INTRODUCTION
In 2017, cancer was the leading cause of death in Korea. The age-standardized rate (ASR) for cancer during this period was 153.9 per 100,000. After cancer, the most common causes of death were cardiac disease, cerebrovascular disease, and pneumonia, with ASRs of 60.2, 44.4, and 37.8, respectively [
1]. During the 12-year period leading up to 2010, the incidence of cervical, endometrial, and ovarian cancer has dynamically changed, becoming similar to patterns found in western countries. However, the ranks of the 3 gynecologic cancers have remained the same. Cancer of the cervix was the most common during this period, with the ASR decreasing from 16.3 to 10.6. Cancers of the ovary ranked second, with the ASR increasing from 5.0 to 5.7, and endometrial cancers ranked third, with the ASR increasing from 2.4 to 6.9 [
2]. During 2018, the estimated incidences for endometrial, ovarian, and cervical cancer in the USA are expected to be 63,230, 22,240, and 13,240, respectively [
3]. The incidence rates and trends of three major gynecologic cancers in Korea, between 1999 and 2015, are being described here.
MATERIALS AND METHODS
The incidence data between 1999 and 2015 were extracted from the Korean National Cancer Incidence Database. The primary subsites were defined based on the International Classification of Diseases, 10th edition [
4]. We defined the 3 main sites of gynecological cancer as the cervix uteri (C53), the endometrium (C54.1), and the ovary (C56).
The ASRs were calculated using the Segi's standard population [
5]. The trends in the incidence rates of gynecological cancer were estimated as an annual percent changes (APCs) by using a joinpoint regression [
6]. The 95% confidence intervals (CIs) were obtained with standard error from the fit of the regression and the t-distribution function.
This study was approved by the Institutional Review Board at the National Cancer Center, Korea (number NCC 2018-0194) and performed according to the principles of the Declaration of Helsinki. The requirement for informed consent was waived.
RESULTS
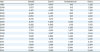
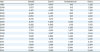
The absolute overall incidence of cervical, ovarian, and endometrial cancer has increased progressively from 6,394 in 1999, to 8,288 in 2015 (
Table 1 and
Fig. 1). However, the absolute number of cervical cancer cases have decreased from 4,443 in 1999 to 3,582 in 2015. The incidences of ovarian, and endometrial cancer have increased from 1,332 in 1999 to 2,443 in 2015, and from 619 in 1999 to 2,263 in 2015, respectively.
Table 1
Number of gynecologic cancer cases by cancer types in the Korea Central Cancer Registry, 1999–2015
|
Year |
Overall |
Cervix |
Endometrium |
Ovary |
|
1999 |
6,394 |
4,443 |
619 |
1,332 |
|
2000 |
6,157 |
4,253 |
615 |
1,289 |
|
2001 |
6,617 |
4,572 |
724 |
1,321 |
|
2002 |
6,632 |
4,402 |
803 |
1,427 |
|
2003 |
6,780 |
4,375 |
925 |
1,480 |
|
2004 |
6,616 |
4,142 |
919 |
1,555 |
|
2005 |
6,797 |
4,029 |
1,093 |
1,675 |
|
2006 |
6,922 |
4,062 |
1,158 |
1,702 |
|
2007 |
6,977 |
3,767 |
1,286 |
1,924 |
|
2008 |
7,374 |
4,015 |
1,477 |
1,882 |
|
2009 |
7,309 |
3,827 |
1,638 |
1,844 |
|
2010 |
7,692 |
3,984 |
1,656 |
2,052 |
|
2011 |
7,638 |
3,791 |
1,792 |
2,055 |
|
2012 |
7,708 |
3,654 |
1,839 |
2,215 |
|
2013 |
7,999 |
3,681 |
2,054 |
2,264 |
|
2014 |
8,080 |
3,553 |
2,090 |
2,437 |
|
2015 |
8,288 |
3,582 |
2,263 |
2,443 |

 | Fig. 1 Age-standardized incidence curve for cervical, endometrial, and ovarian cancer for female patients between 1999 and 2015 in the Korea Central Cancer Registry.
|
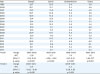
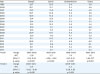
The overall and site-specific ASRs and APCs are shown in
Table 2. The ASR for gynecologic cancer decreased from 23.7 per 100,000 in 1999 to 21.1 in 2015. The APCs during the same period were, −1.36% (95% CI=−2.15, 0.55) between 1999 and 2006 and −0.11% (95% CI=−0.62, −0.42 between 2006 and 2015). The incidence of cervical cancer had decreased from an ASR of 16.3 in 1999 to 9.1 in 2015. The corresponding APC during this period was −3.7% (95% CI=−4.05, −3.40). The incidences of endometrial have been increasing during this period, with the ASR for endometrial cancer rising from 2.4 in 1999 to 5.7 in 2015. The corresponding APC was 7.4% (95% CI=6.41, 8.31) between 1999 and 2009, and 3.5% (95% CI=2.08, 4.85) between 2009 and 2015. The ASR for ovarian cancer increased from 5.0 in 1999 to 6.3 in 2015. The corresponding APC was 1.8% (95% CI=1.46, 2.17).
