INTRODUCTION
Brain death refers to the irreversible cessation of all functions of the brain, including the brainstem.
1 Organ donation from brain-dead donors enables the transplantation of organs that are essential for life, such as the heart. In addition, this type of organ donation helps to overcome limitations, such as organ donations that cannot be donated by living organ donation, family conflicts that may occur from living organ donation, and complications for donors after surgery.
2
In Korea, the first corneal transplant was performed in 1945; the first kidney transplant from a brain-dead donor in 1979; and the first liver transplant from a brain-dead donor in 1988.
3 Thereafter, a public hearing on brain death was held, and a “special committee on brain death research” was established in the Korean Medical Association in 1989. The committee proposed to legislate brain death based on “the definition of death and the criterion of brain death as cardiac and respiratory failure or the irreversible loss of whole brain function including the brainstem.” Finally, in February 1992, the Organ Transplant Act was enacted according to the legislative demands of the medical community and the request of society members.
4
In 2000, the Korean Network for Organ Sharing (KONOS) was established to ensure the equal distribution of donated organs to patients waiting for organ transplants and to address issues related to organ extraction and appropriate donation of organs. In addition, the legislation of the brain death determination process made it possible for the Hospital-Based Organ Procurement Organization (HOPO) to completely manage the process in a unified manner.
3 In 2010, to address the serious imbalance in organ supply and demand, the Organ Transplant Act was amended to include new regulations for notifying and reporting of brain-dead potential organ donors and the introduction of the Organ Procurement Organization, which supports the overall brain-dead organ extraction process.
3
In Korea, the brain death determination process begins when consent is acquired from the guardian after conducting interviews associated with organ donation. The process of determining brain death proceeds in the order of the first brain death examination, second brain death examination, electroencephalography (EEG), and decision by the special committee on brain death.
Prerequisites are confirmed before the first brain death examination. During the first brain death examination, seven brainstem reflexes are confirmed, and an apnea test is performed. The second brain death examination, identical to the first brain death examination, is conducted at a 6-hour interval for adults after the first brain death examination. Then, an EEG examination is performed for 30 minutes or longer to determine if the brain waves are flat. Finally, when a unanimous decision is made through meetings of the brain death special committee, the time of death is declared as the time brain death is determined. The Committee for Brain Death Evaluation comprises at least one neurologist or neurosurgeon, two medical specialists (not general physicians), and at least one non-medical personnel, such as a priest or a social worker. This committee convenes only once after the first and second assessments of brain death and EEG check-up, and meets only when proceedings concern brain-dead organ donors in Korea. After a series of brain death determination processes, organ donation surgeries are performed, and the body is then transferred to the funeral home.
5 All processes involved in pediatric brain death determinations are the same except for the mandatory interval between two brain death assessments: age 2 months–1 year, 48 hours; age 1–6 years, 24 hours; and age over 6 years, 6 hours; and for donors less than 1 year, two EEG check-ups after the first and second brain death assessments.
As a result of various efforts to promote organ donation, organ transplants from brain-dead donors in Korea are increasing every year, but the number of brain-dead donors remains insufficient considering the number of patients awaiting organ transplants, suggesting that the number of brain-dead organ donations should continue to increase.
6 The number of patients waiting for an organ transplant increased steeply from 1,842 in 2012 to 3,506 in 2016, whereas the number of brain-dead organ donors saw a slight increase from 409 in 2012 to 573 in 2016.
7 During various stages of the abovementioned management process, organ donation is significantly hindered.
This study was conducted to promote brain-dead organ donation and explore ways to resolve the imbalance between organ supply and demand by analyzing the causes of organ donation failure from brain-dead potential organ donors in Korea.
METHODS
This study was based on information obtained from the 8,120 potential brain deaths reported to the Korea Organ Donation Agency from January 1, 2012 to December 21, 2016 according to the potential brain death reporting system under Article 17 of the Organ Transplant Act. In addition, data of the donation suitability evaluations performed by the coordinator after the report and the data derived from interviews with the hospital medical staff and the donor's family were analyzed retrospectively. A total of 321 hospitals reported potential brain deaths over the past 5 years. Among these, the number of HOPO was 36.
The process of managing brain-dead organ donors in Korea is shown in
Fig. 1. The definitions of some terms used in this study are as follows; most of them are cited from Lee et al.
