Abstract
Purpose
To compare the success rates of performing only silicone tube intubation versus carrying out both conjunctival resection and silicone tube intubation.
Methods
The subjects of this study involved 62 patients (96 eyes) between October 2015 and May 2017 who were diagnosed as having punctal stricture or nasolacrimal duct stenosis. Out of 96 eyes, 47 underwent only silicone tube intubation, and 49 underwent both silicone tube intubation and conjunctival resection. Three parameters were measured at 1, 3, and 6 months after the surgery: the area of the tear meniscus using RTVue-100 anterior segment optical coherence tomography, the height of the tear meniscus using a slit lamp microscope, and the subjective satisfaction of patients as a result of improved sympotms like epiphora. The surgery was considered successful when the patients' experienced the resolution of symptoms and reduction of the area and height of the tear meniscus.
Results
The area of the tear meniscus, height of the tear meniscus, and subjective satisfaction of patients was superior in the group that underwent both silicone tube intubation and conjunctival resection compared silicone tube intubation only. Based on these results, the success rate of the surgery was 68.9% in the group that underwent only silicone tube intubation and 78.7% in the group that underwent both silicone tube intubation and conjunctival resection.
Conclusions
The resection of relaxed plica semilunares seems to increase the success rate of silicone tube intubation through the reduction of the area and height of the tear meniscus. Therefore, after determining the degree of conjunctivochalasis, if it was found to be severe, a combination with conjunctival resection was expected to increase the success rate of the surgery.
Lacrimation is a very common ophthalmic symptom, which is often caused by the closure of the lacrimal outflow system. Epiphora may result from various causes, such as trauma from repeated rivus lacrimaris enlargement procedures, burns, radiotherapy, conjunctivochalasis, lacrimal duct inflammation, xeroma, and drugs [1]. Silicone tube intubation has been widely used with dacryocystorhinostomy procedures since Keith [2] reported on it in 1968. It has been successful in patients of all ages with varied presentations, such as congenital nasolacrimal duct obstruction in infants and acquired nasolacrimal duct obstruction in adults [3].
There have been many studies to increase the success rate of silicone tube intubation. Jung et al. [4] compared the success rates of silicone tube intubation only and the combination with punctoplasties. Park et al. [5] found that two-stranded silicone tubes increased the success rate of surgery. Lee et al. [6] reported that the success rate varied according to the thickness of the silicone tube. In addition, the use of mitomycin C for silicone tube intubation resulted in a high success rate [7891011]. According to previous studies, the success rate of silicone tube intubation is estimated at 75% to 95% [121314].
Oh et al. [15] reported that scleral fixation of conjunctivochalasis resolved the symptoms in patients with epiphora. Based to this result, we focused on conjunctivochalasis to improve the success rate of silicone tube intubation. We expected conjunctivochalasis around the lacrimal caruncle to specifically block the lower punctum and affect tear flow. Therefore, we aimed to compare the success rates of carrying out only silicone tube intubation vs. carrying out both conjunctival resection and silicone tube intubation. Afterwards, we identified the clinical effects from both procedures.
The subjects of this study consisted of 62 patients (96 eyes) who visited Dong-A University Hospital for lacrimation between October 2015 and May 2017 and were diagnosed with nasolacrimal duct stenosis. All the patients were examined with a lacrimal syringing test and was only included if the syringing passed through a nasolacrimal duct. As a result of the syringing test, patients with regurgitation due to complete nasolacrimal duct obstruction were excluded. Their medical records were prospectively analyzed. This study was conducted with the approval of the institutional review board of Dong-A Univiersity Hospital (DAUHIRB-17-065). Informed consent was obtained from each patient. A total of 96 eyes were allocated in a randomized controlled fashion into two groups. Out of the 96 eyes, 47 underwent only silicone tube intubation, and 49 underwent both silicone tube intubation and conjunctival resection (Fig. 1). Patients who underwent silicone tube intubation and dacryocystorhinostomy for a diagnosis of lacrimal canaliculus and nasolacrimal duct stenosis as well as those with a history of cornea or conjunctival disease that may cause epiphora were excluded from this study. Silicone tube intubation was endoscopically performed. Lidocaine and epinephrine were mixed under the inferior nasal concha, and a wet cotton swab was placed for 5 minutes to allow for the nasal mucosa to contract. The infratrochlear and infraorbital nerves were then treated with 2% lidocaine as a local anesthetic. The lacrimal punctum was enlarged, and a lacrimal probe was used to clear the obstructions. The silicone tube was inserted into the nasal cavity through the superior and inferior nasolacrimal canaliculus while accurately identifying the Hasner valve in the inferior meatus using an endoscopy. The silicone tube taken out of the nose was knotted with a black silk thread, and the knot was fixed to the mucous membrane of the inferior meatus. After silicone tube intubation, the plica semilunaris was incised with a 2-mm × 4-mm rectangle and resected, followed by electrocauterization (Fig. 2A–2D). Although we did not completely remove the bulged plica semilunaris, the resection of the plica semilunaris was only performed if there was a mechanically complete obstruction of the lacrimal punctum due to an anteriorly bulged plica semilunaris. The obstruction was judged by one experienced operator using a slit lamp examination.
