This article has been
cited by other articles in ScienceCentral.
Abstract
Sepsis and meningitis caused by Neisseria meningitidis are rare in neonates, but neonatal sepsis and meningitis are associated with a high rate of mortality. Meningococcal disease is commonly reported in older children and adolescents and is known to be more prevalent in community settings. In this study, a 16-day-old neonate was diagnosed with serogroup B meningococcal sepsis and meningitis. The baby was treated with antibiotics at the early stages of the infection and was discharged in good condition without any complications. This case report can serve to raise awareness of the incidence and importance of meningococcal infection in neonates, especially serogroup B.
Keywords: Meningococcal infections, Neisseria, meningitis
INTRODUCTION
Bacterial meningitis and sepsis (referred to as invasive meningococcal disease) are rare illnesses, but
Neisseria meningitidis is a frequent cause of the invasive disease in children and adults with high rate of mortality especially in the newborn infants.
1) No reliable estimates have been available for the global meningococcal disease burden because of inadequate surveillance in several parts of the world; however, previous studies have found that meningococcal meningitis comprises approximately 0.54% of neonatal meningitis cases.
23) Among serologically distinct meningococcal serogroups, the majority of invasive disease in young children less than 1 year of age is caused by serogroup B as demonstrated in our case.
4) This case report is to review meningococcal infections in neonates and to emphasize the necessity of prevention and chemoprophylaxis of exposed family members and health care staff.
CASE
A 16-day-old female patient, born by normal spontaneous delivery at a gestational age of 38±6 weeks with a birth weight of 2,870 g, visited the emergency department because of poor oral intake and an hour of high fever (39.4°C). The patient had no maternal and natal history and stayed at a postnatal care center until she was taken to our hospital. At the time of neonatal intensive care unit admission, her initial physical examination revealed mottling over her whole body and prolonged capillary filling time more than 2 seconds. The patient's admittance weight was 3,320 g and her initial vital signs were noted as follows: axillary temperature, 36.8°C; heart rate, 143 beats per minute; and respiratory rate, 50 breaths per minute. Blood and urine samples were collected from the patient. Her initial arterial blood gas analysis showed respiratory alkalosis. A complete blood count and serum biochemical analysis revealed a white blood cell (WBC) count of 4,530 cells/µL (segmented neutrophils, 54%; lymphocytes, 28%; monocytes, 15%; metamyelocytes, 1%; myelocytes, 1%; and blast, 1%), hemoglobin level of 17.1 g/dL, hematocrit of 50.9%, platelet count of 488,000 cells/µL, glucose concentration of 281 mg/dL, and Na, K, Cl, C-reactive protein (CRP), and procalcitonin levels of 130 mmol/L, 4.2 mmol/L, 97 mmol/L, 3.99 mg/dL (normal range <0.5 mg/dL), and 35.89 ng/mL (normal range <1.1 ng/mL), respectively. In addition, results of urinalysis and chest radiography were normal. Owing to concern for meningitis, examination of the cerebrospinal fluid (CSF) showed a WBC count of 10,470 cells/µL (neutrophils, 98% and monocytes, 2%), protein level of 378 mg/dL, and glucose concentration of 53 mg/dL. Hemodynamic support and empirical antibiotics (ampicillin and cefotaxime) were immediately administered in response to the clinical suspicion of late-onset sepsis and meningitis. The infant had persistent fever and worsening peripheral perfusion despite treatment; a moderate number of gram-negative cocci were found in CSF gram stain, and these signs and symptoms lead to suspicions of meningococcal infection. The patient's CRP level increased to 17.49 mg/dL after 12 hours and 27.73 mg/dL after another 24 hours; thus, the antibiotic regimen was changed to vancomycin (45 mg/kg/day in 3 divided doses) and cefotaxime (200 mg/kg/day in 4 divided doses). On the third day of hospitalization, the blood and CSF cultures showed gram-negative cocci, and she was isolated to prevent secondary infection. The patient had persistent fever (38.4°C), but her other vital signs were stable. On the fifth day, the gram-negative cocci were confirmed as N. meningitidis serotype B (MenB), and her antibiotic regimen was changed to penicillin G (300,000 IU/kg/day in 4 divided doses) and meningitis dose of cefotaxime (300 mg/kg/day in 4 divided doses). After the change in the antibiotic regimen, fever subsided, and the CRP level decreased to 12.22 mg/dL and finally to 0.91 mg/dL on the eighth day. The antibiotics were maintained for 10 days. A follow-up CSF study revealed a WBC count of 1,925 cells/µL (neutrophils, 61%; lymphocytes, 5%; and monocytes, 34%), protein level of 270 mg/dL, and glucose concentration of 20.2 mg/dL. The follow-up CSF and blood cultures indicated no meningococcal growth.
During hospitalization, the patient underwent brain ultrasonography and magnetic resonance imaging (MRI) for evaluation of neurologic complications or sequelae. Both radiologic examinations did not show any pathologic changes except a focal diffusion-restricted lesion in the splenium of her corpus callosum with mild edematous changes, which may be transient, but normal development of myelination was observed in brain MRI on her hospital day 11. Immunological analysis revealed that IgG/A/M/E levels, complement (C3 and C4), CD 3/4/8/9, and NK cells were within the normal range for her age, and findings on abdominal ultrasonography of screening for asplenia were unremarkable.