8's, Assessment of Brain-Dead Potential Organ Donors, 2016.
 | Fig. 1
|
1) Brain-dead potential organ donors: A patient characterized by a Glasgow Coma Scale score of less than 4, coma mentality with irreversible brain injury, and no self-respiration with ventilator care.
2) Medically suitable brain-dead donors: Brain-dead patients with no absolute contraindication for organ donation. Absolute contraindications are transmittable infections, such as active tuberculosis and tumors with malignancy, with the exception of low-grade central nervous system tumors.
3) Request donors: The donors asked to donate organs to their family members.
4) Consent donors: The donors agreed to donate to their family members.
5) Eligible donors: Organ donors who passed the first brain death assessment. In Korea, donors who pass the first brain death assessment can be reported to KONOS, which then starts the process of determining suitable recipients in need.
6) Actual donors: Organ donors who undergo organ procurement surgery, including those whose organs are not used.
7) Transplantation donors: Organ donors who undergo organ procurement surgery with designated recipients.
Ethics statement
This study was granted exemption from approval by the Institutional Review Board (IRB) of Korea University Medical Center (IRB No. 2018AN0071). There is no informed consent.
RESULTS
From January 2012 to December 2016, the total number of brain-dead potential organ donors reported in Korea was 8,120. During this period, the total number of transplantation donors who underwent actual organ procurement surgery and went from being medically suitable brain-dead organ, request, consent, and eligible donors to actual donors was 2,348, accounting for 28.9% of the total brain-dead potential organ donors (
Fig. 2).
 | Fig. 2 Organ donors who have undergone organ procurement surgery through the entire management process from identification as brain-dead potential organ donors to actual donation (2012–2016).
|
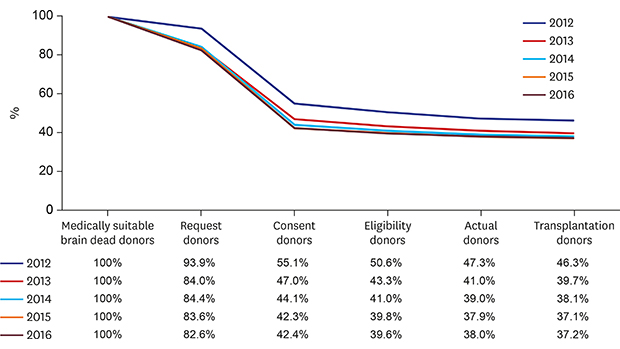
The annual percentages of request, consent, eligible, actual, and transplant donors compared with those of medically suitable brain-dead organ donors from 2012 to 2016 are shown in
Table 1. The number of medically suitable brain-dead donors and transplantation donors increased by 1.74 and 1.38 times, respectively, in 2016 compared with that in 2012. The proportion of transplantation donors to medically suitable brain-dead donors decreased from 46.3% in 2012 to 37.2% in 2016; however, the actual number of transplant donors increased from 2012 to 2016.
Table 1
Number of organ donors in the management process from medically suitable brain-dead donors to actual donation by year (2012–2016)
|
Categories |
No. (% from medically suitable brain-dead organ donors) |
|
2012 |
2013 |
2014 |
2015 |
2016 |
|
Medically suitable brain-dead organ donors |
887 (100.0) |
1,038 (100.0) |
1,173 (100.0) |
1,346 (100.0) |
1,539 (100.0) |
|
Request donors |
833 (93.9) |
872 (84.0) |
991 (84.4) |
1,126 (83.6) |
1,272 (82.6) |
|
Consent donors |
489 (55.1) |
488 (47.0) |
518 (44.1) |
570 (42.3) |
653 (42.4) |
|
Eligibility donors |
449 (50.6) |
450 (43.3) |
482 (41.0) |
536 (39.8) |
610 (39.6) |
|
Actual donors |
420 (47.3) |
426 (41.0) |
458 (39.0) |
511 (37.9) |
585 (38.0) |
|
Transplantation donors |
414 (46.3) |
413 (39.7) |
448 (38.1) |
500 (37.1) |
573 (37.2) |

Fig. 3 shows the failure factors at each stage of the brain-dead donor management process. The common cause of failure in each stage of the management process was donation refusal in 2,257 cases (27.6%), followed by non-brain death in 1,299 cases (15.5%) and unsuitable donors in 949 cases (11.7%). The details of unsuitable donors include uncertain full recovery of cancer, prostate cancer detection, failure due to cholangiocarcinoma, failure due to renal cell carcinoma, disseminated intravascular coagulation findings, neurological death caused by unidentifiable drug addiction, organ function depression due to sepsis, severe hemodynamic instability, malignant findings from kidney tissue examination during extraction, and poor vascular status observed during extraction. Cardiac death, with a total of 800 cases (9.8%), was a cause of failure that occurred consistently throughout all phases of the brain-dead donor management process.
