1. Ohata H, Kitauchi S, Yoshimura N, Mugitani K, Iwane M, Nakamura H, et al. Progression of chronic atrophic gastritis associated with
Helicobacter pylori infection increases risk of gastric cancer. Int J Cancer. 2004; 109(1):138–143. PMID:
14735480.
2. Fox JG, Wang TC. Inflammation, atrophy, and gastric cancer. J Clin Invest. 2007; 117(1):60–69. PMID:
17200707.
3. Masuyama H, Yoshitake N, Sasai T, Nakamura T, Masuyama A, Zuiki T, et al. Relationship between the degree of endoscopic atrophy of the gastric mucosa and carcinogenic risk. Digestion. 2015; 91(1):30–36. PMID:
25632914.
4. Kim N, Park YS, Cho SI, Lee HS, Choe G, Kim IW, et al. Prevalence and risk factors of atrophic gastritis and intestinal metaplasia in a Korean population without significant gastroduodenal disease. Helicobacter. 2008; 13(4):245–255. PMID:
18665932.
5. Inoue M, Tajima K, Matsuura A, Suzuki T, Nakamura T, Ohashi K, et al. Severity of chronic atrophic gastritis and subsequent gastric cancer occurrence: a 10-year prospective cohort study in Japan. Cancer Lett. 2000; 161(1):105–112. PMID:
11078919.
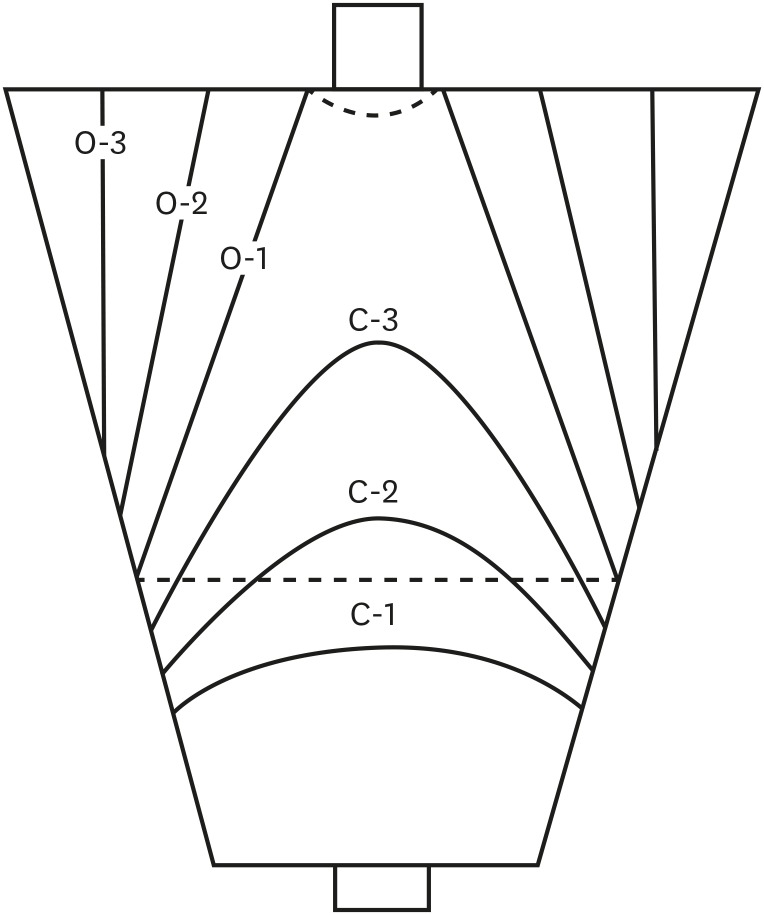
6. Kimura KT, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969; 1(3):87–97.
7. Yoshimura T, Shimoyama T, Fukuda S, Tanaka M, Axon AT, Munakata A. Most gastric cancer occurs on the distal side of the endoscopic atrophic border. Scand J Gastroenterol. 1999; 34(11):1077–1081. PMID:
10582756.
