Abstract
This paper reports a rare case of the symptomatic third metatarsal (MT3) - lateral cuneiform (LC) in a 55-year-old male who presented with complaints of severe intermittent pain in his right foot. Plain radiographs and computed tomography scans revealed sclerosis and irregularity at this joint. The intraoperative findings demonstrated a fibrocartilaginous coalition. The pain had improved one year after removing the MT3-LC joint by en bloc and arthrodesis.
There was a report about complete coalition (osseous fusion) between the third metatarsal (MT3) and lateral cuneiform (LC).1) Failure of a proper joint space formation during prenatal period (tarsal coalition) is the best explanation. Most tarsal coalitions are asymptomatic and incidental finding. Pain is often elicited by traumatic event. In case of pain refractory to conservative treatment, operative treatment including coalition resection or arthrodesis was done.2) Two reports for MT3-LC coalition have been published in the orthopaedic literature.1,3) One of them reported that the patient complained intermittent pain after trauma. One of these1) reported improvement of pain with conservative treatment and the other was improvement of painful non-osseous coalition was treated operatively.3) We describe another nonosseous coalition of MT3-LC joint with similar clinical history. The present report obtained informed consent from the patient.
This study was approved by the Institutional Review Board of Seoul Medical Center. A 55-year-old male presented to our clinic with complaints of severe intermittent pain in his right foot. An abrupt and striking pain started on the middle of the sole and sometimes migrated to forefoot when he stepped on a bump on a road on ordinary walk or sustained a mild twisting injury. He had no definite trauma history. He had underlying clevudine-induced myopathy, diabetes mellitus, and hypertension. He also had a mild limping gait caused by myopathy. The pain was not constant, but was frequent, and was so severe that he could not stand or walk for about 3 days after pain attack. In visual analogue scale score [VAS], he got 70 points out of 100. The pain had been present intermittently for approximately 3 years. Conservative management with medication, splint, and physical therapy improved his symptoms for a brief period. When pain was relieved, tenderness on a sole occurred rarely when walking. However, the symptoms were aggravated soon again. These symptoms wax and wane made the patient complain about anticipatory anxiety on walking. There was mild tenderness over the middle of the plantar area without restriction in range of motion of either the left ankle or the subtalar joint.
Radiographs demonstrated a suspicious MT3-LC joint irregularity compared to left foot oblique view (Fig. 1). No osseous or soft tissue abnormalities were detected. Sagittal and axial computed tomography scans (Fig. 2) demonstrated sclerosis and irregularity at the MT3-LC joint. Subchondral cyst was found on the MT3 side. Magnetic resonance imaging revealed low signal in T1-weighted image and intermediate signal in T2-weighted image for the articular ends (Fig. 3).
Having failed conservative management, the patient was given the option of arthrodesis of this joint as a means of definitive management. With the patient placed supine, longitudinal incision was made on the MT3-LC joint. Micromotion was observed by forceful dorso-plantar stress. The half of joint was connected with fibrocartilaginous tissue. We tried to remove the MT3-LC joint by en bloc resection. This was difficult due to deep and narrow joint space. Arthrodesis was performed using a strut iliac bone graft and fixed with one 4.0 mm cannulated screw, followed by a nonweightbearing cast for 6 weeks. Partial weightbearing and active range of motion exercise commenced at 6 weeks postoperatively. The patient complained of pain 3 months after first operation. A follow-up radiograph revealed that fusion had not been achieved (Fig. 4A). Second operation for fusion was tried using cancellous bone graft on bed for shell-outed non-union site and one 4.0 mm cannulated screw 6 months after first trial. Continuous pain on walk after the same rehabilitation protocol was present, as is in the first operation. Non-union was again confirmed in a follow-up radiograph (Fig. 4B). The reason of the failure was assumed that compression was not enough due to resistance of the intercuneiform and metatarsal ligaments. We blocked out the plantar and dorsal cortex around MT3-LC joint while remaining surrounding ligaments, and inserted a strut block bone harvested at the iliac crest tightly and fixed with low-profile plate and screws. Follow-up radiographs at 1 year postoperatively revealed bone union on MT3-LC joint within tolerable pain (VAS 20) (Fig. 5). At that time the patient had no subjective complaints of pain or instability regardless of activity level.
