Abstract
Purpose
The purpose of this study was to identify factors affecting hyperphosphatemia in hemodialysis patients.
Methods
The participants of the study were 129 patients who had been diagnosed with end-stage renal disease and received hemodialysis. Data were collected from June 15 to August 15, 2017, and analyzed with frequency, percentage, average, standard deviation, independent t-test, χ2 test, and logistic regression using SPSS/WIN 24.0 version.
Results
Out of the 129 hemodialysis patients, 71 (55%) had hyperphosphatemia. There were significant differences between healthy group and hyperphosphatemia group in terms of age (p=.048), BMI (Body Mass Index) (p=.004), causative disease of chronic renal failure (p=.026), frequency of hemodialysis per week (p=.024), nutritional status (p<.001), weight gain on maintenance hemodialysis (p=.001), TIBC(Total Iron Binding Capacity) (p=.035), Ca (Calcium) × P (Phosphorus) (p<.001), BUN(Blood Urea Nitrogen) (p<.001), creatine (p=.012), and diet factors of self-care (p=.035). Results of the analysis of factors affecting hyperphosphatemia in hemodialysis patients indicated an increased risk of hyperphosphatemia with diabetes (Odds Ratio [OR]=21.45, 95% Confidence Interval [CI]=1.38~333.47), hypertension (OR=14.41, 95% CI=1.15~180.12), nutritional status (OR=9.37, 95% CI=1.36~64.18), weight gain on maintenance hemodialysis (OR=4.86, 95% CI=1.18~20.05), and BUN (OR=1.07, 95% CI=1.01~1.14).
Conclusion
Based on the results of this study, it is imperative to manage diabetes and hypertension of hemodialysis patients to prevent hyperphosphatemia. Additionally, it is necessary to not only regularly monitor patients' nutritional conditions and results of blood tests, but also develop and provide an individualized nursing intervention that reflects individual nutritional conditions and biochemical results.
Figures and Tables
Table 1
Comparison of General and Hemodialysis Characteristics between Hyperphosphatemia Group and Normal Group among Hemodialysis Patients (N=129)
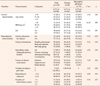
Table 2
Comparison of Nutritional Status between Hyperphosphatemia Group and Normal Group among Hemodialysis Patients (N=129)

Table 3
Comparison of Hematologic Index of Renal Function between Hyperphosphatemia Group and Normal Group among Hemodialysis Patients (N=129)

ACKNOWLEDGEMENT
This article is a condensed form of the first author's master's thesis from Keimyung University.
References
1. Loghman-Adham M. Medication noncompliance in patients with chronic disease: issues in dialysis and renal transplantation. The American Journal of Managed Care. 2003; 9(2):155–171. http://www.researchgate.net/publication/10890033.
2. The Korean Society of Nephrology. 2016 current renal replacement therapy in Korea [Internet]. Seoul: The Korean Society of Nephrology;2016. cited 2016 October 15. Available from: http://www.ksn.or.kr/rang_board/list.html?code=sinchart.
3. Jo YJ, Shin YH. Depression, self care compliance and physiological indices of hemodialysis patients. Keimyung Journal of Nursing Science. 2011; 15(1):115–122.
4. Gutzwiller JP, Schneditz D, Huber AR, Schindler C, Gutzwiller F, Zehnder CE. Estimating phosphate removal in haemodialysis: an additional tool to quantify dialysis dose. Nephrology Dialysis Transplantation. 2002; 17(6):1037–1044. DOI: 10.1093/ndt/17.6.1037.

5. Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. Journal of the American Society of Nephrology. 2004; 15(8):2208–2218. DOI: 10.1097/01.asn.0000133041.27682.a2.

6. Tentori F, Blayney MJ, Albert JM, Gillespie BW, Kerr PG, Bommer J, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the dialysis outcomes and practice patterns study (DOPPS). American Journal of Kidney Diseases. 2008; 52(3):519–530. DOI: 10.1053/j.ajkd.2008.03.020.

7. Arenas MD, Alvarez-Ude F, Gil MT, Moledous A, Malek T, Nuñez C, et al. Implementation of ‘K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease after the introduction of cinacalcet in a population of patients on chronic haemodialysis. Nephrology Dialysis Transplantation. 2007; 22(6):1639–1644. DOI: 10.1093/ndt/gfl840.