8. Liu Y, Uemura N, Xiao SD, Tytgat GN, Kate FJ. Agreement between endoscopic and histological gastric atrophy scores. J Gastroenterol. 2005; 40(2):123–127. PMID:
15770394.
9. Altman DG. Practical Statistics for Medical Research. London, United Kingdom: Chapman and Hall;1991.
10. Lee SP, Lee SY, Kim JH, Sung IK, Park HS, Shim CS. Link between serum pepsinogen concentrations and upper gastrointestinal endoscopic findings. J Korean Med Sci. 2017; 32(5):796–802. PMID:
28378553.
11. Rugge M, Genta RM. OLGA Group. Staging gastritis: an international proposal. Gastroenterology. 2005; 129(5):1807–1808. PMID:
16285989.
12. Inoue T, Uedo N, Ishihara R, Kawaguchi T, Kawada N, Chatani R, et al. Autofluorescence imaging videoendoscopy in the diagnosis of chronic atrophic fundal gastritis. J Gastroenterol. 2010; 45(1):45–51. PMID:
19876586.
13. Lee JY, Kim N, Lee HS, Oh JC, Kwon YH, Choi YJ, et al. Correlations among endoscopic, histologic and serologic diagnoses for the assessment of atrophic gastritis. J Cancer Prev. 2014; 19(1):47–55. PMID:
25337572.
14. Ricci C, Vakil N, Rugge M, Gatta L, Perna F, Osborn JF, et al. Serological markers for gastric atrophy in asymptomatic patients infected with
Helicobacter pylori
. Am J Gastroenterol. 2004; 99(10):1910–1915. PMID:
15447749.
15. Quach DT, Le HM, Nguyen OT, Nguyen TS, Uemura N. The severity of endoscopic gastric atrophy could help to predict Operative Link on Gastritis Assessment gastritis stage. J Gastroenterol Hepatol. 2011; 26(2):281–285. PMID:
21261717.
16. Ahn SY, Lee SY, Hong SN, Kim JH, Sung IK, Park HS, et al. Endoscopic diagnosis of open-type atrophic gastritis is related to the histological diagnosis of intestinal metaplasia and Cdx2 expression. Dig Dis Sci. 2011; 56(4):1119–1126. PMID:
21221798.
17. Quach DT, Le HM, Hiyama T, Nguyen OT, Nguyen TS, Uemura N. Relationship between endoscopic and histologic gastric atrophy and intestinal metaplasia. Helicobacter. 2013; 18(2):151–157. PMID:
23167960.
18. Weck MN, Brenner H. Prevalence of chronic atrophic gastritis in different parts of the world. Cancer Epidemiol Biomarkers Prev. 2006; 15(6):1083–1094. PMID:
16775164.
19. Kanzaki H, Uedo N, Ishihara R, Nagai K, Matsui F, Ohta T, et al. Comprehensive investigation of areae gastricae pattern in gastric corpus using magnifying narrow band imaging endoscopy in patients with chronic atrophic fundic gastritis. Helicobacter. 2012; 17(3):224–231. PMID:
22515361.
20. Redéen S, Petersson F, Jönsson KA, Borch K. Relationship of gastroscopic features to histological findings in gastritis and
Helicobacter pylori infection in a general population sample. Endoscopy. 2003; 35(11):946–950. PMID:
14606018.
21. Watanabe K, Nagata N, Shimbo T, Nakashima R, Furuhata E, Sakurai T, et al. Accuracy of endoscopic diagnosis of
Helicobacter pylori infection according to level of endoscopic experience and the effect of training. BMC Gastroenterol. 2013; 13:128. PMID:
23947684.
22. Hyun YS, Han DS, Bae JH, Park HS, Eun CS. Interobserver variability and accuracy of high-definition endoscopic diagnosis for gastric intestinal metaplasia among experienced and inexperienced endoscopists. J Korean Med Sci. 2013; 28(5):744–749. PMID:
23678267.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download