Abstract
Purpose
We prospectively investigated clinical changes and long-term outcomes after administration of the drugs recommended by the Age-Related Eye Disease Study-2 to patients with intermediate age-related macular degeneration (AMD).
Methods
This prospective multicenter study enrolled 79 eyes of 55 patients taking lutein and zeaxanthin. The primary endpoint was contrast sensitivity; this was checked every 12 months for a total of 36 months after treatment commenced. The secondary endpoints were visual acuity, central macular thickness, and drusen volume; the latter two parameters were assessed using spectral domain optical coherence tomography.
Results
The mean patient age was 72.46 ± 7.16 years. Contrast sensitivity gradually improved at both three and six cycles per degree. The corrected visual acuity was 0.13 ± 0.14 logMAR and did not change significantly over the 36 months. Neither the central macular thickness nor drusen volume changed significantly.
Figures and Tables
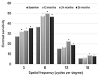 | Figure 1Bar graph showing the results of contrast sensitivity at each spatial frequency. Changing of contrast sensitivity during the follow-up period. *Significantly different than the baseline. |
 | Figure 2Changing of variables during the follow-up period. (A) Best-corrected visual acuity (BCVA). (B) Mean central macular thickness. (C) Mean drusen volume. (D) Area of hypo-fluorescence region. *Significantly different than the baseline. |
 | Figure 3A case of progression to advanced age-related macular degeneration. (A) Baseline. (B) After 36 months of administration of Age-Related Eye Disease Study-2 formula. FAF = fundus autofluorescence; OCT = optical coherence tomography; FA = fluorescein angiography; ICGA = indocyanine green angiography. |
References
1. Vingerling JR, Dielemans I, Hofman A, et al. The prevalence of age-related maculopathy in the Rotterdam study. Ophthalmology. 1995; 102:205–210.

2. Klein R, Chou CF, Klein BE, et al. Prevalence of age-related macular degeneration in the US population. Arch Ophthalmol. 2011; 129:75–80.

3. Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The beaver dam eye study. Ophthalmology. 1992; 99:933–943.
4. Krishnaiah S, Das TP, Kovai V, Rao GN. Associated factors for Age-related maculopathy in the adult population in southern India: the Andhra Pradesh eye disease study. Br J Ophthalmol. 2009; 93:1146–1150.

5. Miyazaki M, Nakamura H, Kubo M, et al. Risk factors for age related maculopathy in a Japanese population: the Hisayama study. Br J Ophthalmol. 2003; 87:469–472.

6. Song SJ, Youm DJ, Chang Y, Yu HG. Age-related macular degeneration in a screened South Korean population: prevalence, risk factors, and subtypes. Ophthalmic Epidemiol. 2009; 16:304–310.

7. Park SJ, Lee JH, Woo SJ, et al. Epidemiologic Survey Committee of the Korean Ophthalmologic Society; Age-related macular degeneration: prevalence and risk factors from Korean National Health and Nutrition Examination Survey, 2008 through 2011. Ophthalmology. 2014; 121:1756–1765.
8. Dimitrov PN, Mukesh BN, McCarty CA, Taylor HR. Five-year incidence of bilateral cause-specific visual impairment in the Melbourne visual impairment project. Invest Ophthalmol Vis Sci. 2003; 44:5075–5081.

9. Domalpally A, Danis R, Agrón E, et al. Evaluation of geographic atrophy from color photographs and fundus autofluorescence images: age-related eye disease study 2 report number 11. Ophthalmology. 2016; 123:2401–2407.
10. Ding X, Patel M, Chan CC. Molecular pathology of age-related macular degeneration. Prog Retin Eye Res. 2009; 28:1–18.

11. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001; 119:1417–1436.
12. Faria BM, Duman F, Zheng CX, et al. Evaluating contrast sensitivity in age-related macular degeneration using a novel computer-based test, the SPAETH/RICHMAN contrast sensitivity test. Retina. 2015; 35:1465–1473.

13. Maynard ML, Zele AJ, Feigl B. Mesopic Pelli-Robson contrast sensitivity and MP-1 microperimetry in healthy ageing and age-related macular degeneration. Acta Ophthalmol. 2016; 94:e772–e778.

14. Richman J, Spaeth GL, Wirostko B. Contrast sensitivity basics and a critique of currently available tests. J Cataract Refract Surg. 2013; 39:1100–1106.

15. Hammond BR, Fletcher LM, Roos F, et al. A double-blind, placebo-controlled study on the effects of lutein and zeaxanthin on photostress recovery, glare disability, and chromatic contrast. Invest Ophthalmol Vis Sci. 2014; 55:8583–8589.

16. Nolan JM, Power R, Stringham J, et al. Enrichment of macular pigment enhances contrast sensitivity in subjects free of retinal disease: central retinal enrichment supplementation trials - report 1. Invest Ophthalmol Vis Sci. 2016; 57:3429–3439.

17. Kvansakul J, Rodriguez-Carmona M, Edgar DF, et al. Supplementation with the carotenoids lutein or zeaxanthin improves human visual performance. Ophthalmic Physiol Opt. 2006; 26:362–371.

18. Loughman J, Nolan JM, Howard AN, et al. The impact of macular pigment augmentation on visual performance using different carotenoid formulations. Invest Ophthalmol Vis Sci. 2012; 53:7871–7880.

19. Nolan JM, Loughman J, Akkali MC, et al. The impact of macular pigment augmentation on visual performance in normal subjects: COMPASS. Vision Res. 2011; 51:459–469.

20. Olmedilla B, Granado F, Blanco I, Vaquero M. Lutein, but not alpha-tocopherol, supplementation improves visual function in patients with age-related cataracts: a 2-y double-blind, placebo-controlled pilot study. Nutrition. 2003; 19:21–24.
21. Ma L, Lin XM, Zou ZY, et al. A 12-week lutein supplementation improves visual function in Chinese people with long-term computer display light exposure. Br J Nutr. 2009; 102:186–190.

22. Bartlett HE, Eperjesi F. Effect of lutein and antioxidant dietary supplementation on contrast sensitivity in age-related macular disease: a randomized controlled trial. Eur J Clin Nutr. 2007; 61:1121–1127.

23. Woods RL, Wood JM. The role of contrast sensitivity charts and contrast letter charts in clinical practice. Clin Exp Optom. 1995; 78:43–57.

24. Legge GE, Rubin GS, Pelli DG, Schleske MM. Psychophysics of reading--II. Low vision. Vision Res. 1985; 25:253–265.

25. Lovie-Kitchin JE, Mainstone JC, Robinson J, Brown B. What areas of the visual field are important for mobility in low vision patients. Vision Res. 1990; 5:249–263.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download