F, et al. Study on Ki-67 immunoreactivity as a prognostic indicator in patients with advanced gastric cancer. Jpn J Clin Oncol. 1998; 28:534–537.


12. Tsamandas AC, Kardamakis D, Tsiamalos P, Liava A, Tzelepi V, Vassiliou V, et al. The potential role of Bcl-2 expression, apoptosis and cell proliferation (Ki-67 expression) in cases of gastric carcinoma and correlation with classic prognostic factors and patient outcome. Anticancer Res. 2009; 29:703–709.

13. Huang G, Chen S, Wang D, Wang R, Lin L, Chen S, et al. High Ki67 Expression has prognostic value in surgically-resected T3 gastric adenocarcinoma. Clin Lab. 2016; 62:141–153.


14. Boger C, Behrens HM, Rocken C. Ki67--An unsuitable marker of gastric cancer prognosis unmasks intratumoral heterogeneity. J Surg Oncol. 2016; 113:46–54.

15. Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012; 379:315–321.


16. Park SC, Chun HJ. Chemotherapy for advanced gastric cancer: review and update of current practices. Gut Liver. 2013; 7:385–393.



17. Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007; 357:1810–1820.


18. Kontzoglou K, Palla V, Karaolanis G, Karaiskos I, Alexiou I, Pateras I, et al. Correlation between Ki67 and breast cancer prognosis. Oncology. 2013; 84:219–225.


19. Nishimura R, Osako T, Okumura Y, Hayashi M, Arima N. Clinical significance of Ki-67 in neoadjuvant chemotherapy for primary breast cancer as a predictor for chemosensitivity and for prognosis. Breast Cancer. 2010; 17:269–275.


20. Li S, Li B, Wang J, Zhang D, Liu Z, Zhang Z, et al. Identification of sensitivity predictors of neoadjuvant chemotherapy for the treatment of adenocarcinoma of gastroesophageal junction. Oncol Res. 2017; 25:93–97.



21. Longley DB, Harkin DP, Johnston PG. 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003; 3:330–338.

22. Choi Y, Lim DH, Yu JI, Jo K, Nam DH, Seol HJ, et al. Prognostic value of Ki-67 labeling index and postoperative radiotherapy in WHO grade II meningioma. Am J Clin Oncol. 2018; 41:18–23.

23. Freudlsperger C, Freier K, Hoffmann J, Engel M. Ki-67 expression predicts radiosensitivity in oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 2012; 41:965–969.

24. Theuer CP. Asian gastric cancer patients at a southern California comprehensive cancer center are diagnosed with less advanced disease and have superior stage-stratified survival. Am Surg. 2000; 66:821–826.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download