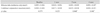
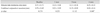
After the surgery, 0.5% moxifloxacin and 0.5% loteprednol etabonate eye lotion was administered to the eyes three times a day. The silicone tubes were maintained for at least 6 months and were removed when the lacrimation resolved and perfusion functioned well in the saline perfusion test. Three parameters were measured at 1, 3, and 6 months after the surgery: the area of the tear meniscus using RTVue- 100 anterior segment optical coherence tomography (Optovue, Fremont, CA, USA), the height of the tear meniscus using a slit lamp microscope, and the subjective satisfaction of patients according to the presence or absence of symptoms. The results were analyzed and compared between the patient group that underwent silicone tube intubation alone and the patient group that underwent both silicone tube intubation and conjunctival resection. The surgery was considered successful when the patients' experienced a resolution of symptoms and a reduction of the area and height of the tear meniscus. RTVue-100 anterior segment optical coherence tomography was performed 3 seconds after natural flickering after turning off the light. The area of the tear meniscus was measured by manually drawing a line along the boundary of the tear meniscus using the embedded program (Fig. 3A, 3B). The height of the tear meniscus was measured using the caliper of the slit lamp microscope (Fig. 4). The patients' subjective perception of symptoms and results of postoperative syringing tests was classified as ‘good,’ ‘normal,’ and ‘fail.’ The results were defined as ‘good’ if the symptoms were eliminated after surgery and passed the syringing test; ‘normal’ if the symptoms somewhat remained, but improved and passed the syringing test; and ‘fail’ if the symptoms were not improved and did not pass the syringing test. Clinical success was defined as ‘good’ or ‘normal.’
Statistical analysis was carried out using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The indices in both groups before and at 1, 3, and 6 months after the surgery were analyzed and compared through the Student t-test and chi-square test. A p-value <0.05 was considered to indicate statistical significance.
There was no significant difference in gender or age between the 29 patients (47 eyes) who underwent silicone tube intubation and the 33 patients (49 eyes) who underwent both conjunctival resection and silicone tube intubation. The initial area of the tear meniscus before surgery was 0.052 ± 0.046 mm2 in the group that underwent only silicone tube intubation and 0.059 ± 0.058 mm2 in the group that underwent both intubation and conjunctival resection. The initial height of the tear meniscus before surgery in the groups was 0.71 ± 0.75 and 0.76 ± 0.69 mm, respectively. There was no statistically significant difference in the area and height of the tear meniscus between the two groups before surgery (Table 1).
The area of the tear meniscus decreased at 1, 3, and 6 months after the surgery in both groups. There was no difference between the two groups at one month after the surgery. However, at 3 and 6 months after the surgery, the group that underwent both silicone tube intubation and conjunctival resection exhibited a statistically significant decrease in the area of the tear meniscus compared to the group that underwent only silicone tube intubation (Table 2 and Fig. 5A, 5B). The height of the tear meniscus also decreased in both groups after the surgery. There was no difference in the height of the tear meniscus between the two groups at 1 and 3 months after the surgery. However, at 6 months, the group that also underwent conjunctival resection exhibited a statistically significant decrease in this regard (Table 3 and Fig. 6A, 6B). There was no significant difference in the subjective satisfaction of patients (success of surgery which was rated as ‘good’ or ‘normal’) between the two groups at one month after the surgery. However, the satisfaction was higher in the group that underwent both silicone tube intubation and conjunctival resection at 3 and 6 months after the surgery (Table 4). Based on these results, the success rate of the surgery was 68.9% in the group that underwent only silicone tube intubation and 78.7% in the group that underwent both silicone tube intubation and conjunctival resection. Postoperatively, wound dehiscence occurred in one patient at the area of the resected conjunctiva that healed naturally. In one patient, a conjunctival granuloma formed, which was resected.
Although the success rate of silicone tube intubation has been reported to be lower than that of a dacryocystorhinostomy, silicone tube intubation protects the normal anatomical structure of the nasolacrimal duct. It has been widely used due to its technical simplicity, short surgery time, low pain, low bleeding risk, and fast postoperative recovery [2]. The silicone tube serves as a stent that reduces lacrimal outflow resistance and enlarges the diameter of the soft tissue of the nasolacrimal duct to increase lacrimal outflow. The mechanical obstruction of the lower punctum because of the relaxed conjunctiva from conjunctivochalasis, particularly the plica semilunaris, may reduce the effectiveness of silicone tube intubation and may interrupt lacrimal outflow. The plica semilunaris is a small wrinkle located in the bulbar conjunctiva of the inner canthus. It is retained as the nictitating membrane to protect the eyes in both birds and fishes and is referred to as the