1. Lomboy JR, Coward RM. The Varicocele: clinical presentation, evaluation, and surgical management. Semin Intervent Radiol. 2016; 33:163–169. PMID:
27582602.

2. Thomason AM, Fariss BL. The prevalence of varicoceles in a group of healthy young men. Mil Med. 1979; 144:181–182. PMID:
107487.

3. Cozzolino DJ, Lipshultz LI. Varicocele as a progressive lesion: positive effect of varicocele repair. Hum Reprod Update. 2001; 7:55–58. PMID:
11212075.

4. Dubin L, Amelar RD. Etiologic factors in 1294 consecutive cases of male infertility. Fertil Steril. 1971; 22:469–474. PMID:
4398669.

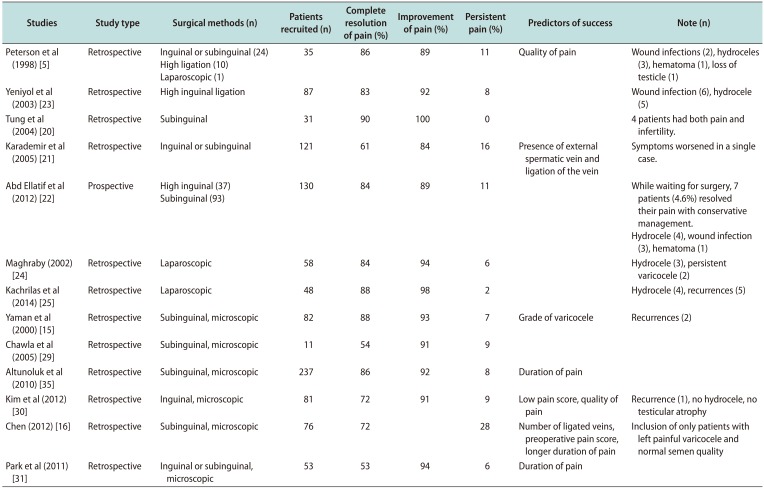
5. Peterson AC, Lance RS, Ruiz HE. Outcomes of varicocele ligation done for pain. J Urol. 1998; 159:1565–1567. PMID:
9554356.

6. Garolla A, Torino M, Miola P, Caretta N, Pizzol D, Menegazzo M, et al. Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Hum Reprod. 2015; 30:1006–1013. PMID:
25779699.

7. Eisenberg ML, Lipshultz LI. Varicocele-induced infertility: newer insights into its pathophysiology. Indian J Urol. 2011; 27:58–64. PMID:
21716891.

8. Hu W, Zhou PH, Zhang XB, Xu CG, Wang W. Roles of adrenomedullin and hypoxia-inducible factor 1 alpha in patients with varicocele. Andrologia. 2015; 47:951–957. PMID:
25335788.

9. Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update. Am J Reprod Immunol. 2008; 59:2–11. PMID:
18154591.
10. Rajfer J, Turner TT, Rivera F, Howards SS, Sikka SC. Inhibition of testicular testosterone biosynthesis following experimental varicocele in rats. Biol Reprod. 1987; 36:933–937. PMID:
3593858.

11. Fujisawa M, Yoshida S, Kojima K, Kamidono S. Biochemical changes in testicular varicocele. Arch Androl. 1989; 22:149–159. PMID:
2665680.

12. Khera M, Lipshultz LI. Evolving approach to the varicocele. Urol Clin North Am. 2008; 35:183–189. viiiPMID:
18423239.

13. Amelar RD, Dubin L. Therapeutic implications of left, right, and bilateral varicocelectomy. Urology. 1987; 30:53–59. PMID:
3603911.

14. Sigalos JT, Pastuszak AW. Chronic orchialgia: epidemiology, diagnosis and evaluation. Transl Androl Urol. 2017; 6:S37–S43. PMID:
28725616.

15. Yaman O, Ozdiler E, Anafarta K, Göğüş O. Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology. 2000; 55:107–108. PMID:
10654904.

16. Chen SS. Factors predicting symptomatic relief by varicocelectomy in patients with normospermia and painful varicocele nonresponsive to conservative treatment. Urology. 2012; 80:585–589. PMID:
22784493.

17. Garg H, Kumar R. An update on the role of medical treatment including antioxidant therapy in varicocele. Asian J Androl. 2016; 18:222–228. PMID:
26763549.