8. Min HS, Lee EJ. A study of the relationship between compliance with therapeutic regimens and physiological parameters of hemodialysis patients. Journal of Korean Academy of Nursing. 2006; 36(1):64–73. DOI: 10.4040/jkan.2006.36.1.64.

9. Denhaerynck K, Manhaeve D, Dobbels F, Garzoni D, Nolte C, De Geest S. Prevalence and consequences of nonadherence to hemodialysis regimens. American Journal of Critical Care. 2007; 16(3):222–235.

10. Choi YS. A study on the relationship between perceived social support, and compliance with sick role behavior in elderly hemodialysis patients [master's thesis]. Seoul: Hanyang University;2008.
11. Lee HJ. Nutritional status stress and depression in diabetic hemodialysis patients [master's thesis]. Seoul: Korea University;2015.
12. Lee JH, Kam S, Kim KY, Song MU, Lee EJ, Lee WK. The effect of phosphorus-related nursing intervention on physiologic indicators of hemodialysis patients. Journal of Health Informatics and Statistics. 2016; 41(2):239–247. DOI: 10.21032/jhis.2016.41.2.239.

13. Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson R, et al. What is subjective global assessment of nutritional status? Journal of Parenteral and Enteral Nutrition. 1987; 11(1):8–13. DOI: 10.1177/014860718701100108.

14. Korean Society for Laboratory Medicine. Laboratory medicine. Seoul: Panmun education;2014.
15. Jo MK, Choi MA. Effect of health contract intervention based on king's goal attainment theory on self care behavior and physiological indices of hemodialysis patients. Korean Society of Nursing Science. 2008; 20(10):59.
16. Powers MJ, Baldree KS, Murphy SP. Stress identification and coping patterns in patients on hemodialysis. Nursing Research. 1982; 31(2):107–112. DOI: 10.1097/00006199-198203000-00011.

17. Kim OS, Park SY, Lee MJ, Chang JE, Chung HJ. A study on the correlation between perceived social support and the quality of life of hemodialysis patients [master's thesis]. Seoul: Seoul National University;1993.
18. Chung JH. Management of hyperphosphatemia in chronic kidney disease. The Korean Society of Nephrology. 2006; 25(2):568–575.
19. Guerin AP, London GM, Marchais SJ, Metivier F. Arterial stiffening and vascular calcification in end-stage renal disease. Nephrology Dialysis Transplantation. 2000; 15(7):1014–1021. DOI: 10.1093/ndt/15.7.1014.
20. Kim EM. Diet management of chronic kidney failure and dialysis patients with diabetes kidneys and health. Kidney and Health. 2006; 10:12–15.
21. Chung CS, Lee YK, Choi JS, Lee SM, Song YR, Kim SJ, et al. Pulmonary hypertension in end-stage renal disease patients with maintenance hemodialysis. Korean Journal of Nephrology. 2011; 30(1):48–52.
22. Shin HS, Jung YS, Rim H. The interdialytic weight gain as a nutritional parameter in hemodialysis patients. Kosin Medical Journal. 2006; 21(1):126–133.
23. Yoo HS, Woo HJ, Kang ET, Jo YW. Evaluation of nutritional status and changes of biochemical parameters according to protein intake levels in hemodialysis patients. Korean Journal of Nephrology. 2000; 19(5):769–777.
24. Block GA, Port FK. Re-evaluation of risks associated with hyperphosphatemia and hyperparathyroidism in dialysis patients: recommendations for a change in management. American Journal of Kidney Diseases. 2000; 35(6):1226–1237. DOI: 10.1016/s0272-6386(00)70064-3.

25. Kimmel PL, Varela MP, Peterson RA, Weihs KL, Simmens SJ, Alleyne S. Interdialytic weight gain and survival in hemodialysis patients: effects of duration of ESRD and diabetes mellitus. Kidney International. 2000; 57(3):1141–1151. DOI: 10.1046/j.1523-1755.2000.00941.x.

26. Mutsert R, Grootendorst DC, Boeschoten EW, Brandts H, Van Manen JG, Krediet RT, et al. Subjective global assessment of nutritional status is strongly associated with mortality in chronic dialysis patients. The American Journal of Clinical Nutrition. 2009; 89(3):787–793. DOI: 10.3945/ajcn.2008.26970.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download