third eyelid. However, it is atrophied in primates, and consequently, the conjunctiva is not directly attached to the eyeball, thereby enabling greater rotation of the eyeball. It also forms a lacrimal lake during movement of the eyeball to prevent lacrimal outflow [16]. In this study, patients who underwent silicone tube intubation had a history conjunctivochalasis and an enlarged or elongated plica semilunaris. In this study, we identified that the plica semilunaris was more elongated than the bulbar conjunctiva, but the cause has yet to be elucidated. Therefore, further research is needed to clarify the cause, including histopathologic findings. Previous studies on conjunctivochalasis have reported the following causes: elastic fiber degeneration associated with aging [17], chronic inflammation [181920], lymphangiectasia according to a disorder of lymphatic vessel leakage, and a reduction of goblet cell count and collagen fiber density [21222324]. A comparison of the relaxed tissues in the plica semilunaris and bulbar conjunctiva in other areas may reveal the reason behind this finding.
Many previous studies have reported that anterior segment optical coherence tomography has high accuracy and good reproducibility for tear meniscus measurements [2526]. Based on these reports, we used anterior segment optical coherence tomography to measure the area of the tear meniscus. There was no significant difference in the area or height of the tear meniscus between the two groups immediately after the surgery. However, 3 months after the surgery, the group that underwent both silicone tube intubation and conjunctival resection exhibited a significant decrease in the tear compared to the group that underwent only silicone tube intubation. Immediately after the surgery, there may not have been a significant difference in the area and height of the tear meniscus between the two groups due to the inflammation and edema of the resected conjunctiva. However, over time, the enlarged and elongated conjunctiva was removed and the wound healed, thereby enabling smoother operation of the lacrimal outflow system through the lower punctum. Consequently, more effective tear perfusion occurred in the group that underwent both silicone tube intubation and conjunctival resection. The patients' symptoms resolved as the tear perfusion began to function more smoothly. Therefore, the symptoms seemed to be correlated with the area and height of the tear meniscus.
Limitations of this study were that the degree of the relaxed conjunctiva was not quantified and that the conjunctiva was resected under the subjective judgment of the surgeon. Kim et al. [27] reported that the degree of conjunctivochalasis could be objectively assessed using an anterior segment optical coherence tomography. This limitation may be improved by objectively quantifying the condition of the relaxed conjunctiva through anterior segment optical coherence tomography before silicone tube intubation. Moreover, although we included a relatively large number of samples (96 eyes), long-term follow-up for over 6 months was not performed. Therefore, re-evaluations through longer follow-ups may be necessary.
The low success rate of surgery reported herein may have resulted from the high standards of what was considered a successful surgery, i.e., one that satisfies all three factors (improvement in the area and height of the tear meniscus and symptoms). However, in terms of the complications of conjunctival resection, only two of the 96 eyes exhibited wound dehiscence (n = 1) and a conjunctival granuloma (n = 1). Therefore, the surgery is considered a safe procedure with low complication rates.
In conclusion, relaxed plica semilunaris resection seems to increase the success rate of silicone tube intubation through the reduction of the area and height of the tear meniscus, similar to other factors in other studies for increasing the success rate of silicone tube intubation. Therefore, if silicone tube intubation is planned, the extent of conjunctiva relaxation should be determined. If the bulged plica semilunaris is mechanically blocking the punctum, a combination with conjunctival resection is expected to increase the success rate of the surgery.
Figures and Tables
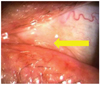 | Fig. 1The arrow showing the conjunctivochalasis. Bulged plica semilunaris is blocking lower punctum. |
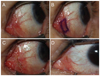 | Fig. 2The process of conjunctival resection. (A) Preoperative state. (B) The conjunctivochalasis of plical semilunaris was marked by pen. (C) Marked area was resected and followed by electrocauterization. (D) Postoperative state after 6 months. |
 | Fig. 3The area of the tear meniscus. (A) The arrow shows the longitudinal plane of tear meniscus. (B) The area was measured bymanually drawing a line along the boundary of the tear meniscususing RTVue-100 anterior segment optical coherence tomography. |
 | Fig. 4The height of the tear meniscus was measured using the caliper of the slit lamp microscope. The yellow dot line and arrowhead show the area and heights of tear meniscus. |
 | Fig. 5The RTVue-100 anterior segment optical coherence images show that the area of tear meniscus was de creased after surgery. (A) Preoperative state and (B) postoperative state. |
 | Fig. 6The height of the tear meniscus, as shown through the yellow dot line, using the caliper of the slit lamp microscope was decreased after surgery. (A) Preoperative state and (B) postoperative state. |
References
1. Oum JS, Park JW, Choi YK, et al. Result of partial nasolacrimal duct obstruction after silicone tube intubation. J Korean Ophthalmol Soc. 2004; 45:1777–1782.
3. Beigi B, O'Keefe M. Results of Crawford tube intubation in children. Acta Ophthalmol (Copenh). 1993; 71:405–407.