18. Kiliç S, Güneş A, Ipek D, Dusak A, Güneş G, Balbay MD, et al. Effects of micronised purified flavonoid fraction on pain, spermiogram and scrotal color Doppler parameters in patients with painful varicocele. Urol Int. 2005; 74:173–179. PMID:
15756071.

19. Hanley HG, Harrison RG. The nature and surgical treatment of varicocele. Br J Surg. 1962; 50:64–67. PMID:
13904361.

20. Tung MC, Huang WJ, Chen KK. Modified subinguinal varicocelectomy for painful varicocele and varicocele-associated infertility. J Chin Med Assoc. 2004; 67:296–300. PMID:
15366407.
21. Karademir K, Senkul T, Baykal K, Ateş F, Işeri C, Erden D. Evaluation of the role of varicocelectomy including external spermatic vein ligation in patients with scrotal pain. Int J Urol. 2005; 12:484–488. PMID:
15948749.

22. Abd Ellatif ME, Asker W, Abbas A, Negm A, Al-Katary M, El-Kaffas H, et al. Varicocelectomy to treat pain, and predictors of success: a prospective study. Curr Urol. 2012; 6:33–36. PMID:
24917707.

23. Yeniyol CO, Tuna A, Yener H, Zeyrek N, Tilki A. High ligation to treat pain in varicocele. Int Urol Nephrol. 2003; 35:65–68. PMID:
14620287.
24. Maghraby HA. Laparoscopic varicocelectomy for painful varicoceles: merits and outcomes. J Endourol. 2002; 16:107–110. PMID:
11962551.

25. Kachrilas S, Popov E, Bourdoumis A, Akhter W, El Howairis M, Aghaways I, et al. Laparoscopic varicocelectomy in the management of chronic scrotal pain. JSLS. 2014; 18:e2014.00302.

26. Ding H, Tian J, Du W, Zhang L, Wang H, Wang Z. Open non-microsurgical, laparoscopic or open microsurgical varicocelectomy for male infertility: a meta-analysis of randomized controlled trials. BJU Int. 2012; 110:1536–1542. PMID:
22642226.

27. Gontero P, Pretti G, Fontana F, Zitella A, Marchioro G, Frea B. Inguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia: which technique is preferable in clinical practice? Urology. 2005; 66:1075–1079. PMID:
16286127.

28. Guo L, Sun W, Shao G, Song H, Ge N, Zhao S, et al. Outcomes of microscopic subinguinal varicocelectomy with and without the assistance of Doppler ultrasound: a randomized clinical trial. Urology. 2015; 86:922–928. PMID:
26278823.

29. Chawla A, Kulkarni G, Kamal K, Zini A. Microsurgical varicocelectomy for recurrent or persistent varicoceles associated with orchalgia. Urology. 2005; 66:1072–1074. PMID:
16286126.

30. Kim HT, Song PH, Moon KH. Microsurgical ligation for painful varicocele: effectiveness and predictors of pain resolution. Yonsei Med J. 2012; 53:145–150. PMID:
22187245.

31. Park HJ, Lee SS, Park NC. Predictors of pain resolution after varicocelectomy for painful varicocele. Asian J Androl. 2011; 13:754–758. PMID:
21102471.

32. Pastuszak AW, Kumar V, Shah A, Roth DR. Diagnostic and management approaches to pediatric and adolescent varicocele: a survey of pediatric urologists. Urology. 2014; 84:450–455. PMID:
24928462.

33. Pryor JL, Howards SS. Varicocele. Urol Clin North Am. 1987; 14:499–513. PMID:
3303595.

34. Shlansky-Goldberg RD, VanArsdalen KN, Rutter CM, Soulen MC, Haskal ZJ, Baum RA, et al. Percutaneous varicocele embolization versus surgical ligation for the treatment of infertility: changes in seminal parameters and pregnancy outcomes. J Vasc Interv Radiol. 1997; 8:759–767. PMID:
9314365.

35. Altunoluk B, Soylemez H, Efe E, Malkoc O. Duration of preoperative scrotal pain may predict the success of microsurgical varicocelectomy. Int Braz J Urol. 2010; 36:55–59. PMID:
20202236.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download