 | Fig. 3 Failure factors for each stage of the brain-dead donor management process (2012–2016).
|
Without a legal guardian, KONOS cannot register the patient as a brain-dead organ donor with consent to organ donation; thus, the absence of a legal guardian was a failure factor associated with only eligible donors, accounting for a total of 81 cases (1.0%). The circumstances of these cases included the absence of a guardian with legal priority, when a guardian with legal priority is known and identified but cannot be contacted, when it is impossible to verify family relationships, and absence of a domestic guardian because the donor is a foreigner.
In cases of accidental death, if the patient's cause of death is unnatural, approval must be obtained from the prosecution for an organ procurement surgery before the autopsy. However, during this process, an autopsy may be necessary to determine the cause of death, and this represents another cause of failure. This problem can also occur at any time during communication with prosecutors in the management of brain-dead donors, accounting for a total of 16 cases (0.2%). The circumstances include when the guardian withdraws consent to donate during the process of identifying the cause of accidental death, when the guardian withdraws consent to donate because a general autopsy is necessary owing to an accidental death, when extraction is rejected before the autopsy, when autopsy is necessary owing to traumas found during extraction, etc.
As mentioned in the above, the brain death determination process in Korea consists of the following 4 major stages: the first and second brain death examinations, EEG, and decision by the brain death special committee.
Fig. 4 presents the reasons for failure during the brain death determination stages, including those that occur during registration in KONOS as a brain-dead organ donor.
 | Fig. 4 Causes of failure during the brain death determination process (2012–2016).
|
DISCUSSION
In Korea, an imbalance in the supply and demand of transplant organs has become a concern due to the shortage of brain-dead organ donors and rapidly increasing number of patients awaiting organ transplants every year, resulting in an urgent need to increase the brain-dead organ donation rate. In this situation, a thorough understanding of factors that lead to successful organ donation is critical. Moreover, attempts to reduce the failure rate by identifying failure factors of organ donation at various stages during the organ donation management process will significantly affect the success of organ donation.
Cases in which medically suitable brain-dead organ donors are unable to proceed to the request donor phase are presented in
Fig. 2 and
Table 1. In Korea, a legal clause on the notification and reporting obligation of potential brain deaths has been developed so that organ donation information could be delivered to every potential brain-dead organ donor.
The major failure factors in the process of brain-dead potential organ donors becoming transplantation donors are observed between the request and consent donor phases. In other words, the very low rate of consent is the greatest failure factor in brain-dead organ donation. In this study, among the potential brain deaths provided with organ donation information over the past 5 years (from January 2011 to December 2016), the organ donation consent rate was 53.3%. However, in practice, some hospitals did not report medically suitable brain-dead organ donors if consent was not obtained after attempting to encourage organ donation; therefore, the actual consent rate is expected to be much lower. This is in contrast with the 50%–80% organ donation consent rate of brain death families reported in Western studies.
9
Several reports have addressed the lower organ donation consent rate in Korea compared to the rate in other countries. There are claims that the Korean organ donation rates are low due to the traditional custom of avoiding physical damage after death.
10 In addition, 65.1% of trauma patients agree to donate organs, while only 34.9% of the guardians of patients with non-traumatic causes agree to organ donation, suggesting that traumatic causes are associated with organ donation consent. In this context, several studies have asserted that families with traumatic brain deaths are more likely to accept brain death due to the effects of exposure to similar situations through the media.
11 Therefore, continuous education and publicity may be necessary to evolve the cultural perception of organ donation.
Although the failure rate between eligible donors and actual and transplantation donors is low, attempts to maintain a low failure rate in this phase are crucial because the first brain-dead examination has already been completed with the consent of the guardian. Brain death determination is an essential aspect of this process. Laws and protocols have been established by the government for the determination of brain death in Korea, which are in accordance with the American Academy of Neurology (AAN) guidelines. Apnea and ancillary tests are required, and two physicians perform the brain death examination for adults at a 6-hour interval. In Spain, the country with the largest number of brain-dead organ donations, the laws and protocols are also consistent with the AAN guidelines except that ancillary tests are optional, and 3 physicians perform the brain death examination without time intervals to determine brain death. In the United States, the protocol varies from state to state; most hospitals (66%) perform 2 brain death examinations, a few hospitals (21%) perform 2–5 brain death examinations, and an even smaller number of hospitals (13%) perform 1 brain death examination. In Australia, 2 physicians perform the brain death examination at 0- to 5-hour intervals, whereas in Germany, 2 physicians perform the brain death examination at intervals of 11–15 hours.