Table 2
Age-standardized gynecologic cancer incidence rate per 100,000 and APC by cancer type among female patients in the Korea Central Cancer Registry, 1999–2015
|
Year |
Overall |
Cervix |
Endometrium |
Ovary |
|
1999 |
23.7 |
16.3 |
2.4 |
5.0 |
|
2000 |
22.1 |
15.1 |
2.3 |
4.8 |
|
2001 |
23.2 |
15.8 |
2.6 |
4.8 |
|
2002 |
22.7 |
14.8 |
2.8 |
5.0 |
|
2003 |
22.6 |
14.2 |
3.2 |
5.2 |
|
2004 |
21.4 |
13.2 |
3.1 |
5.2 |
|
2005 |
21.4 |
12.4 |
3.5 |
5.5 |
|
2006 |
21.3 |
12.3 |
3.6 |
5.4 |
|
2007 |
21.0 |
11.1 |
3.9 |
6.0 |
|
2008 |
21.6 |
11.5 |
4.4 |
5.7 |
|
2009 |
20.9 |
10.7 |
4.8 |
5.4 |
|
2010 |
21.6 |
11.0 |
4.7 |
5.9 |
|
2011 |
21.1 |
10.3 |
4.9 |
5.9 |
|
2012 |
20.8 |
9.7 |
4.9 |
6.2 |
|
2013 |
21.1 |
9.6 |
5.4 |
6.1 |
|
2014 |
21.1 |
9.2 |
5.4 |
6.5 |
|
2015 |
21.1 |
9.1 |
5.7 |
6.3 |
|
Trend 1 |
Range |
1999–2006 |
1999–2015 |
1999–2009 |
1999–2015 |
|
APC |
−1.36 |
−3.7 |
7.4 |
1.8 |
|
95% CI |
−2.15, 0.55 |
−4.05, −3.40 |
6.41, 8.31 |
1.46, 2.17 |
|
p-value |
p<0.001 |
p<0.001 |
p<0.001 |
p<0.001 |
|
Trend 2 |
Range |
2006–2015 |
|
2009–2015 |
|
|
APC |
−0.11 |
|
3.5 |
|
|
95% CI |
−0.62, −0.42 |
|
2.08, 4.85 |
|
|
p-value |
p=0.661 |
|
p<0.001 |
|

Fig. 2 illustrates the overall APCs for the 3 major gynecologic cancers according to site, and age group (
Supplementary Table 1). The overall APC of the 3 major gynecologic cancers in females younger than 30 years of age was 2.2%. The trends of APC have been variable in 30–39 age group, with a decrease (−3.6%) between 1999 and 2005, and an increase (2.4%) between 2005 and 2015. There has also been a variable trend of APC in females aged 80 years or older, with the trend increasing (8.6%) between 1999 and 2004, and decreasing (−0.8%) between 2004 and 2015. The incidence of cervical cancer has been decreasing in all age groups except in those aged between 30 and 39 years for latest period. The APC fell by 5.3% between 1999 and 2006, but rose by 1.5% between 2006 and 2015. The switch in incidence trends from an increase to a decrease has been identified from 2010, in women younger than 30 years old, and from 2003, in women aged 70 years or older. The incidence of endometrial cancer has been increasing in all age groups during the last 5 years of the study period. The extent of the increase, however, has fallen. The highest APCs were noted for endometrial cancer. Females younger than 30 years had the highest APC between 1999–2015. The incidence of newly diagnosed ovarian cancer with endometrial cancer has been consistently increasing in all age groups during the entire study period.
 | Fig. 2
APC in the incidences of overall gynecologic cancers, cervical, endometrial, and ovarian cancers by age group during 1999–2015.
APC, annual percent change.
*p<0.05.

|
DISCUSSION
The overall APC of the three major gynecologic cancers has decreased from −1.36% between 1999 and 2006, to −0.11 between 2006 and 2015 (
Table 2). This is mainly because of the decreasing incidence of cervical cancer, which showed stagnant trends in the last 5 years. During this period, the incidence of endometrial and ovarian cancers has been rising progressively. Compared to previous statistics, the incidence of newly diagnosed cervical (2,910), endometrial (2,741), and ovarian (2,709) cancer in 2018, tends to be converged [
2]. Based on the recent APCs of cervical (−3.7), endometrial (+3.5), and ovarian (+1.8) cancer from this study, the rank of each cancer may be similar to that of the USA in the near future. The estimated incidences of cervical, endometrial, and ovarian cancers in 2018 were 13,240, 63,230, and 22,240, respectively [
3].