The incidence of the MT3-LC coalition reportedly ranges from 3.2% to 6.8%, and occurs in a wide variety of ages (documented in individuals from 17 to 68 years old) in the anthropology literature.4) However, compared with its incidence, reported symptomatic cases are rare.5) The one explanation for this rare occurrence might be associated with the fibrocartilaginous tissue at the coalition site free of nerve elements.6) Nerve endings served as pain receptors are present only in the periosteum around the coalition site and in the articular capsule surrounding affected tarsal bones. Another explanation is that the MT3-LC joint is stable and only rarely displays slight movement of 1.6° of sagittal plane motion.7) Therefore, this joint is less clinically relevant. These conditions are presumed to be the cause of the rare reports.13)
Generally, the cause for development of clinical symptoms is likely a mild trauma like a midfoot sprain. Although there was no specific trauma history in this case, gait disturbance associated with myopathy might have caused repeated and cumulative minor trauma that led to the pain.
There have been two reports of MT3-LC coalition.13) One was a bony coalition case whose pain resolved after conservative treatment with non-steroidal anti-inflammatory agents and immobilization.1) The other was a fibrocartilaginous coalition case.3) The patient in this case, having failed conservative management for 4 years, received an arthrodesis with proximal tibial bone graft. In first metatarsal (MT1) - medial cuneiform (MC) non-osseous coalition cases,89) the symptoms were resolved through arthrodesis or en bloc resection from the base of the bony prominence. An en bloc resection case confirmed a gliding motion of the MT1-MC joint after resection.9) From these findings, the authors concluded that the pain in the tarsal coalition is caused by mechanical abnormality resulting from incomplete coalition, which became painfree after resection. The MT3-LC joint is a mobile joint with small range likewise other tarsometatarsal joints.7) It rarely cause pain and walking disturbance in the normal condition. However, the limitation of movement associated with MT3-LC coalition after minor trauma with mobility of the joint could be a source of pain.
If the coalition is resectable and joint mobility can be recovered, it would be the best option. In case of talocalcaneal coalition, a coalition that occupied less than 30% to 50% of the total articular surface area is suggested to be resected.210) However, in MT3-LC coalition, the total articular surface was too small and deep to resect, arthrodesis to achieve absolute stability was considered as a preferable option.
Figures and Tables
 | Figure 1Medial oblique radiograph demonstrates the third metatarsal-lateral cuneiform joint irregularity (arrow) of the right foot (A) joint compared to left foot oblique view (B). |
 | Figure 2Computed tomography scans of the right foot demonstrates cortical irregularity (A, C) and subchondral cyst (B, D) of the third metatarsal-lateral cuneiform joint (arrows). |
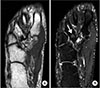 | Figure 3Magnetic resonance imaging scans of the right foot demonstrates low signal in T1-weighted image (A) (arrow) and intermediate signal in T2-weighted image (B) (arrow) of the third metatarsal-lateral cuneiform joint. |
References
1. Day FN 3rd, Naples JJ, White J. Metatarsocuneiform coalition. J Am Podiatr Med Assoc. 1994; 84:197–199.

2. Coughlin MJ, Mann RA, Saltzman CL. Surgery of the foot and ankle. Volume II. 8th ed. Philadelphia: Mosby;2007. p. 1073–1082.
3. Stevens BW, Kolodziej P. Non-osseous tarsal coalition of the lateral cuneiform-third metatarsal joint. Foot Ankle Int. 2008; 29:867–870.

4. Regan MH, Case DT, Brundige JC. Articular surface defects in the third metatarsal and third cuneiform: nonosseous tarsal coalition. Am J Phys Anthropol. 1999; 109:53–65.

5. Conway JJ, Cowell HR. Tarsal coalition: clinical significance and roentgenographic demonstration. Radiology. 1969; 92:799–811.

6. Kumai T, Takakura Y, Akiyama K, Higashiyama I, Tamai S. Histopathological study of nonosseous tarsal coalition. Foot Ankle Int. 1998; 19:525–531.

7. Ouzounian TJ, Shereff MJ. In vitro determination of midfoot motion. Foot Ankle. 1989; 10:140–146.

8. Takakura Y, Nakata H. Isolated first cuneometatarsal coalition: a case report. Foot Ankle Int. 1999; 20:815–817.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download