12 Therefore, the brain death examination process in Korea is neither particularly strict nor lenient compared with that in other countries.
However, various opinions exist regarding the timing of the determination of brain death. Some argue that it should occur during the first brain death examination (brain death determination requirement satisfaction theory), while others argue that it should occur during the second brain death examination (observation time elapsed theory).
13 The German Federal Medical Association guideline for brain death determination stipulates the time of death as the end of the diagnosis and recording.
14 Korea is unique in that it has a special committee on brain death, which differs from other countries that confer brain death determination rights to physicians.
15 A study suggested that the determination of brain death must be performed by physicians and not by a committee, that the brain death determination criteria should not be determined by a majority vote, and that it is reasonable for the subject of responsibility for misjudgment to be the physician and not the brain death special committee.
15 The brain death special committee in Korea may be no more than a group that reviews the brain death examination that has already been conducted.
According to the study results, the common causes of organ donation failure throughout the process included donation refusal (27.6%), non-brain death (15.5%), and incompatible donation (11.6%). These factors cannot be modified significantly within the current institutional and medical frameworks in Korea. However, there is room for improvement for the 3 factors of cardiac death, absence of a legal guardian, and accidental death. First, there were 800 cases of cardiac death (9.8%) in this study, but no data were available regarding the causes of cardiac death. Because potentially brain-dead patients are hemodynamically unstable and critically ill, management by medical staff with a rigorous understanding of brain death is considered to be critical. In light of efforts in the US and other Western nations, there is considerable evidence in the literature that specific care protocols or critical management pathways can increase hemodynamic stability, decrease cardiac arrest, and increase the number of organs recovered per donor.
16,17 In Korea, a brain-dead organ donor management protocol should be established, and research and efforts to identify the cause of cardiac death during the brain death organ donation process should be conducted to reduce its incidence.
Second, 81 cases (1.0%) had an absence of a legal guardian. With the increasing tendency toward nuclear families in Korea, the number of one person has also increased, making consent for organ donation even more difficult to obtain. As per Article 12 of the Organ Transplant Act, a written consent for organ donation must be obtained from a guardian with legal priority. If the legal guardian is missing or is unable to provide consent owing to unavoidable circumstances, the person at the next level of legal priority can provide consent. However, the absence of guardians with primary and secondary legal priority precludes organ donation because no one possesses the right to consent. In addition, organ donation requires documentation to identify the relationship between the brain-dead patient and guardian. In cases of brain death due to sudden accidents, guardians may feel burdened by complicated procedures for issuing documents in the midst of a psychologically difficult situation. Therefore, the laws and systems associated with these circumstances should be reviewed and improved.
Third, 16 cases (0.2%) had accidental deaths. In these cases, guardians are under psychological pressure because they are in contact with the police, prosecutors, and lawyers regarding the accidental death, and in some cases, they feel negatively about organ donation. In addition, if the prosecution requires an autopsy due to the accidental death, organ donation cannot be undertaken unless extraction is approved before the autopsy. The families of brain-dead patients are extremely psychologically vulnerable and therefore may be more likely to react poorly to trivial matters. Therefore, prioritizing organ donation education for police officers and prosecutors who have a limited understanding of brain death compared to medical staff will enhance their ability to navigate its complexities and will foster more compassionate communications with guardians. In addition, the extraction approval rejection rate prior to autopsy may decrease.
This study may lead to more successful organ donations by illuminating the causes of failure in the management process from the identification of brain-dead potential organ donors to actual donation and delineating various methods to address them. However, because this study lacks certain details regarding the causes of failure or merely summarizes them, further studies are warranted for elaborating on these dynamics. Furthermore, efforts should be made to encourage brain-dead potential donors to become successful organ donors during the process of identifying potential brain deaths at each hospital and to investigate the challenges faced by medical staff in managing organ donation.





 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download