The patient was discharged in good overall condition on the thirteenth day of hospitalization. A follow-up examination of the patient in the outpatient clinic revealed no clinical abnormalities.
DISCUSSION
N. meningitidis infection can result in a range of diseases with devastatingly high mortality rates.
5) Onset of disease in susceptible individuals may be very rapid (within hours), and the fatality rate is high, especially among those presenting with septic shock, despite access to modern critical care.
4) Therefore, this case report is to assure the incidence of meningococcal disease in neonates and the importance of early detection and management as well as vaccination to prevent the spread of this fatal disease.
Among 12 serogroups of
N. meningitidis, serogroups A, B, C, X, W, and Y are only responsible for the majority of disease cases.
146) Despite the various pathogenic serogroups, widely available vaccines have been manufactured against serogroups A, C, W, and Y, but not serogroup B.
7) The invasive meningococcal infection in other countries show serotype B is predominant in all age groups, especially in infants; Bilal et al. analyzed 831 cases of neonatal bacterial meningitis in France from 2001 to 2013 and found that serogroup B was implicated in 78% of neonatal bacterial meningitis patients.
8) As serogroup B became an important health concern worldwide, two MenB vaccines, Bexsero
® (GSK, Brentford, UK) and Trumenba
® (Pfizer, Philadelphia, PA, USA), have been recently introduced.
479) UK and Ireland introduced MenB vaccine into the routine infant immunization program and the vaccine effectiveness reached 82.9% against all MenB cases in UK.
1011) Further studies are strongly encouraged to establish the key aspects in long-term success of vaccines and disease eradication.
5)
Nasopharyngeal carriage rate of meningococcus is reported to be approximately 10% in the general population and is carried asymptomatically by young adults, but invasive disease can occur in infants.
2912) Probably because of immunologic immaturity, infants have the highest incidence rate of meningococcal disease and second incidence peak is observed in adolescence and young adults possibly due to increase opportunity for exposure from social activities.
4) World Health Organization and The United States Centers for Disease Control and Prevention defined high risk groups who need vaccination as: infants, preteens, teens, young adults, and those living especially in community settings, as well as individuals with certain immune deficient conditions.
79) Considering the epidemiology of invasive meningococcal disease in Korea, the
8th edition of the Immunization Guideline of the Korean Pediatric Society also recommends the meningococcal vaccine for the high-risk individuals.
13) In addition, although the immunization guideline suggests that droplet isolation is only required during the first 24 hours of appropriate antibiotic administration, our patient was kept isolated according to our hospital isolation policy.
13)
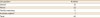
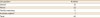
Chemoprophylaxis is a promising intervention to prevent meningococcal infection and should be administered as early as possible following the exposure; thus, her parents and exposed health care staffs were administered oral rifampin (intramuscular ceftriaxone for one pregnant nurse) for chemoprophylaxis (
Table 1).
13) One exposed neonate (labeled with * in
Table 1) was included to the prophylaxis list since he was placed next to the patient in the first day of hospitalization. There was no doubt to prophylaxis her parents, but prophylaxis of medical personnel was controversial since it is not routinely recommended except those exposed to aerosols of respiratory secretions before antibiotic therapy or during the first 24 hours after antibiotic therapy is initiated.
4) Their exact exposure time to the patient was unspecified, patient's oral secretion was frequently suctioned and they spent hours for several procedures such as intravenous catheterization and lumbar puncture. Also, studies have shown that the medical personnel who are exposed to meningococcal infection have 25 times higher incidence than do the general population.
13) Therefore, we decided to offer antibiotic prophylaxis to all exposed individuals to reduce further risk of secondary infection and observed them in outpatient clinic for two more weeks considering its incubation period.
Table 1
The number of individuals who underwent meningococcal chemoprophylaxis
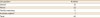
|
Occupation |
Number |
|
Doctor |
12 |
|
Nurse |
23 |
|
Family members |
6 |
|
Another patient*
|
1 |
|
Total |
42 |

Another interesting point is that meningococcal infection tends to spread wherever large groups of people gather together particularly in college dormitories and the army.
14) In Korea, most postpartum mothers prefer to stay at a private postnatal care center for at least two weeks after delivery; therefore, we want to pay attention to this unique cultural factor. The Infection Control and Prevention department performed surveillance for other infants who stayed with the patient prior to her presenting symptoms, and fortunately, no other sepsis or meningitis neonates were reported. In addition, meningococcus was not isolated from nasopharyngeal carriage among first-degree relatives or maternal vaginal carriage. Therefore, the direct sources of infection and influence of this unique community setting on development of disease in neonates remain unclear.
In this report, we successfully managed a 16-day-old neonate diagnosed with meningococcal sepsis and meningitis. Since the incidence of invasive meningococcal infection cannot be disregarded in neonates, newborns should not be exposed to crowded environments, and early detection and primary prevention of infectious disease should remain important.