The incidence of cervical cancer has been consistently decreasing between 1999 and 2015, with an APC of 3.7%. This trend was observed through all age groups in the early study period, except for those younger than 30 years and those aged 80 years or older. Notably, the incidence of cervical cancer had been increasing till 2010 in women younger than 30 years, with an APC of 5.1%, but has decreased ever since, with an APC of −6.5. The recent decline in the incidence of cervical cancer in these young women is probably due to better public health support, increased interest in cervical cancer screening, and attention effect of the introduction of vaccination. Cervical cancer vaccination has been introduced in Korea since 2007, and this may have increased awareness of the disease in younger women. The participation rate in the Korean nationwide cervical cancer screening program in women under the age of 39 has increased from 27.7% to 44.9%, between 2009 and 2014 [
7]. A decline in rates of high-grade squamous intraepithelial neoplasia (HSIL)/atypical squamous cells-cannot exclude HSIL (ASC-H) in this age group is consistent with the findings of the present study. The cervical cancer incidence had increased in elderly women till 2003, with the participation rate in the Korean nationwide cervical cancer screening program being the lowest during this period [
7]. This emphasizes the need for more active promotion of awareness and screening in this age group. Measures such as initiation of community outreach services, and mobile clinics, may be helpful for elderly women, particularly those with high risk factors [
8].
Although the APC of endometrial cancer decreased from 7.4 between 1999 and 2009, to 3.5 between 2009 and 2015, the incidence has been progressively rising. The total fertility rate in Korea was estimated at 1.178 at 2002; the ‘lowest-low fertility’ has lasted ever since [
9]. This nationwide trend, affecting the number of menstrual cycles over a lifetime, in conjunction with a western life style, may lead to a progressive increase in the incidence of endometrial cancer. In addition, another key factor may be a lack of gynecological surveillance, which has proven benefits in reducing endometrial cancer. Endometrial and colorectal cancer showed similar increase in trends during this period, probably owing to a shared genetic background, and etiologies. However, the incidence of colorectal cancer declined around 2011, reflecting proactive fecal occult blood testing, or colonoscopy, in the cancer screening program. In women, the APC of colorectal cancer was −1.8% between 2004 and 2015. [
10]. The association between mutated genes (
MLH1,
MSH2,
MSH6, and
PMS2) and the age at onset of endometrial cancers was demonstrated in a large study. The authors suggested the implementation of gynecological surveillance for endometrial cancer in women with known mutation carriers, using ultrasonography, hysteroscopy, or endometrial biopsy [
11]. It is expected that a recent increase in directed genome-wide sequencing studies, and multigene panel testing in Korea, will establish Korean-targeted surveillance, which has benefits in both, endometrial cancer prevention, and cost-effectiveness.
The incidence of ovarian cancer has been progressively on the rise, with an APC of 1.8%. The estimated number of new cases in 2018 is 2,709. This accounts for 2.9% of all cancer cases in women, with a ranking of 11 immediately after cancer of the uterine corpus [
12]. Although the rank of ovarian cancer is relatively low in terms of incidence, it is the most fatal gynecologic cancer. A total of 1,236 deaths from this cancer have been estimated in 2018, which accounts for 3.9% of the total estimated cancer deaths in females, ranking 8th in female cancer mortality [
12]. Preventive strategies have been widely implemented till date, owing to the lack of effective screening programs, acceptable methods of early detection, and a high rate of resistance to treatments [
2]. Since December 1, 2012, the Korean Health Insurance Review and Assessment service approved the use of risk-reduction surgery with or without preventive surgery for the high-risk population having
BRCA1 or
BRCA2 mutations based on genetic testing [
2]. The position statements released by the Korean Society of Gynecologic Oncology for risk-reducing salpingo-oophorectomy have also been considered [
13]. Korean women have a significant hereditary predisposition to ovarian cancer [
14]. The Korean Society of Obstetrics and Gynecology recently published a position statement recommending bilateral salpingectomy to reduce the risk of ovarian, fallopian, and peritoneal cancer, in women with average risk [
15]. Unfortunately, despite expectations of a decline in the incidence of ovarian cancer, owing to preventive strategies, no such trends were actually observed. Preventive surgical procedures, commonly performed in the age group between 40 and 50 years, need to be continued until the APC declines in the older age groups in the near future [
16]. Notably, the APC in women younger than 30 years was greater for the period between 1999 and 2015, than that recorded in the previous report between 1999 and 2010, being 0.9 (95% CI=0.11, 1.68) and −0.1 (95% CI=−1.44, 1.27), respectively. The APC of between 30 and 39 years was the greatest, among all age groups. These findings suggest that there may be other causes responsible the increasing in ovarian cancer in young women. The watchful expectation of results from preventive surgical procedures may not be the only solution.
In conclusion, the absolute incidence cases of the three major gynecologic cancers has increased between 1999 and 2015. However, the ASRs for the three major gynecologic cancers have reduced from 23.7 to 21.1 per 100,000 between 1999 and 2015, with an APC of −1.36% between 1999 and 2006, and −0.11% between 2006 and 2015. A decline in the incidence of cervical cancer has been noted during the last 5 years of the study period. Although the incidence of endometrial cancer is increasing, the rates have declined from an APC of 7.4% to 3.5% during the periods between 1999 and 2009, and between 2009 and 2015, respectively. The incidence of ovarian cancer has been gradually increasing, with an APC of 1.8% between 1999 and 2015. The dynamically changing patterns of incidence in cervical, endometrial, and ovarian cancer in Korea, are expected to follow the trends in the United States, in the near future [
3].





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download