1. Ferrari S, Reginster JY, Brandi ML, et al. Unmet needs and current and future approaches for osteoporotic patients at high risk of hip fracture. Arch Osteoporos. 2016; 11:37. PMID:
27800591.

2. Steinberg GG, Desai SS, Kornwitz NA, Sullivan TJ. The intertrochanteric hip fracture. A retrospective analysis. Orthopedics. 1988; 11:265–273. PMID:
3357844.

3. Morris AH, Zuckerman JD; AAOS Council of Health Policy and Practice, USA. National Consensus Conference on improving the continuum of care for patients with hip fracture. J Bone Joint Surg Am. 2002; 84-A:670–674. PMID:
11940633.
4. Doppelt SH. The sliding compression screw--today's best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980; 11:507–523. PMID:
7413172.

5. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992; 74:340–344. PMID:
1587873.

6. Larsson S, Elloy M, Hansson LI. Fixation of unstable trochanteric hip fractures. A cadaver study comparing three different devices. Acta Orthop Scand. 1988; 59:658–663. PMID:
3213452.

7. Mulholland RC, Gunn DR. Sliding screw plate fixation of intertrochanteric femoral fractures. J Trauma. 1972; 12:581–591. PMID:
5044317.

8. Anglen J, Banovetz J. Compartment syndrome in the well leg resulting from fracture-table positioning. Clin Orthop Relat Res. 1994; (301):239–242.

9. Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am. 1992; 74:1450–1455. PMID:
1469004.

10. Callanan I, Choudhry V, Smith H. Perineal sloughing as a result of pressure necrosis from the traction post during prolonged bilateral femoral nailing. Injury. 1994; 25:472. PMID:
7960054.

11. Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949; 31B:190–203. PMID:
18150534.

12. Orthopaedic Trauma Association Committee for Coding and Classification. Fracture and dislocation compendium. J Orthop Trauma. 1996; 10(Suppl 1):v–ix. 1–154. PMID:
8814583.
13. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; (310):150–159.
14. Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Strømsøe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998; 12:241–248. PMID:
9619458.

15. Kyle RF, Cabanela ME, Russell TA, et al. Fractures of the proximal part of the femur. J Bone Joint Surg Am. 1994; 76:924–950.

16. Im GI, Shin YW, Song YJ. Potentially unstable intertrochanteric fractures. J Orthop Trauma. 2005; 19:5–9. PMID:
15668577.

17. Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007; 89:470–475. PMID:
17332094.
18. Hardy DC, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw compared with a compression hipscrew with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998; 80:618–630. PMID:
9611022.

19. Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998; (348):87–94. PMID:
9553538.

20. Lee KH, Jeong H, Ha JK, Kim YJ, Jang WH. Lateral positioning for proximal femoral nailing of the intertrochanteric fracture: surgical technique. J Korean Fract Soc. 2011; 24:79–82.
21. Sonmez MM, Camur S, Erturer E, Ugurlar M, Kara A, Ozturk I. Strategies for proximal femoral nailing of unstable intertrochanteric fractures: lateral decubitus position or traction table. J Am Acad Orthop Surg. 2017; 25:e37–e44. PMID:
28134676.
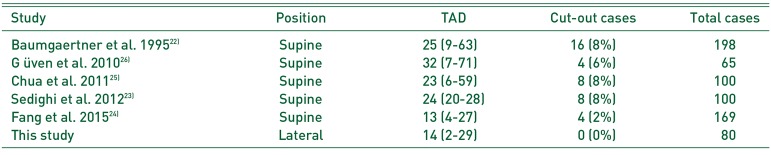
22. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995; 77:1058–1064. PMID:
7608228.

23. Sedighi A, Sales JG, Alavi S. The prognostic value of tipto-apex distance (TAD index) in intertrochanteric fractures fixed by dynamic hip screw. Orthop Rev (Pavia). 2012; 4:e32. PMID:
23589760.

24. Fang C, Lau TW, Wong TM, Lee HL, Leung F. Sliding hip screw versus sliding helical blade for intertrochanteric fractures: a propensity score-matched case control study. Bone Joint J. 2015; 97-B:398–404. PMID:
25737525.
25. Chua YP, Kwan MK, Ng WM, Saw A. Use of the Tip-apex distance in predicting dynamic hip screw cut out in intertrochanteric fracture of the femur in Asian population. Malays Orthop J. 2011; 5:24–27. PMID:
25279032.

26. Güven M, Yavuz U, Kadioğlu B, et al. Importance of screw position in intertrochanteric femoral fractures treated by dynamic hip screw. Orthop Traumatol Surg Res. 2010; 96:21–27. PMID:
20170854.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download