4. Jung JJ, Jang SY, Jang JW, In JH. Comparison results of silicone tube intubation according to syringing and dacryocystography. J Korean Ophthalmol Soc. 2014; 55:1584–1588.

5. Park JJ, Shin DS, Hong SP, Lee KW. Effects of double silicone tube intubation for nasolacrimal duct obstruction in adults. J Korean Ophthalmol Soc. 2005; 46:1951–1956.
6. Lee DH, Choi HY, Ahn JH. Comparison of results and complications between 0.64 mm and 0.94 mm silicone tube intubation in adults. J Korean Ophthalmol Soc. 2016; 57:1193–1198.

7. Lee KS, Byun YJ. Dacryocystorhinostomy with intraoperative mitomycin C. J Korean Ophthalmol Soc. 1998; 39:1909–1914.
8. Kim YT, Chung WS. The effect of mitomycin C in endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2002; 43:728–732.
9. Lee JM, Lee YJ, Kim JH. The effect of mitomycin C concentration in endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2004; 45:1609–1614.
10. Song BY, Kim JD, Kim S. Silicone intubation and postoperative mitomycin application for partial nasolacrimal duct obstruction in adults. J Korean Ophthalmol Soc. 2005; 46:16–21.
11. Kim DS, Lee YJ. Efficacy of silicone nasolacrimal intubation with mitomycin C treatmentfor treatment of incomplete nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2006; 47:181–185.
12. Lim CS, Martin F, Beckenham T, Cumming RG. Nasolacrimal duct obstruction in children: outcome of intubation. J AAPOS. 2004; 8:466–472.

13. Kaufman LM, Guay-Bhatia LA. Monocanalicular intubation with Monoka tubes for the treatment of congenital nasolacrimal duct obstruction. Ophthalmology. 1998; 105:336–341.

14. Engel JM, Hichie-Schmidt C, Khammar A, et al. Monocanalicular silastic intubation for the initial correction of congenital nasolacrimal duct obstruction. J AAPOS. 2007; 11:183–186.

15. Oh SH, Park JY, Yim HB, Lee NY. Treatment of epiphora in patients with conjunctivochalasis using conjunctival fixation to the sclera. J Korean Ophthalmol Soc. 2012; 53:1063–1067.

16. Dartt DA. The conjunctiva: structure and function. In : Duane TD, Tasman W, Jaeger EA, editors. Duane's foundations of clinical ophthalmology. Philadelphia: Lippincott, Williams & Wilkins;2012. p. 11.
17. Watanabe A, Yokoi N, Kinoshita S, et al. Clinicopathologic study of conjunctivochalasis. Cornea. 2004; 23:294–298.

18. Francis IC, Chan DG, Kim P, et al. Case-controlled clinical and histopathological study of conjunctivochalasis. Br J Ophthalmol. 2005; 89:302–305.

19. Meller D, Li DQ, Tseng SC. Regulation of collagenase, stromelysin, and gelatinase B in human conjunctival and conjunctivochalasis fibroblasts by interleukin-1beta and tumor necrosis factor-alpha. Invest Ophthalmol Vis Sci. 2000; 41:2922–2929.
20. Erdogan-Poyraz C, Mocan MC, Bozkurt B, et al. Elevated tear interleukin-6 and interleukin-8 levels in patients with conjunctivochalasis. Cornea. 2009; 28:189–193.

21. Ellis S. Structure and function of the lymphatic system: an overview. Br J Community Nurs. 2006; 11:S4–S6.

22. Skandalakis JE, Skandalakis LJ, Skandalakis PN. Anatomy of the lymphatics. Surg Oncol Clin N Am. 2007; 16:1–16.

23. Kim JT, Kim JH, Kim JC. Visualization of subconjunctival lymphatics and its significance. J Korean Ophthalmol Soc. 2008; 49:1215–1219.

24. Bae JB, Park WC. Histopathologic characteristics of conjunctivochalasis. J Korean Ophthalmol Soc. 2013; 54:1165–1174.

25. Wang J, Aquavella J, Palakuru J, Chung S. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2006; 47:3325–3329.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download