1. Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ, et al. Risks of breast, ovarian, and contralateral breast cancer for
BRCA1 and
BRCA2 mutation carriers. JAMA. 2017; 317:2402–2416.

2. McCluggage WG. Morphological subtypes of ovarian carcinoma: a review with emphasis on new developments and pathogenesis. Pathology. 2011; 43:420–432.


3. Piek JM, van Diest PJ, Zweemer RP, Jansen JW, Poort-Keesom RJ, Menko FH, et al. Dysplastic changes in prophylactically removed fallopian tubes of women predisposed to developing ovarian cancer. J Pathol. 2001; 195:451–456.


4. Harmsen MG, Arts-de Jong M, Hoogerbrugge N, Maas AH, Prins JB, Bulten J, et al. Early salpingectomy (TUbectomy) with delayed oophorectomy to improve quality of life as alternative for risk-reducing salpingo-oophorectomy in
BRCA1/2 mutation carriers (TUBA study): a prospective non-randomised multicentre study. BMC Cancer. 2015; 15:593.



5. Dilley SE, Straughn JM. Leath CA. The evolution of and evidence for opportunistic salpingectomy. Obstet Gynecol. 2017; 130:814–824.


6. Yoon SH, Kim SN, Shim SH, Kang SB, Lee SJ. Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: a meta-analysis. Eur J Cancer. 2016; 55:38–46.


7. Venturella R, Lico D, Borelli M, Imbrogno MG, Cevenini G, Zupi E, et al. 3 to 5 years later: long-term effects of prophylactic bilateral salpingectomy on ovarian function. J Minim Invasive Gynecol. 2017; 24:145–150.

8. Van Lieshout LA, Pijlman B, Vos MC, de Groot MJ, Houterman S, Coppus SF, et al. Opportunistic salpingectomy in women undergoing hysterectomy: results from the HYSTUB randomised controlled trial. Maturitas. 2018; 107:1–6.


9. Song T, Kim MK, Kim ML, Jung YW, Yun BS, Seong SJ, et al. Impact of opportunistic salpingectomy on anti-Müllerian hormone in patients undergoing laparoscopic hysterectomy: a multicentre randomised controlled trial. BJOG. 2017; 124:314–320.


10. Song T, Lee SH, Kim WY, Heo EJ, Kim TJ. Opportunistic salpingectomy does not affect ovarian reserve or surgical outcomes in patients undergoing laparoscopic myomectomy. Gynecol Obstet Invest. 2017; 82:468–474.


11. Ganer Herman H, Gluck O, Keidar R, Kerner R, Kovo M, Levran D, et al. Ovarian reserve following cesarean section with salpingectomy vs tubal ligation: a randomized trial. Am J Obstet Gynecol. 2017; 217:472.e1–472.e6.

12. Antosh DD, High R, Brown HW, Oliphant SS, Abed H, Philip N, et al. Feasibility of prophylactic salpingectomy during vaginal hysterectomy. Am J Obstet Gynecol. 2017; 217:605.e1–605.e5.
13. Gill SE, Mills BB. Physician opinions regarding elective bilateral salpingectomy with hysterectomy and for sterilization. J Minim Invasive Gynecol. 2013; 20:517–521.


14. Chene G, de Rochambeau B, Le Bail-Carval K, Beaufils E, Chabert P, Mellier G, et al. Current surgical practice of prophylactic and opportunistic salpingectomy in France. Gynecol Obstet Fertil. 2016; 44:377–384.

15. Jones NL, Schulkin J, Urban RR, Wright JD, Burke WM, Hou JY, et al. Physicians' perspectives and practice patterns toward opportunistic salpingectomy in high- and low-risk women. Cancer Invest. 2017; 35:51–61.


16. Grol R, Wensing M, Eccles M. Improving patient care: the implementation of change in clinical practice. Edinburgh/New York: Elsevier Butterworth Heinemann;2005.
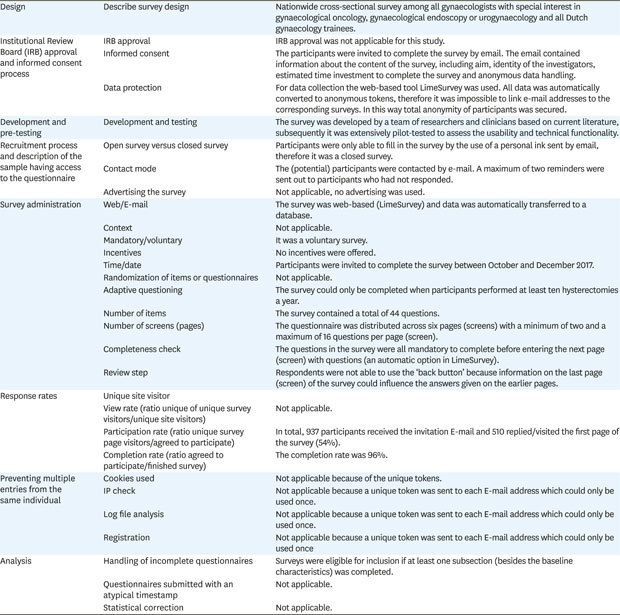
17. Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004; 6:e34.

18. Ghezzi F, Cromi A, Siesto G, Bergamini V, Zefiro F, Bolis P. Infectious morbidity after total laparoscopic hysterectomy: does concomitant salpingectomy make a difference? BJOG. 2009; 116:589–593.


19. Pölcher M, Hauptmann S, Fotopoulou C, Schmalfeldt B, Meinhold-Heerlein I, Mustea A, et al. Opportunistic salpingectomies for the prevention of a high-grade serous carcinoma: a statement by the Kommission Ovar of the AGO. Arch Gynecol Obstet. 2015; 292:231–234.


20. Committee on Gynecologic Practice. Committee opinion No. 620: salpingectomy for ovarian cancer prevention. Obstet Gynecol. 2015; 125:279–281.

21. Salvador S, Scott S, Francis JA, Agrawal A, Giede C. No. 344-opportunistic salpingectomy and other methods of risk reduction for ovarian/fallopian tube/peritoneal cancer in the general population. J Obstet Gynaecol Can. 2017; 39:480–493.


22. Royal College of Obstetricians & Gynaecologists. The distal fallopian tube as the origin of non-uterine pelvic high-grade serous carcinoma. Scientific impact paper No. 44. London: Royal College of Obstetricians & Gynaecologists;2014.
23. McAlpine JN, Hanley GE, Woo MM, Tone AA, Rozenberg N, Swenerton KD, et al. Opportunistic salpingectomy: uptake, risks, and complications of a regional initiative for ovarian cancer prevention. Am J Obstet Gynecol. 2014; 210:471.e1–471.11.

25. Robert M, Cenaiko D, Sepandj J, Iwanicki S. Success and complications of salpingectomy at the time of vaginal hysterectomy. J Minim Invasive Gynecol. 2015; 22:864–869.


26. van der Velden LFJ, Hingstman L. Monitor arbeidsmarkt gynaecologen 2006. Utrecht: NIVEL;2006.







 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download